Abstract
Hyperemesis gravidarum (HG) is a pregnancy condition characterised by severe nausea and vomiting during early pregnancy. The experience of HG is for many women a traumatic event. Few studies have investigated a possible association between HG and birth-related posttraumatic stress. The objective of the current study was to assess whether HG increases the risk of birth-related posttraumatic stress symptoms (PTSS). This was a population-based pregnancy cohort study using data from the Akershus Birth Cohort Study (ABC study). A linear mixed model was used to estimate the association between the degree of nausea (no nausea (n = 574), mild nausea (n = 813), severe nausea (n = 522) and HG (hospitalised due to nausea, n = 20)) and PTSS score at 8 weeks and 2 years after birth. At 8 weeks postpartum, women with HG had higher PTSS scores compared to women with no nausea (p = 0.008), women with mild nausea (p = 0.019) and women with severe nausea (p = 0.027). After 2 years, women with HG had higher PTSS scores compared to women with no nausea (p = 0.038). Women with HG had higher PTSS scores following childbirth compared to women with less pronounced symptoms or no nausea at all. After 2 years, women with HG still had higher PTSS scores compared to women with no nausea. Although the overall differences in PTSS scores were small, the results may still be of clinical relevance.
Similar content being viewed by others
Introduction
Nausea and vomiting in pregnancy affects up to 80% of all pregnancies, predominantly during the first trimester (Gadsby et al. 1993), and is a common cause of sick leave (Dorheim et al. 2013). An estimated 0.3 to 2% of women develop a very severe form, known as hyperemesis gravidarum (HG), which may include metabolic disturbances and nutritional deficiencies (Eliakim et al. 2000; World Health Organization 2004), and therefore lead to hospitalisation (Gazmararian et al. 2002).
The exact cause of HG is not known. However, one of the main hypotheses of today involves the rise of the pregnancy hormone, human chorionic gonadotrophin (hCG), which coincides with the occurrence of HG. Several conditions associated with increased hCG, such as molar pregnancy and multiple gestation, are associated with increased risk of developing HG (Grooten et al. 2015). Another hypothesis involves genetics as HG is inherited along the maternal line (Vikanes et al. 2010a). Moreover, recent, genetic research has identified genes that may increase the risk of HG (Fejzo et al. 2017, 2018). HG has, however, a long history of stigmatisation, being described as the result of hysterical personality traits and psychological disturbances (Fairweather 1968). Despite recent research, women with therapy-resistant HG nevertheless continue to be examined for psychiatric disorders (Kim et al. 2009). A growing body of research has shown an association between HG and maternal depression and anxiety during pregnancy (Mitchell-Jones et al. 2017); however, the causal direction of this association remains elusive (Aksoy et al. 2015; Fell et al. 2006; Kjeldgaard et al. 2017a; Pirimoglu et al. 2010; Seng et al. 2007).
The few studies that have researched psychological distress following pregnancy suggest that HG increases the risk of postpartum depression (Kjeldgaard et al. 2017b) and stress reactions (Christodoulou-Smith et al. 2011; Meltzer-Brody et al. 2017), in particular, for those experiencing prolonged or extreme symptoms (Fejzo et al. 2009; Kjeldgaard et al. 2017b; Mullin et al. 2012). It may therefore be hypothesised that HG could influence the whole pregnancy and birth experience in such a way that it causes posttraumatic stress symptoms (PTSS) following childbirth. A lack of a holistic approach, including psychosocial as well as physical care by midwives, nurses and medical doctors, may worsen the psychological distress of women with HG (Poursharif et al. 2008; Power et al. 2010), further increasing the risk of PTSS (Ayers et al. 2016; Grekin and O'Hara 2014; Reed et al. 2017).
The aim of the present study was to estimate the association between the degree of nausea in pregnancy and birth-related PTSS and whether PTSS change from 8 weeks to 2 years after childbirth.
