Abstract
Objectives
Compression screws that can fix a fracture of the condylar head of the mandible are available. Although typical titanium lag screws are generally used, a series of headless screws have been designed for this purpose. The “headless” advantage derived from the complete submergence of the screw in the bone after fixation is the lack of irritation of the lateral ligament of the temporo-mandibular joint by the screw head. The aim of this study is to compare the compression force of typically used lag screws with that of newly developed headless compression screws.
Materials and methods
This study tested five types of screws with a 14-mm length: 10 2.0-mm lag screws and 40 headless screws (four groups of equal size: 1.5-mm H screws, 1.8-mm H screws, 2.0-mm H screws, and 1.8-mm W screws). Two cuboid blocks of standardized polyurethane foam were fixed by one screw. The maximal compression force (F in N) and torque at maximal compression force (T in Ncm) were tested according to the guidelines of the American Society for Testing and Materials (ASTM F1839-08).
Results
The test results were as follows: 2.0-mm lag screw: F = 211.5 ± 20.7 and T = 21.1 ± 1.6; 1.5-mm H screw: F = 47.2 ± 5.6 and T = 18.2 ± 1.1; 1.8-mm H screw: F = 95.5 ± 9.8 and T = 18.2 ± 1.1; 2.0-mm H screw: F = 145.1 ± 18.4 and T = 25.5 ± 1.5; and 1.8-mm W screw: F = 180.5 ± 8.7 and T = 26.4 ± 2.8. Each type of screw significantly differed from one another as far as compression forces (F) were considered (p < 0.05): the best is the lag screw contrary to the thinnest H screw which is the worst one. For all tested screws, the compression force depended on the torque (S curve relationship was revealed, p < 0.05) and screw diameter (a larger diameter yielded greater compression, p < 0.05).
Conclusions
The 8-mm headless screws featured only a small loss of compression ability compared to the titanium lag screws.
Clinical relevance
Headless screws are mechanically attractive fixation materials for condylar head fracture treatment.
Similar content being viewed by others
Introduction
Surgical management of mandibular head fractures has rapidly progressed in recent years, thanks to improvement in diagnostics [1], including accurate classification and imaging by cone beam tomography, as well as advances in surgical procedures and the development of new surgical materials. On one hand, the treatment principles are constant: reduction and fixation. However, on the other hand, nowadays, surgeon has raspators with working surface covered by diamonds for improved friction tool-bone to facilitate bone-reducing maneuvers. Rigid mandibular head fixation is safer and easier due to application of lower profile screws, i.e., less than 2 mm, and compressive screws, i.e., causing a strong pressure on the bone surface during the initial healing period. Fractures to the condylar head of the mandible can be treated with long screws (i.e., lag screws, full-threaded screws). Although the standard diameter of titanium screws is 2.0 mm, low-profile screws can bear [2] occlusal loading (200 N for 1.7-mm screws and 150 N for 1.2-mm screws) and can be efficiently used to achieve functionally stable and atraumatic osteosynthesis [3].
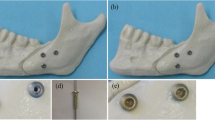
Although the lag screw has a high compressive capability, its screw head protrudes over the bone level after fixation (Fig. 1 a and b). This protrusion can cause problems and lead to bone resorption [4, 5]. To solve this problem, a headless compression screw was created [6]. However, this screw had a lower compression strength than the lag screw. Therefore, a new modified headless compression screw was developed. The author believes that these modifications merge the advantages of both screws, including high compression force and total bone immersion. Different modifications of a screw with the same diameter and length result in variable anchorage in the bone [7]. Which modification yields the highest compression force during fixation? The aim of this study was to compare the compression force of known lag screws with that of modified headless compression screws.
