Abstract
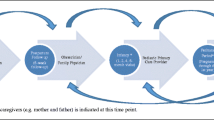
Perinatal mood instability (MI) is a common clinical observation in perinatal women, and existing research indicates that MI is strongly associated with a variety of mental disorders. The purpose of this study is to review the evidence of perinatal MI systematically, with a focus on perinatal MI, its relation to perinatal depression, and its effects on children. A systematic search of the literature using PRISMA guidelines was conducted on seven academic health databases to identify any peer-reviewed articles published in English from 1985 to July 2017. Studies were screened, data were extracted, and quality of the selected studies was assessed. A total of 1927 abstracts were returned from the search, with 1063 remaining for abstract screening after duplicate removal, and 4 quantitative studies were selected for final analysis. The selected studies addressed perinatal MI (n = 2), the relation of perinatal MI to perinatal depression (n = 1), and the effects of perinatal MI on children (n = 1). The selected studies identified that perinatal women experienced a significantly higher level of MI than non-perinatal women, MI is a prominent feature in perinatal women with and without depression, mood lability during the early postpartum predicts psychopathology up to 14 months postpartum, and maternal emotion dysregulation, rather than maternal psychopathology, increases the risk of heightened facial affect synchrony in mother-infant interaction. The study reveals a significant gap in the literature of perinatal MI.

Similar content being viewed by others
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing, Washington, DC
Anestis MD, Selby EA, Crosby RD, Wonderlich SA, Engel SG, Joiner TE (2010) A comparison of retrospective self-report versus ecological momentary assessment measures of affective lability in the examination of its relationship with bulimic symptomatology. Behav Res Ther 48(7):607–613
Beatson JA, Rao S (2013) Depression and borderline personality disorder. Med J Aust 199:S24–S27
Beebe B, Jaffe J, Buck K, Chen H, Cohen P, Feldstein S, Andrews H (2008) Six-week postpartum maternal depressive symptoms and 4-month mother–infant self-and interactive contingency. Infant Ment Health J 29(5):442–471
Bell M, Bayliss D, Glauert R, Harrison A, Ohan J (2018) Children of parents who have been hospitalised with psychiatric disorders are at risk of poor school readiness. Epidemiol Psychiatr Sci:1–13
Berle J, Mykletun A, Daltveit AK, Rasmussen S, Holsten F, Dahl AA (2005) Neonatal outcomes in offspring of women with anxiety and depression during pregnancy. Arch Womens Ment Health 8(3):181–189
Bernieri FJ, Rosenthal R (1991) Interpersonal coordination: behavior matching and interactional synchrony. Cambridge University Press, New York
Bloch M, Daly RC, Rubinow DR (2003) Endocrine factors in the etiology of postpartum depression. Compr Psychiatry 44(3):234–246
Bornstein MH, Manian N (2013) Maternal responsiveness and sensitivity reconsidered: some is more. Dev Psychopathol 25(4pt1):957–971
Bowen R, Baetz M, Hawke J, Bowen A (2006) Mood variability in anxiety disorders. J Affect Disord 91(2):165–170
Bowen R, Baetz M, Leuschen C, Wagner J, Pierson R (2011) Predictors of suicidal thoughts: mood instability versus neuroticism. Personal Individ Differ 51:1034–1038
Bowen A, Bowen R, Balbuena L, Muhajarine N (2012) Are pregnant and postpartum women moodier? Understanding perinatal mood instability. J Obstet Gynaecol Can 34(11):1038–1042
Bowen R, Wang Y, Balbuena L, Houmphan A, Baetz M (2013) The relationship between mood instability and depression: implications for studying and treating depression. Med Hypotheses 81:459–462
Bridges LJ, Grolnick WS (1995) The development of emotional self-regulation in infancy and early childhood. Soc Dev 15:185–211
Broome MR, He Z, Iftikhar M, Eyden J, Marwaha S (2015a) Neurobiological and behavioural studies of affective instability in clinical populations: a systematic review. Neurosci Biobehav Rev 51:243–254
Broome MR, Saunders K, Harrison P, Marwaha S (2015b) Mood instability: significance, definition and measurement. Brit J Psychiat 207(4):283–285