Methods
Study population
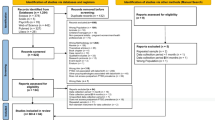
Data were derived from the Norwegian Akershus Birth Cohort (ABC), a large population-based prospective cohort study. Between November 2008 and April 2010, women were recruited at the routine foetal ultrasound examination in pregnancy week 17 (Garthus-Niegel et al. 2014, 2017). There were no exclusion criteria other than inability to complete a questionnaire in Norwegian. Of the 4814 women invited to participate, 4662 women were included in the study (96.8%). Data were collected by self-administered questionnaires in pregnancy weeks 17 (Q1) and 32 (Q2), and 8 weeks (Q3) and 2 years (Q4) after delivery. Q3 was administered 8 weeks following childbirth to ensure that maternity blues (Pop et al. 2015) would not interfere with the assessment of postpartum psychiatric disorders. Q4 was administered 2 years after birth, as the main focus of this questionnaire was to assess mental health in relation to child development. Additional information was obtained by linkage to the electronic birth records. The birth records are completed by the hospital staff and contain socio-demographic and medical information about the mother, child, pregnancy and birth. Some women dropped out of the study due to moving or severe obstetric complications. Figure 1 displays a flow chart of the recruitment and retention for the first three questionnaires, which comprised our baseline study sample. Note that the sample sizes may deviate somewhat from previous publications due to small changes in the latest quality-assured data files released for research.
We included all women who participated in at least the first three questionnaires (n = 1981). Women with multiple pregnancies were excluded (n = 36). The final study sample consisted of 1945 women. An overview of time points for data collection of relevant maternal characteristics is presented in Fig. 2.
All women gave written informed consent. The study was approved by the Regional Committee for Ethics in Medical Research in Norway (approval number S-08013a)
Key variables
The main predictor was the degree of nausea, reported in Q2. The women reported whether they had experienced no, mild or severe nausea, and whether they had been on sick leave or hospitalised due to nausea. We categorised the degree of nausea into four groups: no nausea, mild nausea, severe nausea (including sick leave) and HG (hospitalised due to nausea).
The main outcome was PTSS, measured by the Impact of Event Scale (IES) (Horowitz et al. 1979) in Q3 and Q4. The questions were asked in relation to the birth of the index pregnancy. The IES is a self-rating scale that measures symptoms of intrusion (seven items) and avoidance (eight items). The scale has four response categories (not at all, rarely, sometimes and often), with higher scores reflecting a higher degree of posttraumatic stress. The scale has been validated in postpartum women (Olde et al. 2006), with scores over 19 reflecting clinically significant distress, and scores above 34 indicating probable presence of PTSD (Neal et al. 1994).
Mental health measurements
Symptoms of previous general posttraumatic stress disorder (PTSD) were measured in Q1. The women reported whether they at any time in their lives had been involved in or had experienced a dramatic and terrifying event. If they had, they reported whether they had suffered from any of eight potential symptoms related to that event during the last month. The symptoms were based on the Mini-International Neuropsychiatric Interview (M.I.N.I.), which is designed for epidemiological studies (Sheehan et al. 1998). The measured symptoms were (1) re-experienced the event (e.g., in dreams, nightmares, intense memories or flashbacks), (2) avoided thinking or talking about the event, (3) had problems remembering the event, (4) felt distant, (5) had been considerably disturbed by the event in my work and in social activities, (6) had problems sleeping, (7) had problems concentrating or (8) had been nervous. A score of 1 was given if the symptom was present, resulting in a sumscore ranging from 0 (no symptoms) to 8 (maximum number of symptoms).
Prenatal depression was measured by the Edinburgh Postnatal Depression Scale (EPDS) (Cox et al. 1987) in Q1. The EPDS is a 10-item self-rating scale designed to identify postnatal depression but has also been validated in pregnancy (Cox et al. 1996; Eberhard-Gran et al. 2001; Murray and Cox 1990). Each item is scored from 0 to 3 with higher scores reflecting higher levels of depression. The total score ranges from 0 to 30. Prenatal depression was dichotomised as “yes” and “no” with presence of depression defined as a score > 12.
Anxiety was measured using 10 items from The Hopkins Symptom Check List (SCL-25) (Hesbacher et al. 1980) in Q1. The SCL-25 is a widely used self-rating scale, and the first 10 items comprise the anxiety score (SCL-A). Each item is scored from 0 to 3 with higher scores reflecting higher levels of anxiety. Each item ranges from “not at all” (score 1) to “extremely” (score 4), and the sumscore ranges from 10 to 40. Presence of anxiety was defined as a score ≥ 18.
Subjective birth experience was measured using a numeric rating scale (NRS) 8 weeks after birth. The NRS was based on the question “What was your overall experience of the birth?” The answers were scored from 0 (“very good”) to 10 (“extremely bad”). Negative birth experience was defined as an NRS score ≥ 9.
Socio-demographic and reproductive factors
Parity was obtained from Q1 and dichotomised into primiparity and multiparity. Maternal age and education were obtained from the birth record. Level of education was dichotomised into ≤ 12 years and > 12 years.
