Abstract
Aim
To evaluate the intra- and inter-examiner reliability in the assessment of probing depth (PD) measurements at healthy dental implant sites and periodontally healthy natural teeth.
Materials and methods
Five patients exhibiting 21 dental implants were enrolled in the study. Eight experienced examiners performed duplicate PD measurements at six sites of all implants and of preselected natural teeth. Intra-examiner accuracy was estimated using intra-examiner correlation coefficients (ICCs) with 95% confidence intervals (CI). A gold standard (GS) examiner was set. Inter-examiner accuracy compared to the GS examiner was assessed using pairwise inter-examiner ICCs.
Results
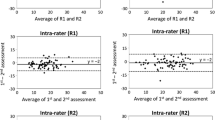
The intra-examiner ICC ranged from 0.759 (95% CI, 0.692–0.812) to 0.863 (95% CI, 0.826–0.892) for the measurements at teeth and from 0.712 (95% CI, 0.580–0.800) to 0.841 (95% CI, 0.774–0.888) for the PDs assessed at implants. The inter-examiner ICCs for tooth measurements varied from 0.197 (95% CI, − 0.280 to 0.511) to 0.791 (95% CI, 0.560–0.892). The corresponding values for the assessments at implants varied from 0.576 (95% CI, 0.286–0.734) to 0.794 (95% CI, 0.708–0.855).
Conclusions
The intra- and inter-examiner reproducibility of repeated PD measurements assessed by experienced examiners tended to be higher for the measurements at periodontally healthy teeth compared to healthy dental implant sites.
Clinical relevance
Experienced examiners demonstrated a higher degree of reliability of probing measurements around teeth compared to dental implants.




Similar content being viewed by others
References
Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, Figuero E, Giovannoli JL, Goldstein M, Lambert F, Ortiz-Vigon A, Polyzois I, Salvi GE, Schwarz F, Serino G, Tomasi C, Zitzmann N (2015) Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol 42(16):S152–S157
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E, Hämmerle CHF, Heitz-Mayfield LJA, Huynh-Ba G, Iacono V, Koo KT, Lambert F, McCauley L, Quirynen M, Renvert S, Salvi GE, Schwarz F, Tarnow D, Tomasi C, Wang HL, Zitzmann N (2018) Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 45(20):S286-s291
Araujo MG, Lindhe J (2018) Peri-implant health. J Clin Periodontol 45:S230–S236
Monje A, Caballé-Serrano J, Nart J, Peñarrocha D, Wang HL, Rakic M (2018) Diagnostic accuracy of clinical parameters to monitor peri-implant conditions: a matched case-control study. J Periodontol 89(4):407–417
Serino G, Turri A, Lang NP (2013) Probing at implants with peri-implantitis and its relation to clinical peri-implant bone loss. Clin Oral Implants Res 24(1):91–95
Gerber JA, Tan WC, Balmer TE, Salvi GE, Lang NP (2009) Bleeding on probing and pocket probing depth in relation to probing pressure and mucosal health around oral implants. Clin Oral Implants Res 20(1):75–78
García-García M, Mir-Mari J, Figueiredo R, Valmaseda-Castellón E (2021) Probing single-tooth dental implants with and without prostheses: a cross-sectional study comparing healthy and peri-implant mucositis sites. J Clin Periodontol 48(4):581–589
Fuchigami K, Munakata M, Kitazume T, Tachikawa N, Kasugai S, Kuroda S (2017) A diversity of peri-implant mucosal thickness by site. Clin Oral Implants Res 28(2):171–176
Badersten A, Nilvéus R, Egelberg J (1984) Reproducibility of probing attachment level measurements. J Clin Periodontol 11(7):475–485
Glavind L, Löe H (1967) Errors in the clinical assessment of periodontal destruction. J Periodontal Res 2(3):180–184
Grossi SG, Dunford RG, Ho A, Koch G, Machtei EE, Genco RJ (1996) Sources of error for periodontal probing measurements. J Periodontal Res 31(5):330–336
Eickholz P, Grotkamp FL, Steveling H, Mühling J, Staehle HJ (2001) Reproducibility of peri-implant probing using a force-controlled probe. Clin Oral Implants Res 12(2):153–158
Ringeling J, Parvini P, Weinbach C, Nentwig GH, Nickles K, Eickholz P (2016) Discomfort/pain due to pocket probing at teeth and endosseous implants: a cross-sectional study. Clin Oral Implants Res 27(8):1005–1009
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, Lijmer LG, Moher D, Rennie D, de Vet HCW, Kressel HY, Rifai N, Golub RM, Altman DG, Hooft L, Korevaar DA, Cohen JF (2015) STARD group STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 351:h5527
Chapple ILC, Mealey BL, Van Dyke TE, Bartold PM, Dommisch H, Eickholz P, Geisinger ML, Genco RJ, Glogauer M, Goldstein M, Griffin TJ, Holmstrup P, Johnson GK, Kapila Y, Lang NP, Meyle J, Murakami S, Plemons J, Romito GA, Shapira L, Tatakis DN, Teughels W, Trombelli L, WalterC WG, Xenoudi P, Yoshie H (2018) Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(1):S74-s84
