Abstract
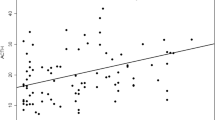
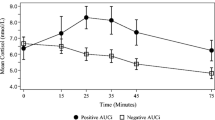
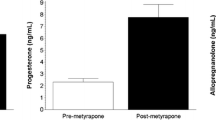
It is unclear whether women with a history of postpartum depression (PPD) have residual, abnormal hypothalamic-pituitary-adrenal (HPA) axis reactivity, as has been reported in major depression (MDD). Further unclear is whether the abnormalities in HPA axis reactivity associated with MDD represent a stable, underlying predisposition or a state-dependent phenomenon. This study sought the following: (1) to determine if euthymic postpartum women with a history of depression have an abnormal HPA axis reactivity to pharmacologic and psychological challenges and (2) to compare HPA reactivity in women with histories of PPD versus MDD. As a secondary objective, we wanted to determine the influence of trauma history on HPA axis function. Forty-five parous (12–24 months postpartum), euthymic women with history of MDD (n = 15), PPD (n = 15), and controls (n = 15) completed pharmacologic (dexamethasone/corticotropin-releasing hormone (CRH) test [DEX/CRH]) and psychological (Trier social stress test [TSST]) challenges during the luteal phase. Outcome measures were cortisol and adrenocorticotropic hormone (ACTH) response after DEX/CRH, and blood pressure, heart rate, epinephrine, norepinephrine, and cortisol response during the TSST. All groups had robust cortisol and ACTH response to DEX/CRH and cortisol response to TSST. Groups did not differ significantly in cortisol or ACTH response to DEX/CRH or in blood pressure, heart rate, epinephrine, norepinephrine, or cortisol response to TSST. Cortisol/ACTH ratio did not differ significantly between groups. Trauma history was associated with decreased cortisol response to DEX/CRH in women with histories of MDD, which was not significant after correction (F 8,125, p = 0.02, Greenhouse-Geisser corrected p = 0.11). Currently euthymic women with histories of MDD or PPD did not demonstrate residual abnormal stress responsivity following administration of either a pharmacologic or psychological stressor.




Similar content being viewed by others
References
Ahrens T, Deuschle M, Krumm B, van der Pompe G, den Boer JA, Lederbogen F (2008) Pituitary-adrenal and sympathetic nervous system responses to stress in women remitted from recurrent major depression. Psychosom Med 70(4):461–467. doi:10.1097/PSY.0b013e31816b1aaa
Anacker C, Zunszain PA, Carvalho LA, Pariante CM (2011) The glucocorticoid receptor: pivot of depression and of antidepressant treatment? Psychoneuroendocrinology 36(3):415–425. doi:10.1016/j.psyneuen.2010.03.007
Bagley SL, Weaver TL, Buchanan TW (2011) Sex differences in physiological and affective responses to stress in remitted depression. Physiol Behav 104(2):180–186. doi:10.1016/j.physbeh.2011.03.004
Bloch M, Rubinow DR, Schmidt PJ, Lotsikas A, Chrousos GP, Cizza G (2005) Cortisol response to ovine corticotropin-releasing hormone in a model of pregnancy and parturition in euthymic women with and without a history of postpartum depression. J Clin Endocrinol Metab 90(2):695–699
Brand SR, Brennan PA, Newport DJ, Smith AK, Weiss T, Stowe ZN (2010) The impact of maternal childhood abuse on maternal and infant HPA axis function in the postpartum period. Psychoneuroendocrinology 35(5):686–693. doi:10.1016/j.psyneuen.2009.10.009
Burke HM, Davis MC, Otte C, Mohr DC (2005) Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology 30(9):846–856