Clinical application of the evaluated screws. Open rigid internal fixation of the condyle head of the mandible. a, b Examples of 2.0-mm lag screw application (note the screw head protrudes above the bone surface what can irritates lateral ligament and cause bone resorption). c, d Own design of the 1.5-mm Herbert screw (completely submerged within the bone). e, f Own design of the 1.8 Weil’s osteotomy-like screw (completely submerged within the bone)
Materials and methods
Two types of recently designed and manufactured headless screws (H screw and W screw) were used in the test (Fig. 1, Table 1). Fifty screws were tested and divided into equal 10-sample groups. All screws had a length of 14 mm. The H screw is a modified version of Herbert’s screw, which exhibits now a self-drilling tip, no cannulation, and a low profile (1.5-mm screw: shaft diameter 1.1 mm, trailing thread diameter 2.1 mm; 1.8-mm screw: shaft diameter 1.4 mm, trailing thread diameter 2.4 mm; 2.0-mm screw: shaft diameter 1.6 mm, trailing thread diameter 2.6 mm). The W screw was developed based on the performance of screws applied for Weil osteotomy, which is an oblique osteotomy of the metatarsal head and neck. The osteotomy line is similar to that of a type C condylar head fracture according to Neff’s classification. Own designed W screw had a leading thread diameter of 1.8 mm (self-tapping), a shaft diameter of 1.1 mm, and a gradually widened trailing thread with a maximal external diameter of 3.2 mm. The leading threads in H and W screws were 5 mm in length. Thus, the experimental groups were organized by screw type. Each group consisted of 10 screws. The control group included the self-tapping lag screw with a length of 14 mm (leading thread, 8-mm length), shaft diameter of 2.0 mm, and head diameter of 2.6 mm.
The high variability in the density and the elastic modulus of cancellous bone affects biomechanical testing results [8]. Synthetic foam materials have been shown to produce less intra- and interspecimen variability than cadaver bone [9]. A foam block has consistent material properties, similar to the human cancellous bone. Solid polyurethane foam is widely used as an ideal medium to mimic human cancellous bone and has been confirmed by the American Society for Testing and Materials [10] as a standard material for testing orthopedic devices and instruments. In this study, polyurethane foam (Sawbones, Vashon, WA, USA: density 0.16 g/cc, compression modulus 58 MPa) was used as a substitute for osteoporotic cancellous bone [11,12,13,14].
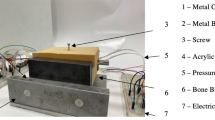
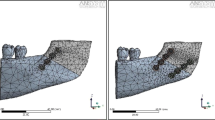
An experimental station was constructed (Fig. 2) to compare the compression force and screw torque in polyurethane blocks. The compression force and torque at maximal compression force were recorded simultaneously. Data were collected at a frequency of 10 Hz with a Forsentek FC10 detector (Shenzhen, China) to measure the compression force and a dynamometric screwdriver to measure torque (Imada Cedar DIS-TW20, Brooklyn, New York, USA). The test blocks were prepared of polyurethane foam of 40 pcf density (according to ASTM F1839). The force detector was calibrated in a range from 0 to 500 N using a dynamic test instrument (Instron ElectroPuls E3000, Darmstadt, Germany). Fifty screws were tested. The statistical analysis was performed using Statgraphics Centurion XVI (Statpoint, The Plains, Virginia, USA). Compression force and torque results were evaluated with a Kruskal-Wallis test due to between-group variance alterations. The same evaluation was also used for screw diameter analysis. Simple regression was applied to identify a relationship between compression force and torque. A p value less than 0.05 was considered significant.
Results
The observed compression forces and moment of the force in maximal compression (torque) are shown in Table 1 and Figs. 3 and 4. According to the Kruskal-Wallis test, the compression force was significantly different according to the screw type (test statistic, 46; p < 0.001). Although the torque was significantly different based on screw type (test statistic, 42, p < 0.001), comparison of the headless 1.8 × 14 H screw versus the headless 1.5 × 14 H screw and the headless 1.8 × 14 W screw versus the headless 2.0 × 14 H screw demonstrated identical torque at maximal compression force.
The effects of screw diameter on compression force and torque at maximal compression force are presented in Figs. 5 and 6. The maximal compression force was 178.3 ± 39.0 N for 2.0-mm screws; 138.0 ± 44.5 N for 1.8-mm screws, and 47.2 ± 5.6 N for 1.5-mm screws (significantly different by diameter; test statistic, 28; p < 0.001). Among all screws tested, the torque was lowest (test statistic, 14; p < 0.001) in 1.5-mm screws (18.2 ± 1.1 Ncm). The torque was 22.3 ± 4.7 Ncm in all 1.8-mm screws and 23.3 ± 2.7 Ncm in all 2.0-mm screws; no significant difference was found among these screws.
