Abstract
Objective
To identify the microbiome in sockets with alveolar osteitis and compare it with a control group using metagenomic techniques.
Materials and methods
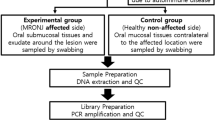
A case-control study was conducted in subjects that had undergone a tooth extraction. Microbiological samples were taken from the sockets of 10 patients with dry socket after tooth extraction (AO group) and 10 patients in whom exodontia resulted in no postoperative complications (control group). Bacterial DNA was isolated, and the 16S rRNA gene was amplified and sequenced. Multiplexed tag-encoded sequencing of DNA from the samples was performed, and the reads were processed by Metagenomic Rapid Annotation.
Results
A total of 151 different species were found: 55 bacteria were only found in the AO group, 51 were specific to the control group, and 45 were common to both groups. The most frequently found genera in both groups were Prevotella. Prevotella nanceiensis, Actinomyces odontolyticus, Treponema maltophilum, Veillonella dispar, Tannerella forsythia, and Leuconostoc mesenteroides were found in several patients with alveolar osteitis, with an abundance greater than 0.5%, and were absent in all the control group samples.
Conclusions
Patients who develop alveolar osteitis after dental extractions might have a different microbiota from that of patients without postoperative complications. Since this is a preliminary report, further research is needed to assess whether bacteria play an important role in the etiology of dry socket.
Clinical relevance
This study seems to indicate that bacteria may play an important role in the alveolar osteitis etiology. Thus, new prevention and treatment strategies should be considered.


Similar content being viewed by others
References
Vezeau PJ (2000) Dental extraction wound management: medicating postextraction sockets. J Oral Maxillofac Surg 58:531–537
Blum IR (2002) Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg 31:309–317
Noroozi AR, Philbert RF (2009) Modern concepts in understanding and management of the “dry socket” syndrome: comprehensive review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:30–35
Alexander RE (2000) Dental extraction wound management: a case against medicating postextraction sockets. J Oral Maxillofac Surg 58:538–551
Nitzan D, Sperry JF, Wilkins TD (1978) Fibrinolytic activity of oral anaerobic bacteria. Arch Oral Biol 23:465–470
Nitzan DW (1983) On the genesis of “dry socket”. J Oral Maxillofac Surg 41:706–710
Brescó-Salinas M, Costa-Riu N, Berini-Aytés L, Gay-Escoda C (2006) Antibiotic susceptibility of the bacteria causing odontogenic infections. Med Oral Patol Oral Cir Bucal 11:70–75
Poeschl PW, Spusta L, Russmueller G, Seemann R, Hirschl A, Poeschl E, Klug C, Ewers R (2010) Antibiotic susceptibility and resistance of the odontogenic microbiological spectrum and its clinical impact on severe deep space head and neck infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110:151–156
Peñarrocha M, Sanchis JM, Sáez U, Gay C, Bagán JV (2001) Oral higiene and postoperative pain after mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92:260–264
Hedström L, Sjögren P (2007) Effect estimates and methodological quality of randomized controlled trials about prevention of alveolar osteitis following tooth extraction: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103:8–15
Laird WR, Stenhouse D, MacFarlane TW (1972) Control of postoperative infection. A comparative evaluation of clindamycin and phenoxymethylpenicillin. Br Dent J 133:106–109
Larsen PE (1991) The effect of chlorhexidine rinse on the incidence of alveolar osteitis following the surgical removal of implacted third molars. J Oral Maxillofac Surg 49:932–937
Haraji A, Rakhshan V, Khamverdi N, Alishahi HK (2013) Effects of intra-alveolar placement of 0.2% chlorhexidine bioadhesive gel on dry socket incidence and postsurgical pain: a double-blind split-mouth randomized controlled clinical trial. J Orofac Pain 27:256–262
Human Oral Microbiome Database (HOMD) c2007–2018 Cambridge (MA): The Forsyth Institute; Accessed April 2016. http://www.homd.org/
Kilian M, Chapple IL, Hannig M et al (2016) The oral microbiome—an update for oral healthcare professionals. Br Dent J 221:657–666
Zarco MF, Vess TJ, Ginsburg GS (2012) The oral microbiome in health and disease and the potential impact on personalized dental medicine. Oral Dis 18:109–120
ASA Physical Status Classification System (2014) Washington DC: American Society of Anesthesiologists; [updated October 15 2014; Accessed April 20 2017] http://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system
Group JCHMPDGWG. 16S 454 Sequencing Protocol HMP Consortium (2010) Available at: http://www.hmpdacc.org/doc/16S_Sequencing_SOP_4.2.2.pdf. Accessed 25 Jan 2016
Schmieder R, Edwards R (2011) Quality control and preprocessing of metagenomic datasets. Bioinformatics 27:863–864