Buttner MM, Mott SL, Pearlstein T, Stuart S, Zlotnick C, O’Hara MW (2013) Examination of premenstrual symptoms as a risk factor for depression in postpartum women. Arch Women’s Ment Health 16(3):219–225. doi:10.1007/s00737-012-0323-x
Carpenter LL, Tyrka AR, Ross NS, Khoury L, Anderson GM, Price LH (2009) Effect of childhood emotional abuse and age on cortisol responsivity in adulthood. Biol Psychiatry 66(1):69–75. doi:10.1016/j.biopsych.2009.02.030
Dietz PM, Williams SB, Callaghan WM, Bachman DJ, Whitlock EP, Hornbrook MC (2007) Clinically identified maternal depression before, during, and after pregnancies ending in live births. Am J Psychiatr 164(10):1515–1520
Glynn LM, Davis EP, Sandman CA (2013) New insights into the role of perinatal HPA-axis dysregulation in postpartum depression. Neuropeptides 47(6):363–370. doi:10.1016/j.npep.2013.10.007
Gold PW, Gabry KE, Yasuda MR, Chrousos GP (2002) Divergent endocrine abnormalities in melancholic and atypical depression: clinical and pathophysiologic implications. Endocrinol Metab Clin N Am 31(1):37–62, vi
Groer MW, Morgan K (2007) Immune, health and endocrine characteristics of depressed postpartum mothers. Psychoneuroendocrinology 32(2):133–139
Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB (2008) The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology 33(6):693–710. doi:10.1016/j.psyneuen.2008.03.008
Hohne N, Poidinger M, Merz F, Pfister H, Bruckl T, Zimmermann P, Uhr M, Holsboer F, Ising M (2014) Increased HPA axis response to psychosocial stress in remitted depression: the influence of coping style. Biol Psychol 103:267–275. doi: 10.1016/j.biopsycho.2014.09.008
Holsen LM, Lancaster K, Klibanski A, Whitfield-Gabrieli S, Cherkerzian S, Buka S, Goldstein JM (2013) HPA-axis hormone modulation of stress response circuitry activity in women with remitted major depression. Neuroscience 250:733–742. doi:10.1016/j.neuroscience.2013.07.042
Keating C, Dawood T, Barton DA, Lambert GW, Tilbrook AJ (2013) Effects of selective serotonin reuptake inhibitor treatment on plasma oxytocin and cortisol in major depressive disorder. BMC Psychiatry 13:124. doi:10.1186/1471-244X-13-124
Kepple AL, Lee EE, Haq N, Rubinow DR, Schmidt PJ (2016) History of post-partum depression in a clinic-based sample of women with premenstrual dysphoric disorder. J Clin Psychiatry 77(4):e415–e420. doi:10.4088/JCP.15m09779
Kirschbaum C, Pirke KM, Hellhammer DH (1993) The ‘Trier Social Stress Test’—a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 28(1–2):76–81
Kunzel HE, Binder EB, Nickel T, Ising M, Fuchs B, Majer M, Pfennig A, Ernst G, Kern N, Schmid DA, Uhr M, Holsboer F, Modell S (2003) Pharmacological and nonpharmacological factors influencing hypothalamic-pituitary-adrenocortical axis reactivity in acutely depressed psychiatric in-patients, measured by the Dex-CRH test. Neuropsychopharmacology 28(12):2169–2178. doi: 10.1038/sj.npp.1300280
Lange C, Zschucke E, Ising M, Uhr M, Bermpohl F, Adli M (2013) Evidence for a normal HPA axis response to psychosocial stress in patients remitted from depression. Psychoneuroendocrinology 38(11):2729–2736. doi:10.1016/j.psyneuen.2013.06.033
Lee RJ, Hempel J, Tenharmsel A, Liu T, Mathe AA, Klock A (2012) The neuroendocrinology of childhood trauma in personality disorder. Psychoneuroendocrinology 37(1):78–86. doi:10.1016/j.psyneuen.2011.05.006
Lok A, Mocking RJ, Ruhe HG, Visser I, Koeter MW, Assies J, Bockting CL, Olff M, Schene AH (2012) Longitudinal hypothalamic-pituitary-adrenal axis trait and state effects in recurrent depression. Psychoneuroendocrinology 37(7): 892–902. doi: 10.1016/j.psyneuen.2011.10.005