For all tested screws, regression analysis indicated (Fig. 4) a moderately strong relationship between the compression force and torque (R2 = 45; correlation coefficient (cc) = 0.67; p < 0.001). When the effects of screw type were evaluated, compression was only related to torque in the headless 1.8 × 14 W screw (R2 = 47; cc = 0.68; p < 0.05, Fig. 7) and showed a trend towards significance in the headless 1.5 × 14 H screw (R2 = 34; cc = 0.58; p = 0.08). No relationship was found for the other three groups.
Discussion
Screw stability and compression rate is obviously dependent on an insertion protocol. The main issue is proper drilling. The canal in the proximal (deeper) bone fragment must be significantly narrower than the external diameter of the threads in the screw top (leading thread). Thanks to this, the top of the screw can evoke a compression force to both bone fragments. And that is why, in this experiment, the author used a significantly narrower drill than external diameter of screw leading thread (Table 1). Optimally, the screw should be perpendicular to the fracture plane in clinical application of the insertion protocol. To release the full compression capacity, gliding drilling of the distal (superficial) bone fragment is recommended [15]. The double drilling in the preauricular region is sometimes a challenging procedure. The gradual increase in diameter of the drill or step diameter drills (only single drilling for screw is enough) are facilitation and solution of that difficulty.
The second issue is the type of the screw. The cancellous and cortical screws are available nowadays, but only that previous one are proper to mandibular head compressive fixation. The deep leading threads are essential in the screw design. Only a deep anchorage in proximal fragment cancellous bone ensures the compressive capacity [16].
The third issue is the kind of bone in which the screw is immersed. It is well known [17] that cancellous bone served lower pullout strength and lower screw stability. Unfortunately, there is no possibility to slide along the cortical wall nor bicortical stabilization in mandible head orthopedic surgery. Two reasons explained these limits: (1) tiny and restrained periosteum elevation prevents avascular osteonecrosis but narrows the field of view for drilling navigation and (2) through-and-through penetration of the mandibular head irritates of TMJ ligaments on the medial pole or affects articular surface, but such screwing increases the stability of compressed bone fragments.
The screw presented in this paper was developed as a modification of the screw designed by Timothy James Herbert. The present screw was easier to install due to the elimination of the internal canal but was still able to achieve compression fixation. The second advantage of this screw was the lack of a classical head, such as in the lag screw, without a high loss of compression. Due to the lack of a screw head, more room is available for surgical maneuvers in the limited condylar region. Furthermore, bone compression by the screw head is known to cause fracture or resorption of the outer layer of the cortex [4]. However, until now, the large diameter of the screw relative to the condyle made accurate alignment difficult. When the screw is used, countersinking is not necessary because the screw head engages inside the bone. Moreover, gliding canal preparation and K-wire manipulation are also unnecessary. The effect of the depth of the headless 14-mm screw in the condylar head is similar to that of a 15–16-mm lag screw due to the complete submersion of the new screw in the bone.
The reduced diameter (1.5 mm), lack of a protrusive head (H and W screws), threads that engage both fragments, and short leading threads for fixation of a small proximal segment are excellent concepts for fixing typical A head fractures [18]. This screw would be most ideal for type A and B condylar head fracture fixation due to its perpendicular insertion (to the bone surface), leading to regular immersion of the screw end in cortical bone. Of the two types of fractures, type A is most applicable for this screw because of the amount of bone in the two bone segments, which ensures the possibility of compressive fixation. However, its use with a type C fracture would also be possible [3]. Moreover, stable fixation is easy because the screw is inserted perpendicular to the fracture line. Oblique insertion, which may be necessary in type C fractures, may require deeper screw immersion if the osteosynthesis material is added below the bone level or in the case of conversion to plate fixation [19].
The threadless central shaft screw design (all screws investigated in this study) is biomechanically preferable to the fully threaded variable pitch screw design because it achieves higher or identical compression forces at different interfragmentary gaps with similar stiffness and loads, even though the threadless central shaft screws show a greater loss of compression force over time [20]. The compression force generated by a screw is thought to be an important factor in facilitating union by reducing the fracture gap and improving fracture surface interdigitation, thereby promoting primary bone healing and increasing rotational and bending stability [11, 21,22,23,24,25].
A strong compression force increases the contact area between bone fragments. What does the lowest compression force (47 N) found in this experiment mean? Koh et al. [20] observed the following forces in a scaphoid bone model: 21 N (Acutrac screw), 28 N (Herbert-Whipple screw), and 45 N (HCS 3.0 screw). Therefore, the interfragmentary compression force observed in this study seems appropriate because forces of 100–200 N were detected for 1.8- and 2.0-mm screws.