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, Sculean A, Tonetti MS (2020) EFP Workshop Participants and Methodological Consultants Treatment of stage I-III periodontitis—the EFP S3 level clinical practice guideline. J Clin Periodontol 47(22):4–60
Yi Y, Koo KT, Schwarz F, Amara HB, Heo SJ (2020) Association of prosthetic features and peri-implantitis: a cross-sectional study. J Clin Periodontol 47(3):392–403
Hasturk H, Cugini M (2014) Examiner standardization and calibration for oral and periodontal regenerative studies. In Osteology guidelines for oral and maxillofacial regeneration clinical research. Osteology Foundation, Quintessence Publishing. 97-120
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163
StataCorp., Stata statistical software (2021) release 17. College Station TX: StataCorp LLC
Mombelli A, Mühle T, Brägger U, Lang NP, Bürgin WB (1997) Comparison of periodontal and peri-implant probing by depth-force pattern analysis. Clin Oral Implants Res 8(6):448–454
Di Gianfilippo R, Askar H, Henderson J, Franceschi D, Wang HL, Wang CW (2021) Intra- and inter-examiner repeatability of diagnostic peri-implant clinical measurement: a pilot study. J Oral Implantol. https://doi.org/10.1563/aaid-joi-D-20-00160
Merli M, Bernardelli F, Giulianelli E, Toselli I, Moscatelli M, Pagliaro U, Nieri M (2014) Inter-rater agreement in the diagnosis of mucositis and peri-implantitis. J Clin Periodontol 41(9):927–933
Ramanauskaite A, Becker K, Schwarz F (2018) Clinical characteristics of peri-implant mucositis and peri-implantitis. Clin Oral Implants Res 29(6):551–556
Romandini M, Berglundh J, Derks J, Sanz M, Berglundh T (2021) Diagnosis of peri-implantitis in the absence of baseline data: a diagnostic accuracy study. Clin Oral Implants Res 32(3):297–313. https://doi.org/10.1111/clr.13700
Chu SJ, Kan JYK, Lee EA, Lin GH, Jahangiri L, Nevins M, Wang HL (2019) Restorative emergence profile for single-tooth implants in healthy periodontal patients: clinical guidelines and decision-making strategies. Int J Periodontics Restorative Dent 40(1):19–29
Bauman GR, Mills M, Rapley JW, Hallmon WH (1992) Clinical parameters of evaluation during implant maintenance. Int J Oral Maxillofac Implants 7(2):220–227
Katafuchi M, Weinstein BF, Leroux BG, Chen YW, Daubert DM (2018) Restoration contour is a risk indicator for peri-implantitis: a cross-sectional radiographic analysis. J Clin Periodontol 45(2):225–232
Vierron E, Giraudeau B (2009) Design effect in multicenter studies: gain or loss of power? BMC Med Res Methodo 9:39
Harden M, Friede T (2018) Sample size calculation in multi-centre clinical trials. BMC Med Res Methodol 18(1):156
Garnick JJ, Silverstein L (2000) Periodontal probing: probe tip diameter. J Periodontol 71(1):96–103
Lindhe J, Meyle J (2008) Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35(8):282–285
Lang NP, Berglundh T (2011) Periimplant diseases: where are we now?—Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 38(11):178–181
Al Shayeb KN, Turner W, Gillam DG (2014) Accuracy and reproducibility of probe forces during simulated periodontal pocket depth measurements. Saudi Dent J 26(2):50–55
Seabra RC, Costa FO, Costa JE, Van Dyke T, Soares RV (2008) Impact of clinical experience on the accuracy of probing depth measurements. Quintessence Int 39(7):559–565
Funding
This work was realized within the research project “PeriPLas” funded by the German Ministry of Education and Research (grant numbers: 13N14478, 13N14479, and 13N14480).
Author information
Authors and Affiliations
Contributions
A.R: data analysis, original draft preparation, writing, review, and editing; K.O: conceptualization and original draft preparation; F.S: conceptualization, methodology, resources, writing, review, and editing; K.J: conceptualization, methodology, investigation, writing, review, editing, and supervision; R.C: investigation; J.B: investigation; A.K.E: investigation; J.S: investigation; C.F: investigation; C.E: project administration; T.K: conceptualization, methodology, investigation, writing, review, editing, supervision, project administration, and funding acquisition; L.J: conceptualization, methodology, investigation; S.J: methodology, writing, review, and editing; B.H: conceptualization, methodology, software, validation, data analysis, data curation, writing, review, editing, supervision, visualization, and project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The protocol has been approved by the Ethics Committee of Universitätsklinikum Bonn (102/21-MPG).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramanauskaite, A., Obreja, K., Schwarz, F. et al. Reliability of probing depth assessments at healthy implant sites and natural teeth. Clin Oral Invest 27, 2533–2545 (2023). https://doi.org/10.1007/s00784-022-04810-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04810-5