MacMillan HL, Georgiades K, Duku EK, Shea A, Steiner M, Niec A, Tanaka M, Gensey S, Spree S, Vella E, Walsh CA, De Bellis MD, Van der Meulen J, Boyle MH, Schmidt LA (2009) Cortisol response to stress in female youths exposed to childhood maltreatment: results of the youth mood project. Biol Psychiatry 66(1):62–68. doi: 10.1016/j.biopsych.2008.12.014
Magiakou MA, Mastorakos G, Rabin D, Dubbert B, Gold PW, Chrousos GP (1996) Hypothalamic corticotropin-releasing hormone suppression during the postpartum period: implications for the increase in psychiatric manifestations at this time. J Clin Endocrinol Metab 81(5):1912–1917. doi:10.1210/jcem.81.5.8626857
Pariante CM (2009) Risk factors for development of depression and psychosis. Glucocorticoid receptors and pituitary implications for treatment with antidepressant and glucocorticoids. Ann N Y Acad Sci 1179:144–152. doi:10.1111/j.1749-6632.2009.04978.x
Pariante CM, Lightman SL (2008) The HPA axis in major depression: classical theories and new developments. Trends Neurosci 31(9):464–468. doi:10.1016/j.tins.2008.06.006
Parry BL, Sorenson DL, Meliska CJ, Basavaraj N, Zirpoli GG, Gamst A, Hauger R (2003) Hormonal basis of mood and postpartum disorders. Curr Womens Health Rep 3(3):230–235
Roca CA, Schmidt PJ, Altemus M, Deuster P, Danaceau MA, Putnam K, Rubinow DR (2003) Differential menstrual cycle regulation of hypothalamic-pituitary-adrenal axis in women with premenstrual syndrome and controls. J Clin Endocrinol Metab 88(7):3057–3063. doi:10.1210/jc.2002-021570
Ruhe HG, Khoenkhoen SJ, Ottenhof KW, Koeter MW, Mocking RJ, Schene AH (2015) Longitudinal effects of the SSRI paroxetine on salivary cortisol in major depressive disorder. Psychoneuroendocrinology 52:261–271. doi:10.1016/j.psyneuen.2014.10.024
Schiller CE, Meltzer-Brody S, Rubinow DR (2015) The role of reproductive hormones in postpartum depression. CNS Spectr 20(1):48–59. doi:10.1017/S1092852914000480
Schule C (2007) Neuroendocrinological mechanisms of actions of antidepressant drugs. J Neuroendocrinol 19(3):213–226
Sher L, Oquendo MA, Galfalvy HC, Cooper TB, Mann JJ (2004) The number of previous depressive episodes is positively associated with cortisol response to fenfluramine administration. Ann N Y Acad Sci 1032:283–286
Taylor A, Glover V, Marks M, Kammerer M (2009) Diurnal pattern of cortisol output in postnatal depression. Psychoneuroendocrinology 34(8):1184–1188
Young EA, Abelson JL, Cameron OG (2004) Effect of comorbid anxiety disorders on the hypothalamic-pituitary-adrenal axis response to a social stressor in major depression. Biol Psychiatry 56(2):113–120. doi:10.1016/j.biopsych.2004.03.017
Acknowledgements
We would like to thank the study participants who generously gave of their time. We would also like to acknowledge the late Dr. Robert M. Hamer, biostatistician, for his contribution to the study design, his thoughtful guidance, and the invaluable role he played in the training of Dr. Ferguson and so many others at The University of North Carolina at Chapel Hill.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was supported by the National Institutes of Health Grant K23MH085165 (PI: Meltzer-Brody).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ferguson, E.H., Di Florio, A., Pearson, B. et al. HPA axis reactivity to pharmacologic and psychological stressors in euthymic women with histories of postpartum versus major depression. Arch Womens Ment Health 20, 411–420 (2017). https://doi.org/10.1007/s00737-017-0716-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-017-0716-y