Using information on birth complications registered in the birth record, we constructed an index of obstetric complications, which have previously been associated with HG and/or postpartum PTSD, and thus may influence the association between nausea and PTSS. Each potential complication was treated as a dichotomous variable, depending on whether or not it had occurred. As few women had more than one of the included obstetric complications, two categories were created; “no complications” and “1 complication or more”. The complications were the following: (1) preterm birth (< 37 weeks), (2) placental abruption, (3) pre-eclampsia, (4) small for gestational age and (5) low 10-min Apgar score (Bolin et al. 2013; Dodds et al. 2006; Fiaschi et al. 2018; Meltzer-Brody et al. 2017).
Major negative life events during the last 12 months were measured using ten items in Q2. These items were selected from established life event scales (Coddington 1972; Swearingen and Cohen 1985). The life events included were (1) being separated or divorced, (2) serious problems in the marriage or cohabiting relationship (3) problems or conflicts with family members, friends or neighbours, (4) problems at work or in school, (5) economic problems, (6) serious illness or injury, (7) serious illness or injury in the close family, (8) traffic accident, fire or theft, (9) loss of a closely related person and (10) other difficulties. As few women experienced more than one event, major negative life events were dichotomised as “yes” with one or more negative life events present or “no”.
Statistics
Data were described as means and standard deviations (SD) or frequencies and percentages. Missing values on the psychometric scales were imputed if the number of missing items was ≤ 20% per case. The association between PTSS scores assessed at 8 weeks and 2 years after giving birth and the degree of nausea was assessed by a linear mixed model with random intercepts for women, accounting for intra-women correlations. Fixed effects for time point (8 weeks or 2 years), degree of nausea and the interaction between those two were entered. Further, to assess whether possible confounders (parity, maternal age, education, obstetric complications, previous PTSD, prenatal depression, prenatal anxiety, major negative life events) were associated with changes in PTSS over time, the multiple linear mixed model with fixed effects for each characteristic and the interaction between the characteristic and time point were estimated. In order to explore, whether the differences in birth-related PTSS scores were explained by negative birth experience, we performed two models adjusting for co-variates: one multiple model with no adjustment for negative birth experience and one multiple model adjusting for negative birth experience.
Linear mixed modelling handles unbalanced data by including all available information, also from drop-outs.
SAS version 14 was used for data analysis. The results with p values below 0.05 were considered statistically significant.
Data availability
The dataset analysed in the current study is not publicly available due to data privacy restrictions and ethical restrictions established by the Norwegian Regional Committee for Ethics in Medical Research. Data are however available through application to the ABC study. All inquiries about access to data should be sent to the ABC steering group, attention: Nina.Vislokken.Odegard@ahus.no. All requests to access personal data will be handled in accordance with the procedures by the Ethics Committee.
Results
A total of 1945 women were included in the study. The mean age was 31.3 years (range 18.8–45.5 years; SD 4.6 years), and 50% were primiparous. Roughly 70% of the women reported nausea; 42% had mild nausea, nearly 27% had severe nausea and 1% had HG. A total of 72 (3.7%) and 35 (1.8%) women reported birth-related PTSD (PTSS score > 34) 8 weeks and 2 years after birth, respectively. Characteristics of the sample are presented in Table 1.
According to linear mixed model, there were statistically significant differences in PTSS scores according to the degree of nausea. As compared to women without nausea, at 8 weeks after birth, women with severe nausea (p = 0.002) and with HG (0.006) had statistically significantly higher PTSS scores. Women with HG also had statistically significantly higher PTSS scores compared to women with mild nausea (p = 0.023). Two years after birth, only women with severe nausea had statistically significantly higher PTSS scores compared to the scores of women without nausea (p = 0.035).
When adjusted for co-variates (parity, maternal age, education, obstetric complications, previous PTSD, prenatal depression, prenatal anxiety and major negative life events), the results slightly changed. In the model not adjusting for negative birth experience, there were no longer statistically significant differences in PTSS scores between women with mild nausea and women with HG (p = 0.054) 8 weeks postpartum.
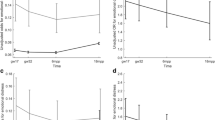
The results changed in the model adjusting for negative birth experience. Higher PTSS was significantly associated with negative birth experience (p < 0.001) at both time points. Eight weeks after giving birth, women with HG had higher PTSS scores compared with women without nausea (p = 0.008), women with mild nausea (p = 0.019) and women with severe nausea (p = 0.027). After 2 years, women with HG only had higher PTSS scores compared with women without nausea (p = 0.038). The main results are listed in Table 2 and presented graphically in Fig. 3.