Calkins SD (1994) Origins and outcomes of individual differences in emotion regulation. Monogr Soc Res Child Dev 59(2–3):53–72
Calkins SD, Leerkes EM (2004) Early attachment processes and the development of emotional self-regulation. In: Baumeist, Vohs (eds) Handbook of self-regulation: research, theory, and applications, 2nd edn. Guilford Press, New York, pp 324–339
Cassidy J (1994) Emotion regulation: influences of attachment relationships. Monogr Soc Res Child Dev 59(2–3):228–249
Chang L, Schwartz D, Dodge KA, McBride-Chang C (2003) Harsh parenting in relation to child emotion regulation and aggression. J Fam Psycho 17(4):598–606
Chmielowska M, Fuhr DC (2017) Intimate partner violence and mental ill health among global populations of indigenous women: a systematic review. Soc Psychiatry Psychiatr Epidemiol 52(6):689–704
Cole PM, Martin SE, Dennis TA (2004) Emotion regulation as a scientific construct: methodological challenges and directions for child development research. Child Dev 75(2):317–333
Crawford JR, Henry JD (2004) The Positive and Negative Affect Schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 43(3):245–265
Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spong C (2010) Williams obstetrics, vol 872, 23rd edn. McGraw Hill, New York
Dayan J, Creveuil C, Herlicoviez M, Herbel C, Baranger E, Savoye C, Thouin A (2002) Role of anxiety and depression in the onset of spontaneous preterm labor. Am J Epidemiol 155(4):293–301
Ebner-Priemer UW, Kuo J, Schlotz W, Kleindienst N et al (2008) Distress and affective dysregulation in patients with borderline personality disorder: a psychophysiological ambulatory monitoring study. J Nerv Ment Dis 196(4):314–320
Ehring T, Fischer S, Schnülle J, Bösterling A, Tuschen-Caffier B (2008) Characteristics of emotion regulation in recovered depressed versus never depressed individuals. Personal Individ Differ 44(7):1574–1584
Faber J, Fonseca LM (2014) How sample size influences research outcomes. Dental Press J Orthod 19(4):27–29
Faurholt-Jepsen M, Ritz C, Frost M, Mikkelsen RL, Christensen EM, Bardram J, Vinberg M, Kessing LV (2015) Mood instability in bipolar disorder type I versus type II-continuous daily electronic self-monitoring of illness activity using smartphones. J Affect Disord 186:342–349
Field T (2010) Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev 33(1):1–6
Fredrickson BL (2000) Extracting meaning from past affective experiences: the importance of peaks, ends, and specific emotions. Cognit Emot 14:577–606
Fried EI, Nesse RM, Guille C, Sen S (2015) The differential influence of life stress on individual symptoms of depression. Acta Psychiatr Scand 131:465–471
Gaudreau P, Sanchez X, Blondin JP (2006) Positive and negative affective states in a performance-related setting: testing the factorial structure of the PANAS across two samples of French-Canadian participants. Eur J Psychol Assess 22(4):240–249
Glover V, Kammerer M (2004) The biology and pathophysiology of peripartum psychiatric disorders. Prim Psychiatry 3:37–41
Glover V, O’Connor T, O’Donnell K (2010) Prenatal stress and the programming of the HPA axis. Neurosci Biobehav Rev 35(1):17–22
Gratz KL, Roemer L (2004) Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 26(1):41–54
Hapgood CC, Elkind GS, Wright JJ (1988) Maternity blues: phenomena and relationship to later post partum depression. Aust N Z J Psychiatry 22(3):299–306
Henshaw C (2003) Mood disturbance in the early puerperium: a review. Arch Womens Ment Health 6(2):s33–s42
Jaffe J, Beebe B, Feldstein S, Crown CL, Jasnow MD, Rochat P, Stern DN (2001) Rhythms of dialogue in infancy: coordinated timing in development. Monogr Soc Res Child Dev 66(2):i-viii+1-149
Jahng S, Wood PK, Trull TJ (2008) Analysis of affective instability in ecological momentary assessment: indices using successive difference and group comparison via multilevel modeling. Psychol Methods 13(4):354
Joober R, Schmitz N, Annable L, Boksa P (2012) Publication bias: what are the challenges and can they be overcome? J Psychiatry Neurosci 37(3):149–152
Kessler RC, Berglund P, Demler O et al (2003) The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). Jama 289(23):3095–3105
