Abstract
Objectives
The inhibition of bone destruction is one of the main goals of periodontitis treatment. The aim of this study was to investigate the protective effects of non-thermal atmospheric plasma (NTAP) on alveolar bone loss radiographically, histomorphometrically, and histologically in experimental periodontitis in rats.
Materials and methods
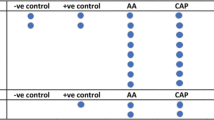
A total of twenty-eight rats were randomly divided into three groups: control group (CG) (n = 8), periodontitis group (PG) (n = 10), and NTAP group (NTAPG) (n = 10). In PG and NTAPG, experimental periodontitis was created with ligating. The kINPen 11 plasma jet was applied around the ligatured teeth in NTAPG. The samples from each group were radiographically assessed with microcomputed tomography (micro-CT); then, histological (presence of osteoclasts and inflammatory cells) and immunohistochemical (immunoreactive of OCN and ALP) findings were compared.
Results
The results revealed a significant increase in alveolar bone loss in the PG compared with CG and NTAPG (p < 0.05). Inflammation, alveolar resorption, and cement damage were reduced significantly in the group treated with NTAP compared to the PG (p < 0.05). Significantly higher levels of osteoclasts were detected in the PG in comparison with both CG and NTAPG (p < 0.05). The lowest osteocalcin and ALP values were determined in PG, and the differences between PG and both groups were also significant (p < 0.05).
Conclusion
Within the limitations of the present study, we can say that NTAP may enhance the bone remodeling process by inhibiting inflammation and preventing alveolar bone destruction.
Clinical relevance
NTAP has clinical potential for accelerating and treating periodontitis with the inflammatory response modulation, osteoblast differentiation, and alveolar bone loss reduction.





Similar content being viewed by others

References
Berglundh T, Donati M (2005) Aspects of adaptive host response in periodontitis. J Clin Periodontol 32:87–107
Curtis MA, Diaz PI, Van Dyke TE (2020) The role of the microbiota in periodontal disease. Periodontol 2020 83:14–25
Joseph S, Curtis MA (2021) Microbial transitions from health to disease. Periodontology 2000 86:201–209
Hathaway-Schrader JD, Novince CM (2021) Maintaining homeostatic control of periodontal bone tissue. Periodontol 2000 86:157–187
Hashimi SM (2019) Exogenous noggin binds the BMP-2 receptor and induces alkaline phosphatase activity in osteoblasts. J Cell Biochem 120:13237–13242
Qin D, Zhang H, Zhang H, Sun T, Zhao H, Lee WH (2019) Anti-osteoporosis effects of osteoking via reducing reactive oxygen species. J Ethnopharmacol 244:112045
Khan SA, Kong EF, Meiller TF, Jabra-Rizk MA (2015) Periodontal diseases: bug induced, host promoted. PLoS Pathog 11(7):e1004952
Sanz-Sanchez I, Ortiz-Vigon A, Herrera D, Sanz M (2016) Microbiological effects and recolonization patterns after adjunctive subgingival debridement with Er:YAG laser. Clin Oral Invest 20:1253–1261
Assem NZ, Alves MLF, Lopes AB, Gualberto Junior EC, Garcia VG, Theodoro LH (2017) Antibiotic therapy as an adjunct to scaling and root planing in smokers: a systematic review and meta-analysis. Braz Oral Res 31:e67
Jepsen K, Jepsen S (2016) Antibiotics/antimicrobials: systemic and local administration in the therapy of mild to moderately advanced periodontitis. Periodontol 2000 71:82–112
Scholtz V, Pazlarova J, Souskova H, Khun J, Julak J (2015) Nonthermal plasma—a tool for decontamination and disinfection. Biotechnol Adv 33:1108–1119
Bekeschus S, Schmidt A, Weltmann KD, von Woedtke T (2016) The plasma jet kINPen–a powerful tool for wound healing. Clin Plasma Med 4:19–28
Choi BBR, Choi JH, Ji J, Song KW, Lee HJ, Kim GC (2018) Increment of growth factors in mouse skin treated with non-thermal plasma. Int J Med Sci 15:1203
De Lima V, Bezerra MM, de Menezes Alencar VB, Daniel Portela Vidal F, Da Rocha FAC, de Castro Brito GA, de Albuquerque RR (2000) Effects of chlorpromazine on alveolar bone loss in experimental periodontal disease in rats. Eur J Oral Sci 108:123–129
Socransky SS, Haffajee AD (1992) The bacterial etiology of destructive periodontal disease: current concepts. J Periodontol 63:322–331
Albandar JM (2000) (2002) Global risk factors and risk indicators for periodontal diseases. Periodontol 29:177–206