Regarding co-variates, the following were statistically significantly associated with PTSS at both time points in the unadjusted and the two adjusted model: previous PTSD, parity, prenatal depression and negative life events. Obstetric complications were not associated with PTSS, while level of education (at 8 weeks postpartum) and maternal age (at 8 weeks and 2 years after giving birth) were associated with PTSS in the unadjusted model but not in the adjusted models. Prenatal anxiety was statistically significant associated with PTSS in the unadjusted model but only at 8 weeks in the adjusted models. The results for all included variables are presented in the supplementary table.
Discussion
The main finding of this study was that women with HG reported higher birth-related PTSS scores at 8 weeks postpartum than women who had experienced severe, mild or no nausea. Two years after giving birth, however, women with HG reported higher PTSS scores only when compared with women who had no nausea. The associations remained significant after additional adjustment for negative birth experience.
Our study was based on a longitudinal pregnancy cohort study with the focus on maternal mental health in relation to pregnancy, birth and the period up to 2 years following childbirth. To the best of our knowledge, no previous study has explored the association between the degree of nausea and childbirth-related PTSS. However, available studies show results along the lines of the results of the present study. A Danish register-based study of women with no psychiatric history (Meltzer-Brody et al. 2017) revealed that women with HG had a greater risk of developing acute stress (incidence rate ratio 1.32, 95% CI 1.33–2.55) up to 12 months following childbirth. In an American cross-sectional study utilising service usage data (Seng et al. 2001), women with PTSD were nearly four times more likely to have had HG than women without PTSD (aOR 3.9, 95% CI 2.0–7.4). In contrast to our study, the two studies noted above did not provide information about the specific trauma exposure. Two further studies based on an online survey (Christodoulou-Smith et al. 2011; Fejzo et al. 2009; Mullin et al. 2012) also showed that women with HG were more likely to experience postpartum PTSS. However, the definitions of PTSS were not adequately explained in these studies to render comparison possible.
In order to investigate, whether PTSS would change over time, we estimated the association between the degree of nausea during pregnancy and birth-related PTSS at two time points after birth. Indeed, our results revealed higher PTSS scores among women with HG at both time points compared to those with less severe nausea symptoms. The results also suggest that PTSS levels decrease over time.
As the PTSS score was related to childbirth, we wanted to explore whether differences in scores could be explained by the birth experience, since a negative birth experience has previously been shown to be the most important factor in the development of PTSS following childbirth (Garthus-Niegel et al. 2013). Thus, we estimated two multiple models, one adjusting and one not adjusting for negative birth experiences. Our results revealed that childbirth-related PTSS was strongly associated with negative birth experiences (Supplementary table). After additional adjustment for negative birth experiences in the adjusted model, there were still statistically significant differences in PTSS scores between the HG group and women with no, mild or severe nausea 8 weeks postpartum, suggesting that women with HG have a greater risk of PTSS regardless of their birth experience.
Although the differences in mean scores were small (2–4 points) and all mean scores were far below the scores that may indicate a full PTSD diagnosis (score > 34), we believe that the results may still be of clinical importance. Unfortunately, the nature of the data allowed us to investigate PTSS only 8 weeks and 2 years after birth, thus limiting the interpretation of development in the symptom burden. In future research, it would be interesting to explore whether stress levels among women who suffered from HG increase, when they consider a new pregnancy. When addressing the results of the present study, a few things are important to bear in mind. First, severe, unremitting nausea and vomiting is, for many women, a traumatic experience. The severity of nausea is comparable to that of receiving chemotherapy (Lacroix et al. 2000), and quality of life may decrease to a level comparable to that of women with breast cancer or myocardial infarction (Lacasse et al. 2008). In addition, feelings of isolation and lack of support may put a strain on a partner relationship (Heitmann et al. 2017; Lacasse et al. 2008; Mazzotta et al. 2000; Tan et al. 2017). Furthermore, thoughts of pregnancy termination (Heitmann et al. 2017; Poursharif et al. 2007) or suicidal ideation may arise (Poursharif et al. 2007). If a doctor hesitates to initiate treatment, this may worsen these negative emotions (Grooten et al. 2015; Raymond 2013). Current options of treatment are mainly restricted to symptom relief, such as anti-emetics, rehydration and supplementation of vitamins and nutrients (Grooten et al. 2015).
Our results indicate that HG may influence the whole pregnancy and birth experience in such a way that it increases the risk of PTSS following childbirth. Hence, women with HG may receive better care, if health care providers practice holistically, involving social and psychological care as well as physical interventions. In addition, improved health care and support may prevent women from resorting to either pregnancy termination due to anxiety about being pregnant (Mazzotta et al. 2000; Poursharif et al. 2007; Raymond 2013) or avoidance of future pregnancies (Heitmann et al. 2016; Poursharif et al. 2008).