Interestingly, the analysis of all 50 tested screws revealed a relationship between torque in maximal compression force and compression force. In particular, H screws produced bone fragment compression that was not dependent on the amount of screw tightening. This can be explained by the phenomenon described by Herbert [4]. The number of turns determines the compression (not torque) due to the different pitches of the threads in both ends of the screw. However, the W screw is designed as a compound lag screw with H screw construction. The top is a typical H screw, but on the end, it expands similar to the head of a lag screw. This makes the compression dependent on the torque as the end of the W screw begins to merge into the cortical bone. Subsequently, increasing the torque does not produce any increase in the compression force. Therefore, the compression force remains constant and strong (Fig. 7).
Performed tests confirmed that lag screws have the highest compression capacity. Due to their headless designs, the H or W screws can be non-irritating options for open reduction and rigid fixation of the condylar head. However, they exhibit a difference in maximal compression force. All compression forces seemed sufficient for condylar head fracture fixation, but some applications may require the use of a guiding jig or positioning plate [26] to hold the fragments together during insertion of the screw and to align the instruments. Without that initial compression, shrinkage of the fracture line may not be sufficient when the smallest H screw is applied. This problem disappears in the case of the headless 1.8 × 14 W screw. The compression force is approximately similar to that of the 2.0/8 × 14 lag screw, but it has a lower profile (1.8- versus 2.0-mm system and 1.1- versus 2.0-mm shaft), with no protruding head above the bone level after fixation. This screw even allows for the application of three screws per condyle head, which improves interfragmentary compression.
This study had some limitations. Although the mechanical properties of the synthetic bones were similar to those of human cancellous bone, some differences were present in the structure of the materials. Specifically, synthetic bones have an almost uniform pore size, whereas human cancellous bone has a complex anatomical texture. This can affect the compression efficacy and fastening torque of the screws. The results of this study were based on a single-density synthetic bone; however, the biomechanical performance of the screws changes with the bone density environment [13]. The tests were conducted on synthetic bones with a perfect fracture gap simulated by parallel planes. Only specific types of fractures, types A and B, of the condyle head were simulated. These simulations were required to perform replicable and reliable testing. Finally, most screw loosening cases can be attributed to physiological cyclic loading during biting. Further evaluation of interfragmentary compression that simulates the cyclic loading of screws under physiological situations is necessary.
In conclusion, although the headless construction of the screws led to decreased compression force generated by the screw, the observed values were still sufficient for interfragmentary compression. This study confirmed the advantage of a non-irritant screw construction that exhibited only a small loss of compression ability.
References
Kozakiewicz M (2019) Classification proposal for fractures of the processus condylaris mandibulae. Clin Oral Investig 23:485–491
Neff A, Mühlberger G, Karoglan M, Kolk A, Mittelmeier W, Scheruhn D, Horch HH, Kock S, Schieferstein H (2004) Stabilitat der Osteosynthese bei Gelenkwalzenfrakturen in Klinik und biomechanischer Simulation. Mund Kiefer Gesichtschir 8:63–74
Kozakiewicz M, Świniarski J (2017) Treatment of high fracture of the neck of the mandibular condylar process by rigid fixation performed by lag screws: finite element analysis. Dent Med Probl 54:223–228
Herbert TJ, Fisher WE (1984) Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br 66:114–123
Kolk A, Neff A (2015) Long-term results of ORIF of condylar head fractures of the mandible: a prospective 5-year follow-up study of small-fragment positional-screw osteosynthesis (SFPSO). J Craniomaxillofac Surg 43:452–461
Kozakiewicz M (2018) Small diameter compression screw, completely submerged within bone, for rigid internal fixation of the condylar head of the mandible. Br J Oral Maxillofac Surg 56:74–76
Kozakiewicz M, Sołtysiak P (2017) Pullout force comparison of selected screws for rigid fixation in maxillofacial surgery. Dent Med Probl 54:129–133