Isbary G, Morfill G, Schmidt HU, Georgi M, Ramrath K, Heinlin J, Karrer S, Landthaler M, Shimizu T, Steffes B, Bunk W, Monetti R, Zimmermann JL, Pompl R, Stolz W (2010) A first prospective randomized controlled trial to decrease bacterial load using cold atmospheric argon plasma on chronic wounds in patients. Br J Dermatol 163:78–82
Koban I, Jablonowski L, Kramer A, Weltmann KD, Kocher T (2012) Medical plasma in dentistry: a future therapy for peri-implantitis. In: Machala Z, Hensel K, Akishev Y (eds) Plasma for bio-decontamination, medicine and food security. NATO Science for Peace and Security Series A: Chemistry and Biology. Springer, Dordrecht, pp 191–200
Von Woedtke T, Reuter S, Masur K, Weltmann KD (2013) Plasmas for medicine. Phys Rep 530:291–320
Graves DB (2012) The emerging role of reactive oxygen and nitrogen species in redox biology and some implications for plasma applications to medicine and biology. J Phys D Appl Phys 45:263001
Duchesne C, Banzet S, Lataillade J, Rousseau A, Frescaline N (2019) Cold atmospheric plasma modulates endothelial nitric oxide synthase signalling and enhances burn wound neovascularisation. J Pathol 249:368–380
Arndt S, Unger P, Berneburg M, Bosserhoff AK, Karrer S (2018) Cold atmospheric plasma (CAP) activates angiogenesis-related molecules in skin keratinocytes, fibroblasts and endothelial cells and improves wound angiogenesis in an autocrine and paracrine mode. J Dermatol Sci 89:181–190
Roy J, Galano JM, Durand T, Le Guennec JY, Lee JCY (2017) Physiological role of reactive oxygen species as promoters of natural defenses. FASEB J 31:3729–3745
Boeckmann L, Schäfer M, Bernhardt T, Semmler ML, Jung O, Ojak G, Fischer T, Peters K, Nebe B, Müller-Hilke B, Seebauer C, Bekeschus S, Emmert S (2020) Cold atmospheric pressure plasma in wound healing and cancer treatment. Appl Sci 10:6898
Tominami K, Kanetaka H, Sasaki S, Mokudai T, Kaneko T, Niwano Y (2017) Cold atmospheric plasma enhances osteoblast differentiation. PLoS One 12:e0180507
Seibel MJ (2000) Molecular markers of bone turnover: biochemical, technical and analytical aspects. Osteoporos Int 11:18–29
Lian JB, Gundberg CM (1988) Osteocaicin: biochemical considerations and clinical applications. Clin Orthop Relat Res 226:267–291
Delmas RD (1991) What do we know about biochemical bone markers? Baillieres Clin Obstet Gynaecol 5:817–830
Coleman JE (1992) Structure and mechanism of alkaline phosphatase. Annu Rev Biophys Biomol Struct 21:441–483
Eggers B, Marciniak J, Memmert S, Kramer FJ, Deschner J, Nokhbehsaim M (2020) The beneficial effect of cold atmospheric plasma on parameters of molecules and cell function involved in wound healing in human osteoblast-like cells in vitro. Odontology 108:1–10
Han I, Choi EH (2017) The role of non-thermal atmospheric pressure biocompatible plasma in the differentiation of osteoblastic precursor cells, MC3T3-E1. Oncotarget 8:36399
Yumoto H, Hirao K, Tominaga T, Bando N, Takahashi K, Matsuo T (2015) Electromagnetic wave irradiation promotes osteoblastic cell proliferation and up-regulates growth factors via activation of the ERK1/2 and p38 MAPK pathways. Cell Physiol Biochem 35:601–615
Hirose Y (1995) Effect of pulsing electromagnetic fields on the proliferation and differentiation of osteoblast-like cells. Studies on using immunohistochemical and histochemical staining techniques. J Jpn Prosehodont Soc 39:159–164
Lee DE, Kim JH, Choi SH, Cha JH, Bak EJ, Yoo YJ (2015) Periodontitis mainly increases osteoclast formation via enhancing the differentiation of quiescent osteoclast precursors into osteoclasts. J Per Res 50:256–264
Przekora A, Pawlat J, Terebun P, Duday D, Canal C, Hermans S, Audemar M, Labay C, Thomann JS, Ginalska G (2019) The effect of low temperature atmospheric nitrogen plasma on MC3T3-E1 preosteoblast proliferation and differentiation in vitro. J Phys D Appl Phys 52:275401
Kwon JS, Kim YH, Choi EH, Kim KN (2013) The effects of non-thermal atmospheric pressure plasma jet on attachment of osteoblast. Curr Appl Phys 13:42–47
Knight ET, Liu J, Seymour GJ, Faggion CM Jr (2000) Cullinan MP (2016) Risk factors that may modify the innate and adaptive immune responses in periodontal diseases. Periodontol 71:22–51
Reynolds MA (2014) Modifiable risk factors in periodontitis: at the intersection of aging and disease. Periodontol 2000 64:7–19
Li Q, Valerio MS, Kirkwood KL (2012) MAPK usage in periodontal disease progression. J Signal Transduct 2012:308943