Strengths and limitations
A major strength of this study is its long-term, prospective data collection, which allowed us to assess PTSS scores 8 weeks and 2 years after childbirth. Self-selection bias may have been present; however, self-selection bias does not necessarily affect the estimated associations (Nilsen et al. 2009). No women were excluded due to other pregnancy complications, thereby reducing the risk of overestimating the association between the degree of nausea and birth-related PTSS. However, generalisability may be limited as only Norwegian-speaking women, mainly Caucasians, were included in the study. The associations may therefore differ in other ethnic groups.
We used instruments designed to measure psychological distress in population-based studies. Questionnaire studies often yield larger study populations compared with studies utilising clinical interviews, though questionnaires cannot be used for clinical diagnosis.
Subjective birth experience was measured retrospectively 2 months postpartum, but should ideally have been measured shortly after delivery. Additionally, the subjective birth experience and PTSS were assessed simultaneously, which may affect the causal direction; however, it seems reasonable to assume that the birth experience would influence the stress response rather than vice versa (Garthus-Niegel et al. 2013). No established and validated instrument such as the Perceptions of Labour and Delivery Scale (Bailham et al. 2004) was used in the present study to measure subjective birth experiences. Use of a more comprehensive and validated measurement instrument might provide further insights into the role of subjective birth experiences in the development of PTSS.
Regarding the definition of HG, the ABC study unfortunately does not include a validated score such as the Pregnancy Unique Quantification of Emesis (PUQE) (Birkeland et al. 2015; Koren et al. 2005). The data provided information about the degree of nausea, sick leave and hospitalisation. In Norway, during the study period, only women with severe metabolic disturbances were admitted to the hospital for HG, and no outpatient treatment was available. However, health care is free of charge in Norway, and all women in need of inpatient treatment are admitted regardless of socioeconomic status. Therefore, in order to restrict our HG group to those with the most severe symptoms, we defined HG as hospitalisation due to nausea. Hospitalisation for HG was assessed retrospectively in pregnancy week 32; however, recall bias is highly unlikely due to the relatively short interval (Vikanes et al. 2010b).
Conclusion
Women with HG had higher PTSS scores following childbirth, compared with women with no nausea and those with less pronounced symptoms. After 2 years, women with HG still had higher PTSS scores compared with women with no nausea. These associations remained significant regardless of the subjective birth experience. Although the overall differences in PTSS scores were small, the results may still be of clinical relevance. Understanding the association between HG and PTSS and perinatal mental health in general may help to move us towards a better, possibly more holistic approach in caring for women with HG, both psychologically and physically.
References
Aksoy H, Aksoy Ü, Karadağ Öİ, Hacimusalar Y, Açmaz G, Aykut G, Çağlı F, Yücel B, Aydın T, Babayiğit MA (2015) Depression levels in patients with hyperemesis gravidarum: a prospective case-control study. SpringerPlus 4:34. https://doi.org/10.1186/s40064-015-0820-2
Ayers S, Bond R, Bertullies S, Wijma K (2016) The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol Med 46:1121–1134. https://doi.org/10.1017/s0033291715002706
Bailham D, Slade P, Joseph S (2004) Principal components analysis of the perceptions of labour and delivery scale and revised scoring criteria. J Reprod Infant Psychol 22:157–165
Birkeland E, Stokke G, Tangvik RJ, Torkildsen EA, Boateng J, Wollen AL, Albrechtsen S, Flaatten H, Trovik J (2015) Norwegian PUQE (Pregnancy-Unique Quantification of Emesis and nausea) identifies patients with hyperemesis gravidarum and poor nutritional intake: a prospective cohort validation study. PLoS One 10:e0119962. https://doi.org/10.1371/journal.pone.0119962