Meyer F, Paarmann D, D'Souza M, Olson R, Glass EM, Kubal M, Paczian T, Rodriguez A, Stevens R, Wilke A, Wilkening J, Edwards RA (2008) The metagenomics RAST server—a public resource for the automatic phylogenetic and functional analysis of metagenomes. BMC Bioinformatics 9:386–394
Gomez-Alvarez V, Teal TK, Schmidt TM (2009) Systematic artifacts in metagenomes from complex microbial communities. ISME J 3:1314–1317
Wang Q, Garrity GM, Tiedje JM, Cole JR (2007) Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol 73:5261–5267
Futami R, Muñoz-Pomer L, Viu JM, Domínguez-Escribá L, Covelli L, Bernet GP, Sempere JM, Moya A, Llorens C (2011) GPRO: the professional tool for annotation, management and functional analysis of omic databases. Biotech Bioinform 2011-SOFT3 1:1–5
OSU CORE database, Oral microbiome. Available at: http://microbiome.osu.edu/sequences. Accessed 21 Nov 2016
Charalampakis G, Belibasakis GN (2015) Microbiome of peri-implant infections: lessons from conventional, molecular and metagenomic analyses. Virulence 6:183–187
Cortés-Acha B, Figueiredo R, Seminago R, Roig FJ, Llorens C, Valmaseda-Castellón E (2017) Microbiota analysis of biofilms on experimental abutments mimicking denal implants: an in vivo model. J Periodontol 88:1090–1104
Bienek DR, Filliben JJ (2016) Risk assessment and sensitivity meta-analysis of alveolar osteitis occurrence in oral contraceptive users. J Am Dent Assoc 147:394–404
Taberner-Vallverdú M, Sánchez-Garcés MÁ, Gay-Escoda C (2017) Efficacy of different methods used for dry socket prevention and risk factor analysis: a systematic review. Med Oral Patol Oral Cir Bucal 22:e750–e758
Rodríguez Sánchez F, Rodríguez Andrés C, Arteagoitia Calvo I (2017) Does chlorhexidine prevent alveolar osteitis after third molar extractions? Systematic review and meta-analysis. J Oral Maxillofac Surg 75:901–914
Ramos E, Santamaría J, Santamaría G, Barbier L, Arteagoitia I (2016) Do systemic antibiotics prevent dry socket and infection after third molar extraction? A systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 122:403–425
Lodi G, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S (2012) Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst Rev 11:CD003811
Serrati S, Margheri F, Bruschi S et al (2006) Plasminogen activators and inhibitor type-1 in alveolar osteitis. Eur J Oral Sci 114:500–503
Seo ES, Lee JH, Park JY, Kim D, Han HJ, Robyt JF (2005) Enzymatic synthesis and anti-coagulant effect of salicin analogs by using the Leuconostoc mesenteroides glucansucrase acceptor reaction. J Biotechnol 117:31–38
Ates O (2015) Systems biology of microbial exopolysaccharides production. Front Bioeng Biotechnol 3:200
Acknowledgements
The authors would like to thank Mary Georgina Hardinge for English language editing of the manuscript and to Dr. Carlos Noguera for help with collecting the samples.
Funding
The present research was partially funded (4000€) with a postgraduate research grant from the Faculty of Dentistry of the University of Barcelona.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Rui Figueiredo reports grants from the Faculty of Dentistry—University of Barcelona during the conduct of the study. He also reports grants, personal fees, and non-financial support from Mozo-Grau (Valladolid, Spain), grants from Mundipharma Research (Cambridge, UK), personal fees from BioHorizons Ibérica (Madrid, Spain), Inibsa Dental (Lliça de Vall, Spain), Dentsply implants Iberia (Barcelona, Spain), and Araguaney Dental (Barcelona, Spain) outside the submitted work. Dr. Eduard Valmaseda-Castellón reports grants from the Faculty of Dentistry—University of Barcelona during the conduct of the study. He also reports grants, personal fees, and non-financial support from MozoGrau, personal fees from BioHorizons Ibérica, personal fees from Inibsa Dental, and personal fees from Dentsply implants Iberia outside the submitted work. Dr. Laura Aguilar-Durán, Dr. Ramón Seminago, Dr. Carlos Llorens, and Dr. Francisco J. Roig report grants from the Faculty of Dentistry—University of Barcelona to conduct the present study. The authors declare no other conflicts of interest regarding this study. The present research was conducted by the Dental and Maxillofacial Pathology and Therapeutics Research Group at the IDIBELL Institute and was funded by a postgraduate research grant from the Faculty of Dentistry of the University of Barcelona (4000€).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its latter amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aguilar-Durán, L., Figueiredo, R., Seminago, R. et al. A metagenomic study of patients with alveolar osteitis after tooth extraction. A preliminary case-control study. Clin Oral Invest 23, 4163–4172 (2019). https://doi.org/10.1007/s00784-019-02855-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02855-7