Koenigsberg HW (2010) Affective instability: toward an integration of neuroscience and psychological perspectives. J Personal Disord 24(1):60–82
Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, Silverman JM, Serby M, Schopick F, Siever L (2002) Characterizing affective instability in borderline personality disorder. Am J Psychiatry 159:784–788
Li D, Liu L, Odouli R (2008) Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: a prospective cohort study. Hum Reprod 24(1):146–153
Links PS, Eynan R, Heisel MJ, Nisenbaum R (2008) Elements of affective instability associated with suicidal behaviour in patients with borderline personality disorder. Can J Psychiatr 53(2):112–116
Lotzin A, Schiborr J, Barkmann C, Romer G, Ramsauer B (2016) Maternal emotion dysregulation is related to heightened mother–infant synchrony of facial affect. Dev Psychopathol 28(2):327–339
Martinez-Torteya C, Dayton CJ, Beeghly M et al (2014) Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Dev Psychopathol 26(2):379–392
Marwaha S, Parsons N, Flanagan S, Broome M (2013) The prevalence and clinical associations of mood instability in adults living in England: results from the Adult Psychiatric Morbidity Survey 2007. Psychiatry Res 205:262–268
Marwaha S, He Z, Broome M, Singh S, Scott J, Eyden J, Wolke D (2014) How is affective instability defined and measured? A systematic review. Psychol Med 44(09):1793–1808
Marwaha S, Balbuena L, Winsper C, Bowen R (2015) Mood instability as a precursor to depressive illness: a prospective and mediational analysis. Aust N Z J Psychiatry 30:557–565
McLaughlin KA, Mennin DS, Farach F (2007) The contributory role of worry in emotion generation and dysregulation in generalized anxiety disorder. Behav Res Ther 45(8):1735–1752
Meie LL, Orth U, Denissen JJ, Kühnel A (2011) Age differences in instability, contingency, and level of self-esteem across the life span. J Res Pers 45(6):604–612
Miller J, Pilkonis PA (2006) Neuroticism and affective instability: the same or different? Am J Psychiatry 163(5):839–845
Miller DJ, Vachon DD, Lynam DR (2009) Neuroticism, negative affect, and negative affect instability: establishing convergent and discriminant validity using ecological momentary assessment. Personal Individ Differ 47(8):873–877
Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma-Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J (2009) Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med 39(9):1533–1547
Nelson AM (2003) Transition to motherhood. J Obstet Gynecol Neonatal Nurs 32(4):465–477
O’Hara MW, McCabe JE (2013) Postpartum depression: current status and future directions. Annu Rew Clin Psychol 9:379–407
O'Hara MW, Wisner KL (2014) Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynecol 28(1):3–12
Ostir GV, Smith PM, Smith D, Ottenbacher KJ (2005) Reliability of the Positive and Negative Affect Schedule (PANAS) in medical rehabilitation. Clin Rehabil 19(7):767–769
Patel R, Lloyd T, Jackson R et al (2015) Mood instability is a common feature of mental health disorders and is associated with poor clinical outcomes. BMJ Open 5(5):e007504
Porter CL, Hsu HC (2003) First-time mothers’ perceptions of efficacy during the transition to motherhood: links to infant temperament. J Fam Psychol 17(1):54–65
Quilty LC, Sellbom M, Tackett JL, Bagby RM (2009) Personality trait predictors of bipolar disorder symptoms. Psychiatry Res 169:159–163
Rossell SL, Nobre AC (2004) Semantic priming of different affective categories. Emotion 4(4):354–363
Rossi V, Pourtois G (2012) Transient state-dependent fluctuations in anxiety measured using STAI, POMS, PANAS or VAS: a comparative review. Anxiety Stress Coping 25(6):603–645
Schoenleber M, Berghoff CR, Tull MT, DiLillo D, Messman-Moore T, Gratz KL (2016) Emotional lability and affective synchrony in borderline personality disorder. Personal Disord 7(3):211–220
Schuch FB, Vancampfort D, Sui X et al (2016) Are lower levels of cardiorespiratory fitness associated with incident depression? A systematic review of prospective cohort studies. Prev Med 93:159–165
Schwartz CE, Rapkin BD (2004) Reconsidering the psychometrics of quality of life assessment in light of response shift and appraisal. Health Qual Life Outcomes https://hqlo.biomedcentral.com/track/pdf/10.1186/1477-7525-2-16. Accessed 08 October 2017