Bolin M, Akerud H, Cnattingius S, Stephansson O, Wikstrom AK (2013) Hyperemesis gravidarum and risks of placental dysfunction disorders: a population-based cohort study. BJOG 120:541–547. https://doi.org/10.1111/1471-0528.12132
Christodoulou-Smith J, Gold JI, Romero R, Goodwin TM, Macgibbon KW, Mullin PM, Fejzo MS (2011) Posttraumatic stress symptoms following pregnancy complicated by hyperemesis gravidarum. J Matern Fetal Neonatal Med 24:1307–1311. https://doi.org/10.3109/14767058.2011.582904
Coddington RD (1972) The significance of life events as etiologic factors in the diseases of children. II. A study of a normal population. J Psychosom Res 16:205–213
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150:782–786. https://doi.org/10.1192/bjp.150.6.782
Cox JL, Chapman G, Murray D, Jones P (1996) Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. J Affect Disord 39:185–189. https://doi.org/10.1016/0165-0327(96)00008-0
Dodds L, Fell DB, Joseph KS, Allen VM, Butler B (2006) Outcomes of pregnancies complicated by hyperemesis gravidarum. Obstet Gynecol 107:285–292. https://doi.org/10.1097/01.AOG.0000195060.22832.cd
Dorheim SK, Bjorvatn B, Eberhard-Gran M (2013) Sick leave during pregnancy: a longitudinal study of rates and risk factors in a Norwegian population. BJOG 120:521–530. https://doi.org/10.1111/1471-0528.12035
Eberhard-Gran M, Eskild A, Tambs K, Schei B, Opjordsmoen S (2001) The Edinburgh Postnatal Depression Scale: validation in a Norwegian community sample. Nord J Psychiatry 55:113–117. https://doi.org/10.1080/08039480151108525
Eliakim R, Abulafia O, Sherer DM (2000) Hyperemesis gravidarum: a current review. Am J Perinatol 17:207–218. https://doi.org/10.1055/s-2000-9424
Fairweather DV (1968) Nausea and vomiting in pregnancy. Am J Obstet Gynecol 102:135–175
Fejzo MS, Poursharif B, Korst LM, Munch S, MacGibbon KW, Romero R, Goodwin TM (2009) Symptoms and pregnancy outcomes associated with extreme weight loss among women with hyperemesis gravidarum. J Women’s Health 18:1981–1987. https://doi.org/10.1089/jwh.2009.1431
Fejzo MS, Myhre R, Colodro-Conde L, MacGibbon KW, Sinsheimer JS, Reddy MV et al (2017) Genetic analysis of hyperemesis gravidarum reveals association with intracellular calcium release channel (RYR2). Mol Cell Endocrinol 439:308–316. https://doi.org/10.1016/j.mce.2016.09.017
Fejzo MS, Sazonova OV, Sathirapongsasuti JF, Hallgrimsdottir IB, Vacic V, MacGibbon KW et al (2018) Placenta and appetite genes GDF15 and IGFBP7 are associated with hyperemesis gravidarum. Nat Commun 9:1178. https://doi.org/10.1038/s41467-018-03258-0
Fell DB, Dodds L, Joseph KS, Allen VM, Butler B (2006) Risk factors for hyperemesis gravidarum requiring hospital admission during pregnancy. Obstet Gynecol 107:277–284. https://doi.org/10.1097/01.aog.0000195059.82029.74
Fiaschi L, Nelson-Piercy C, Gibson J, Szatkowski L, Tata LJ (2018) Adverse maternal and birth outcomes in women admitted to hospital for hyperemesis gravidarum: a population-based cohort study. Paediatr Perinat Epidemiol 32:40–51. https://doi.org/10.1111/ppe.12416
Gadsby R, Barnie-Adshead AM, Jagger C (1993) A prospective study of nausea and vomiting during pregnancy. Br J Gen Pract 43:245–248
Garthus-Niegel S, von Soest T, Vollrath ME, Eberhard-Gran M (2013) The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Arch Womens Ment Health 16:1–10. https://doi.org/10.1007/s00737-012-0301-3
Garthus-Niegel S, Ayers S, von Soest T, Torgersen L, Eberhard-Gran M (2014) Maintaining factors of posttraumatic stress symptoms following childbirth: a population-based, two-year follow-up study. J Affect Disord 172c:146–152. https://doi.org/10.1016/j.jad.2014.10.003
Garthus-Niegel S, Ayers S, Martini J, von Soest T, Eberhard-Gran M (2017) The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based, 2-year follow-up study. Psychol Med 47:161–170. https://doi.org/10.1017/s003329171600235x
Gazmararian JA, Petersen R, Jamieson DJ, Schild L, Adams MM, Deshpande AD, Franks AL (2002) Hospitalizations during pregnancy among managed care enrollees. Obstet Gynecol 100:94–100