Goldstein SA (1987) The mechanical properties of trabecular bone: dependence on anatomic location and function. J Biomech 20:1055–1061
Chapman JR, Harrington RM, Lee KM, Anderson PA, Tencer AF, Kowalski D (1996) Factors affecting the pullout strength of cancellous bone screws. J Biomech Eng 118:391–398
ASTM F1839-08 (2012) Standard specification for rigid polyurethane foam for use as a standard material for testing orthopaedic devices and instruments. Am Soc Test Mater
Assari S, Darvish K, Ilyas AM (2012) Biomechanical analysis of second-generation headless compression screws. Injury 43:1159–1165
Baran O, Sagol E, Oflaz H, Sarikanat M, Havitcioglu H (2009) A biomechanical study on preloaded compression effect on headless screws. Arch Orthop Trauma Surg 129:1601–1605
Ramaswamy R, Evans S, Kosashvili Y (2010) Holding power of variable pitch screws in osteoporotic, osteopenic and normal bone: are all screws created equal? Injury 41:179–183
Bailey C, Kuiper J, Kelly C (2006) Biomechanical evaluation of a new composite bioresorbable screw. J Hand Surg Br 31:208–212
Krenkel C (1992) Axial ‘anchor’ screw (lag screw with biconcave washer) or ‘slanted-screw’ plate for osteosynthesis of fractures of the mandibular condylar process. J Craniomaxillofac Surg 20:348–353
Park JW, Kim KT, Sung JK, Park SH, Seong KW, Cho DC (2017) Biomechanical comparison of inter-fragmentary compression pressures: lag screw versus Herbert screw for anterior odontoid screw fixation. J Korean Neurosurg Soc 60:498–503
Ueno M, Sakai R, Tanaka K, Inoue G, Uchida K, Imura T, Saito W, Nakazawa T, Takahira N, Mabuchi K, Takaso M (2015) Should we use cortical bone screws for cortical bone trajectory? J Neurosurg Spine 22:416–421
Neff A, Kolk A, Neff F, Horch HH (2002) Surgical vs. conservative therapy of diacapitular and high condylar fractures with dislocation. A comparison between MRI and axiography. Mund Kiefer Gesichtschir 6:66–73
Kozakiewicz M, Świniarski J (2017) Finite element analysis of new introduced plates for mandibular condyle neck fracture treatment by open reduction and rigid fixation. Den Med Probl 54:319–326
Koh IH, Kang HJ, Kim JS, Park SJ, Choi YR (2015) A central threadless shaft screw is better than a fully threaded variable pitch screw for unstable scaphoid nonunion: a biomechanical study. Injury 46:638–642
Beadel GP, Ferreira L, Johnson JA, King GJ (2004) Interfragmentary compression across a simulated scaphoid fracture—analysis of 3 screws. J Hand Surg Am 29:273–278
Gardner AW, Yew YT, Neo PY, Lau CC, Tay SC (2012) Interfragmentary compression profile of 4 headless bone screws: an analysis of the compression lost on reinsertion. J Hand Surg Am 37:1845–1851
Gruszka DS, Burkhart KJ, Nowak TE, Achenbach T, Rommens PM, Muller LP (2012) The durability of the intrascaphoid compression of headless compression screws: in vitro study. J Hand Surg Am 37:1142–1150
Rankin G, Kuschner SH, Orlando C, McKellop H, Brien WW, Sherman RA (1991) Biomechanical evaluation of a cannulated compressive screw for use in fractures of the scaphoid. J Hand Surg Am 16:1002–1010
Toby EB, Butler TE, McCormack TJ, Jayaraman G (1997) A comparison of fixation screws for the scaphoid during application of cyclical bending loads. J Bone Joint Surg Am 79:1190–1197
Neff A, Kolk A, Meschke F, Deppe H, Horch HH (2005) Kleinfragmentschrauben vs. Plattenosteosynthese bei Gelenkwalzenfrakturen Vergleich funktioneller Ergebnisse mit MRT und Achsiographie. Mund Kiefer GesichtsChir 9:80–88
Acknowledgements
The author would like to thank ChM (www.chm.eu) for their support of the study.
Funding
This study was financially supported by the Medical University of Lodz (grant nos. 1.503/5-061-02/503-51-001 and 1.503/5-061-02/503-51-002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study complies with the principles stated in the Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects,” adopted by the 18th World Medical Assembly, Helsinki, Finland, June 1964, and as amended most recently by the 64th World Medical Assembly, Fontaleza, Brazil, October 2013.
Conflict of interest
The author declares that they have no conflicts of interest.
Ethical approval
For this type of study, formal ethical approval is not required.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kozakiewicz, M. Comparison of compression screws used for mandible head fracture treatment—experimental study. Clin Oral Invest 23, 4059–4066 (2019). https://doi.org/10.1007/s00784-019-02842-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02842-y