Amini MR, Hosseini MS, Fatollah S, Mirpour S, Ghoranneviss M, Larijani B, Mohajeri-Tehrani MR, Khorramizadeh MR (2020) Beneficial effects of cold atmospheric plasma on inflammatory phase of diabetic foot ulcers; a randomized clinical trial. J Diabetes Metab Disord 19:1–11
Küçük D, Savran L, Ercan UK, Yarali ZB, Karaman O, Kantarci A, Saglam M, Köseoğlu S (2020) Evaluation of efficacy of non-thermal atmospheric pressure plasma in treatment of periodontitis: a randomized controlled clinical trial. Clin Oral Investig 24:3133–3145
Zhang Y, Xiong Y, Xie P, Ao X, Zheng Z, Dong X, Li H, Yu Q, Zhu Z, Chen M, Chen W (2018) Non-thermal plasma reduces periodontitis-induced alveolar bone loss in rats. Biochem Biophys Res Commun 503:2040–2046
Gupta R, Galgali SR, Bavle RM, Chandavarkar V (2013) Evaluation of thickness of cementum of periodontally diseased teeth of non-diabetic and type 2 diabetic patients: a scanning electron microscopy study. J Indian Soc Periodontol 17:592–596
Bilgin E, Gurgan CA, Arpak MN, Bostanci HS, Guven K (2004) Morphological changes in diseased cementum layers: a scanning electron microscopy study. Calcif Tissue Int 74:476–785
Bartold PM, McCulloch CAG, Narayanan AS (2000) Pitaru S (2000) Tissue engineering: a new paradigm for periodontal regeneration based on molecular and cell biology. Periodontol 24:253–269
Han G, Nguyen LN, Macherla C, Chi Y, Friedman JM, Nosanchuk JD, Martinez LR (2012) Nitric oxide–releasing nanoparticles accelerate wound healing by promoting fibroblast migration and collagen deposition. Am J Pathol 180:1465–1473
Oz HS, Puleo DA (2011) Animal models for periodontal disease. BioMed Res Int 2011:754857
Klausen B (1991) Microbiological and immunological aspects of experimental periodontal disease in rats: a review article. J Periodontol 62:59–73
Toker H, Ozan F, Ozer H, Ozdemir H, Eren K, Yeler H (2008) A morphometric and histopathologic evaluation of the effects of propolis on alveolar bone loss in experimental periodontitis in rats. J Periodontol 79:1089–1094
Misch KA, Yi ES, Sarment DP (2006) Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol 77:1261–1266
Alpan AL, Çalisir M, Kizildag A, Özdede M, Özmen Ö (2020) Effects of a glycogen synthase kinase 3 inhibitor tideglusib on bone regeneration with calvarial defects. J Craniofac Surg 31:1477–1482
Nicolielo LFP, Van Dessel J, Shaheen E, Letelier C, Codari M, Politis C, Lambrichts I, Jacobs R (2017) Validation of a novel imaging approach using multi-slice CT and cone-beam CT to follow-up on condylar remodeling after bimaxillary surgery. Int J Oral Sci 9:139–144
Kulah K, Gulsahi A, Kamburoğlu K, Geneci F, Ocak M, Celik HH, Ozen T (2019) Evaluation of maxillary trabecular microstructure as an indicator of implant stability by using 2 cone beam computed tomography systems and micro-computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 127:247–256
Jungbauer G, Moser D, Müller S, Pfister W, Sculean A, Eick S (2021) The antimicrobial effect of cold atmospheric plasma against dental pathogens—a systematic review of in-vitro studies. Antibiotics 10:211
Menezes M, Prado M, Gomes B, Gusman H, Simao R (2016) Effect of photodynamic therapy and non-thermal plasma on root canal filling: analysis of adhesion and sealer penetration. J Appl Oral Sci 25:396–403
Funding
This study was supported by the Scientific Research Project Coordination Center of Eskisehir Osmangazi University in Eskisehir, Turkey (grant number 2019-2479).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The experimental protocol and design were performed in accordance with guidelines laid down by the National Institutes of Health in the USA regarding the care and use of animals for experimental procedures or with the European Communities Council Directive (2010/63/EU) and approved by the Animal Research Ethics Committee of Eskisehir Osmangazi University (Protocol No. 661–1/2019). The study protocol and manuscript were created according to the “NC3Rs ARRIVE Guidelines, Animal Research: Reporting of in Vivo Experiments.”
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kusakcı-Seker, B., Ozdemir, H. & Karadeniz-Saygili, S. Evaluation of the protective effects of non-thermal atmospheric plasma on alveolar bone loss in experimental periodontitis. Clin Oral Invest 25, 6949–6959 (2021). https://doi.org/10.1007/s00784-021-04203-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04203-0