Grekin R, O'Hara MW (2014) Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev 34:389–401. https://doi.org/10.1016/j.cpr.2014.05.003
Grooten IJ, Roseboom TJ, Painter RC (2015) Barriers and challenges in hyperemesis gravidarum. Nutr Metab Insights 8:33–39. https://doi.org/10.4137/nmi.s29523
Heitmann K, Solheimsnes A, Havnen GC, Nordeng H, Holst L (2016) Treatment of nausea and vomiting during pregnancy -a cross-sectional study among 712 Norwegian women. Eur J Clin Pharmacol 72:593–604. https://doi.org/10.1007/s00228-016-2012-6
Heitmann K, Nordeng H, Havnen GC, Solheimsnes A, Holst L (2017) The burden of nausea and vomiting during pregnancy: severe impacts on quality of life, daily life functioning and willingness to become pregnant again—results from a cross-sectional study. BMC Pregnancy Childbirth 17:75. https://doi.org/10.1186/s12884-017-1249-0
Hesbacher PT, Rickels K, Morris RJ, Newman H, Rosenfeld H (1980) Psychiatric illness in family practice. J Clin Psychiatry 41:6–10
Horowitz M, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective stress. Psychosom Med 41:209–218
Kim DR, Connolly KR, Cristancho P, Zappone M, Weinrieb RM (2009) Psychiatric consultation of patients with hyperemesis gravidarum. Arch Womens Ment Health 12:61–67. https://doi.org/10.1007/s00737-009-0064-7
Kjeldgaard HK, Eberhard-Gran M, Benth JS, Nordeng H, Vikanes AV (2017a) History of depression and risk of hyperemesis gravidarum: a population-based cohort study. Arch Womens Ment Health 20:397–404. https://doi.org/10.1007/s00737-016-0713-6
Kjeldgaard HK, Eberhard-Gran M, Benth JS, Vikanes AV (2017b) Hyperemesis gravidarum and the risk of emotional distress during and after pregnancy. Arch Womens Ment Health 20:747–756. https://doi.org/10.1007/s00737-017-0770-5
Koren G, Piwko C, Ahn E, Boskovic R, Maltepe C, Einarson A, Navioz Y, Ungar WJ (2005) Validation studies of the Pregnancy Unique-Quantification of Emesis (PUQE) scores. J Obstet Gynaecol 25:241–244. https://doi.org/10.1080/01443610500060651
Lacasse A, Rey E, Ferreira E, Morin C, Berard A (2008) Nausea and vomiting of pregnancy: what about quality of life? BJOG 115:1484–1493. https://doi.org/10.1111/j.1471-0528.2008.01891.x
Lacroix R, Eason E, Melzack R (2000) Nausea and vomiting during pregnancy: a prospective study of its frequency, intensity, and patterns of change. Am J Obstet Gynecol 182:931–937
Mazzotta P, Stewart D, Atanackovic G, Koren G, Magee LA (2000) Psychosocial morbidity among women with nausea and vomiting of pregnancy: prevalence and association with anti-emetic therapy. J Psychosom Obstet Gynaecol 21:129–136
Meltzer-Brody S, Maegbaek ML, Medland SE, Miller WC, Sullivan P, Munk-Olsen T (2017) Obstetrical, pregnancy and socio-economic predictors for new-onset severe postpartum psychiatric disorders in primiparous women. Psychol Med 47:1427–1441. https://doi.org/10.1017/S0033291716003020
Mitchell-Jones N, Gallos I, Farren J, Tobias A, Bottomley C, Bourne T (2017) Psychological morbidity associated with hyperemesis gravidarum: a systematic review and meta-analysis. BJOG 124:20–30. https://doi.org/10.1111/1471-0528.14180
Mullin PM, Ching C, Schoenberg F, MacGibbon K, Romero R, Goodwin TM, Fejzo MS (2012) Risk factors, treatments, and outcomes associated with prolonged hyperemesis gravidarum. J Matern Fetal Neonatal Med 25:632–636. https://doi.org/10.3109/14767058.2011.598588
Murray D, Cox JL (1990) Screening for depression during pregnancy with the Edinburgh depression scale (EDDS). J Reprod Infant Psychol 8:99–107. https://doi.org/10.1080/02646839008403615
Neal LA, Busuttil W, Rollins J, Herepath R, Strike P, Turnbull G (1994) Convergent validity of measures of post-traumatic stress disorder in a mixed military and civilian population. J Trauma Stress 7:447–455
Nilsen RM, Vollset SE, Gjessing HK, Skjaerven R, Melve KK, Schreuder P, Alsaker ER, Haug K, Daltveit AK, Magnus P (2009) Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr Perinat Epidemiol 23:597–608. https://doi.org/10.1111/j.1365-3016.2009.01062.x
Olde E, Kleber RJ, van der Hart O, Pop VJM (2006) Childbirth and posttraumatic stress responses—a validation study of the Dutch Impact of Event Scale—revised. Eur J Psychol Assess 22:259–267. https://doi.org/10.1027/1015-5759.22.4.259
