Abstract
Background
Surgical risk in patients with unruptured aneurysms is well known. The relative impact of surgery and natural history of subarachnoid haemorrhage (SAH) on patients in good clinical condition (World Federation of Neurological Surgeons [WFNS] grades 1 and 2) is less well quantified. The aim of this study was to determine causes of poor outcome in patients admitted in good grade SAH.
Methods
A retrospective study of prospectively collected data among WFNS-1 and -2 patients: demographics, SAH and aneurysm-related data, surgical complications and outcome as assesed by the Glasgow Outcome Scale (GOS). Causes of poor outcome (GOS 1–3) were determined.
Results
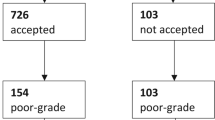
During a 7-year period (2009–15), 56 patients with SAH WFNS-1 (39 patients) or WFNS-2 (17 patients) were treated surgically (21 men, 35 women; mean age, 52.4 years). According to the Fisher scale, 19 patients were grade 1 or 2; 37 patients were grade 3 or 4. Most aneurysms were located at anterior communicating (26) or middle cerebral (15) artery.
Altogether, 11 patients (19.6%) achieved GOS 1–3. This was attributed to SAH-related complications in six patients (rebleeding, vasospasm), surgery in four patients (postoperative ischaemia in two, haematoma and ventriculitis in one patient each), grand-mal seizure with aspiration in one patient. Age over 60 years (p = 0.017) and presence of hydrocephalus (p < 0.001) were statistically significant predictors of poor GOS; other variables (e.g. sex, Fisher grade, aneurysm size or location, use of temporary clips, intraoperative rupture, vasospasm) were not significant.
Conclusions
Patients admitted in good-grade SAH achieve favourable outcome following surgical aneurysm repair in the majority of cases. Negative factors include age over 60 years and presence of hydrocephalus. Aneurysm surgery following good-grade SAH still carries a small but significant risk similar to that shown in large multi-institutional trials.
Similar content being viewed by others
References
Akyuz M, Tuncer R (2006) The effects of fenestration of the interpeduncular cistern membrane arousted to the opening of lamina terminalis in patients with ruptured ACoA aneurysms: a prospective, comparative study. Acta Neurochir (Wien) 148:723–725, discussion 731–722
Bardach NS, Zhao S, Gress DR, Lawton MT, Johnston SC (2002) Association between subarachnoid hemorrhage outcomes and number of cases treated at California hospitals. Stroke 33:1851–1856
Barker FG II, Amin-Hanjani S, Butler WE, Ogilvy CS, Carter BS (2003) In-hospital mortality and morbidity after surgical treatment of unruptured intracranial aneurysms in the United States, 1996–2000: the effect of hospital and surgeon volume. Neurosurgery 52:995–1009
Britz GW (2005) ISAT trial: coiling or clipping for intracranial aneurysms? Lancet 366:783–785
Bulters DO, Santarius T, Chia HL, Parker RA, Trivedi R, Kirkpatrick PJ, Kirollos RW (2011) Causes of neurological deficits following clipping of 200 consecutive ruptured aneurysms in patients with good-grade aneurysmal subarachnoid haemorrhage. Acta Neurochir (Wien) 153:295–303
Cowan JA, Ziewacz J, Dimick JB, Upchurch GR, Thompson BG (2007) Use of endovascular coil embolization and surgical clip occlusion for cerebral artery aneurysms. J Neurosurg 107:530–535
Crobeddu E, Mittal MK, Dupont S, Wijdicks EF, Lanzino G, Rabinstein AA (2012) Predicting the lack of development of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Stroke 43:697–701
Dupont SA, Wijdicks EF, Manno EM, Lanzino G, Rabinstein AA (2009) Prediction of angiographic vasospasm after aneurysmal subarachnoid hemorrhage: value of the Hijdra sum scoring system. Neurocrit Care 11:172–176
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6:1–9
Frontera JA, Fernandez A, Schmidt JM, Claassen J, Wartenberg KE, Badjatia N, Connolly ES, Mayer SA (2009) Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke 40:1963–1968
Graff-Radford NR, Torner J, Adams HP Jr, Kassell NF (1989) Factors associated with hydrocephalus after subarachnoid hemorrhage. A report of the Cooperative Aneurysm Study. Arch Neurol 46:744–752
Harbaugh RE, Heros RC, Hadley MN (2003) More on ISAT. Lancet 361:783–784, author reply 784
Hoh BL, Rabinov JD, Pryor JC, Carter BS, Barker FG 2nd (2003) In-hospital morbidity and mortality after endovascular treatment of unruptured intracranial aneurysms in the United States, 1996–2000: effect of hospital and physician volume. AJNR Am J Neuroradiol 24:1409–1420
Jurák L, Bradáč O, Kaiser M, Brabec R, Buchvald P, Endrych L, Suchomel P (2013) Hydrocefalus jako komplikace subarachnoidálního krvácení. Cesk Slov Neurol N 76:70–75
Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL (1990) The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1: Overall management results. J Neurosurg 73:18–36
Kassell NF, Torner JC, Jane JA, Haley EC Jr, Adams HP (1990) The International Cooperative Study on the Timing of Aneurysm Surgery. Part 2: Surgical results. J Neurosurg 73:37–47