Spinrad TL, Stifter CA (2002) Maternal sensitivity and infant emotional reactivity: concurrent and longitudinal relations. Marriage Fam Rev 34(3–4):243–263
Thompson RA (2001) Childhood anxiety disorders from the perspective of emotion regulation. In: Vasey, Dadds (eds) The developmental psychopathology of anxiety, 1st edn. Oxford University Press, Oxford, pp 160–182
Thompson RA, Calkins SD (1996) The double-edged sword: emotional regulation for children at risk. Dev Psychopathol 8(1):163–182
Thompson RJ, Berenbaum H, Bredemeier K (2011) Cross-sectional and longitudinal relations between affective instability and depression. J Affect Disord 130(1):53–59
Tronick E, Als H, Adamson L, Wise S, Brazelton TB (1978) The infant's response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child psychiatry 17(1):1–13
Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, Watson D (2008) Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. J Abnorm Psychol 117(3):647–661
Tull MT, Roemer L (2007) Emotion regulation difficulties associated with the experience of uncued panic attacks: evidence of experiential avoidance, emotional nonacceptance, and decreased emotional clarity. Behav Ther 38(4):378–391
Watson D, Clark LA, Tellegen A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54(6):1063–1070
Weibel S, Micoulaud-Franchi JA, Brandejsky L et al (2017) Psychometric properties and factor structure of the short form of the Affective Lability Scale in adult patients with ADHD. J Atten Disord. https://doi.org/10.1177/1087054717690808
Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, Tugwell P (2016) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute, Ottawa, ON
Wilkinson RB (1999) Mood changes in mothers and fathers through childbearing: are the blues so blue? Psychol Health 14(5):847–858
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This systematic review included studies that involved human participants.
Informed consent
All reviewed studies obtained informed consent from participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Search strategy
Appendix. Search strategy
Search strategy
Database search
A systematic search for recent literature relevant to perinatal mood instability (MI) was conducted by a health sciences librarian and a PhD student.
List of databases searched
Seven databases were searched: Cumulative Index to Nursing and Allied Health (CINAHL), Cochrane Library (Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials), Embase, PubMed, MEDLINE, PsychINFO, and Scopus.
Research question
What is the state of the literature related to perinatal MI, its relation to perinatal depression, and its effects on children?
Inclusion criteria
The following criteria were used to guide the search:
-
A primary focus of the article is on the topic area: MI in pregnant women or women with a newborn or infant less than 24 months, MI in relation to perinatal mood disturbances, and effects of perinatal MI on children
-
Study methodology limited to all types of primary studies: quantitative, qualitative, mixed methods, and reviews
-
Published between January 1985 and July 2017
-
Published in English
-
Accessible for retrieval
Exclusion criteria
The following criteria were used to exclude literature from the search:
-
Topic not related to perinatal MI or in relation to perinatal MI (e.g., antennal and postpartum depression, and antenatal and postpartum anxiety only).
-
Dissertations, commentaries, narrative, anecdotal articles, letters to the editor, editorials, expert reports, consensus documents, and discussion papers
-
Non-English studies
-
Unpublished (e.g., gray literature)
-
Studies involving animals
-
Articles focusing only on antenatal and postpartum depression, and antenatal and postpartum anxiety
Rights and permissions
About this article
Cite this article
Li, H., Bowen, A., Bowen, R. et al. Mood instability during pregnancy and postpartum: a systematic review. Arch Womens Ment Health 23, 29–41 (2020). https://doi.org/10.1007/s00737-019-00956-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-019-00956-6