Pirimoglu ZM, Guzelmeric K, Alpay B, Balcik O, Unal O, Turan MC (2010) Psychological factors of hyperemesis gravidarum by using the SCL-90-R questionnaire. Clin Exp Obstet Gynecol 37:56–59
Pop VJ, Truijens SE, Spek V, Wijnen HA, van Son MJ, Bergink V (2015) A new concept of maternity blues: is there a subgroup of women with rapid cycling mood symptoms? J Affect Disord 177:74–79. https://doi.org/10.1016/j.jad.2015.02.015
Poursharif B, Korst LM, Macgibbon KW, Fejzo MS, Romero R, Goodwin TM (2007) Elective pregnancy termination in a large cohort of women with hyperemesis gravidarum. Contraception 76:451–455. https://doi.org/10.1016/j.contraception.2007.08.009
Poursharif B, Korst LM, Fejzo MS, MacGibbon KW, Romero R, Goodwin TM (2008) The psychosocial burden of hyperemesis gravidarum. J Perinatol 28:176–181. https://doi.org/10.1038/sj.jp.7211906
Power Z, Thomson AM, Waterman H (2010) Understanding the stigma of hyperemesis gravidarum: qualitative findings from an action research study. Birth 37:237–244. https://doi.org/10.1111/j.1523-536X.2010.00411.x
Raymond SH (2013) A survey of prescribing for the management of nausea and vomiting in pregnancy in Australasia. Aust N Z J Obstet Gynaecol 53:358–362. https://doi.org/10.1111/ajo.12045
Reed R, Sharman R, Inglis C (2017) Women’s descriptions of childbirth trauma relating to care provider actions and interactions. BMC Pregnancy Childbirth 17:21. https://doi.org/10.1186/s12884-016-1197-0
Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I (2001) Posttraumatic stress disorder and pregnancy complications. Obstet Gynecol 97:17–22
Seng JS, Schrot JA, van De Ven C, Liberzon I (2007) Service use data analysis of pre-pregnancy psychiatric and somatic diagnoses in women with hyperemesis gravidarum. J Psychosom Obstet Gynaecol 28:209–217. https://doi.org/10.1080/01674820701262044
Sheehan DV et al (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–33 quiz 34–57
Swearingen EM, Cohen LH (1985) Measurement of adolescents' life events: the junior high life experiences survey. Am J Community Psychol 13:69–85
Tan A, Lowe S, Henry A (2017) Nausea and vomiting of pregnancy: effects on quality of life and day-to-day function. Aust N Z J Obstet Gynaecol 58:278–290. https://doi.org/10.1111/ajo.12714
Vikanes A, Skjaerven R, Grjibovski AM, Gunnes N, Vangen S, Magnus P (2010a) Recurrence of hyperemesis gravidarum across generations: population based cohort study. BMJ 340:c2050. https://doi.org/10.1136/bmj.c2050
Vikanes A, Grjibovski AM, Vangen S, Gunnes N, Samuelsen SO, Magnus P (2010b) Maternal body composition, smoking, and hyperemesis gravidarum. Ann Epidemiol 20:592–598. https://doi.org/10.1016/j.annepidem.2010.05.009
World Health Organization (2004) ICD-10, chapter XV, pregnancy, childbirth and the puerperium (O00-O99), other maternal disorders predominantly related to pregnancy (O20-O29). World Health Organization. http://apps.who.int/classifications/apps/icd/icd10online2004/fr-icd.htm?go20.htm+
Acknowledgements
The authors would like to thank the involvement of the staff within the maternity wards at Akershus University Hospital for their contributions towards this project. They are also grateful to all the participating women.
Funding
HKK was funded by the South-Eastern Norway Regional Health Authority (grant no.2014003). The ABC study was funded by the Norwegian Research Council (project number 191098). The funding sources had no role in the conduct of the study.
Author information
Authors and Affiliations
Contributions
MEG conceived, designed and coordinated the ABC study. ÅV, MEG, SGN, CJ and HKK prepared the protocol for the current study. HKK analysed the data and prepared the manuscript. JSB supervised the data analyses. All authors were involved in interpreting the data, critically revising the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Table
(DOCX 18 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kjeldgaard, H.K., Vikanes, Å., Benth, J.Š. et al. The association between the degree of nausea in pregnancy and subsequent posttraumatic stress. Arch Womens Ment Health 22, 493–501 (2019). https://doi.org/10.1007/s00737-018-0909-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-018-0909-z