Krisht AF, Gomez J, Partington S (2006) Outcome of surgical clipping of unruptured aneurysms as it compares with a 10-year nonclipping survival period. Neurosurgery 58:207–216, discussion 207–216
McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, Albuquerque FC (2011) The Barrow Ruptured Aneurysm Trial. J Neurosurg 116:135–144
McLaughlin N, Bojanowski MW (2004) Early surgery-related complications after aneurysm clip placement: an analysis of causes and patient outcomes. J Neurosurg 101:600–606
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360:1267–1274
Raaymakers TW, Rinkel GJ, Limburg M, Algra A (1998) Mortality and morbidity of surgery for unruptured intracranial aneurysms: a meta-analysis. Stroke 29:1531–1538
Rabinstein AA, Pichelmann MA, Friedman JA, Piepgras DG, Nichols DA, McIver JI, Toussaint LG 3rd, McClelland RL, Fulgham JR, Meyer FB, Atkinson JL, Wijdicks EF (2003) Symptomatic vasospasm and outcomes following aneurysmal subarachnoid hemorrhage: a comparison between surgical repair and endovascular coil occlusion. J Neurosurg 98:319–325
Saveland H, Hillman J, Brandt L, Edner G, Jakobsson KE, Algers G (1992) Overall outcome in aneurysmal subarachnoid hemorrhage. A prospective study from neurosurgical units in Sweden during a 1-year period. J Neurosurg 76:729–734
Spetzler RF, McDougall CG, Albuquerque FC, Zabramski JM, Hills NK, Partovi S, Nakaji P, Wallace RC (2013) The Barrow Ruptured Aneurysm Trial: 3-year results. J Neurosurg 119:146–157
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, De Villiers JC (1988) A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry 51:1457
Todd MM, Hindman BJ, Clarke WR, Torner JC (2005) Mild intraoperative hypothermia during surgery for intracranial aneurysm. N Engl J Med 352:135–145
Wester K (2009) Lessons learned by personal failures in aneurysm surgery: what went wrong, and why? Acta Neurochir (Wien) 151:1013–1024
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O’Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362:103–110
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
This is an important article particularly considering that the senior surgeon (and all the surgeons) are highly talented and the institution is an excellent one with great experience. So we can assume that the results are honest and valid.
To be concise, good-grade SAH patients in this series, WFNS 1 and 2, operated for primarily MCA or ACoA aneurysms, still experience a near 20% risk of poor outcome. This is not the 5% or so number that most of us would like to own or admit to for patients we consider good-grade, yet no doubt it reflects the state of the art and the realities that SAH patients face. The culprits are the usual ones, rebleeding, surgical complications, hydrocephalus, DIND, infection, epilepsy. We have lived this life and faced these adversaries routinely.
Let us be honest also. Many of us who completed training 25-30 years ago, prior to endovascular techniques, were experts in aneurysm surgery and approached with relish both unruptured and SAH patients, with the philosophy that what we offered was a surgical art as highly developed as we could make it, and with complete confidence that we were offering to the patient the best possible treatment. But the refinement of endovascular therapy changed the balance and reset the goalposts (or in the Rest of World we should say moved the goalkeeper’s net). The numbers of surgeons like us are declining, both in the number of cases that we do, and in the number of graduate neurosurgeons with the training and the case experience to perform these operations. As mentors and leaders we now encourage every surgeon interested in cerebrovascular disease to acquire endovascular skills. This was unthinkable when I graduated my own training. I do not believe we will ever go back to those days.
So this paper is an excellent one, from quality surgeons. What we do with the information is left to our own judgment. As for me, I need a comparator between these quality data and the results of endovascular treatment in the same patient group. Then I will know what is the best recommendation when I sit face to face with a patient or family.
I recommend this paper to all readers, and especially trainees, as a useful and learned dissertation on the philosophy and process of decision making in surgery for aneurysmal SAH.
Christopher Miranda Loftus
IL, USA
The submitted article has been in part presented at the 16th European Congress of Neurosurgery in Athens, Greece (4-8 September 2016) in the form of an e-poster
Rights and permissions
About this article
Cite this article
Beneš, V., Jurák, L., Brabec, R. et al. Causes of poor outcome in patients admitted with good-grade subarachnoid haemorrhage. Acta Neurochir 159, 559–565 (2017). https://doi.org/10.1007/s00701-017-3081-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3081-8



