Abstract
Background
Traumatic spinal injuries can be life-threatening conditions. Despite numerous epidemiological studies, reports on specific spinal regions affected are lacking.
Hypothesis
We hypothesized that fractures at specific regions, such as the cervical spine (including the axis segment), have been affected to a greater degree. We also hypothesized that advanced age may be a significant contributing factor.
Objective
To longitudinally analyze trend of spine fractures and specific fracture subtypes.
Study design
Longitudinal trend analysis of discharged patient state database.
Patient sample
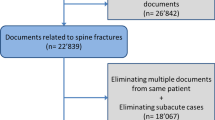
Discharged patient’s data from 15 years (2003–2017)
Methods
We retrieved pertinent ICD-9 and 10 codes depicting fractures involving the entire spine and specific subtypes. To assess possible association with age, we analyzed the trend of the average age in patients discharged with and without spinal fractures as well as in specific fracture subtypes. Similar analysis was performed for other common fragility fractures. FDA device/drug status: The manuscript submitted does not contain information about medical device(s) or drug(s).
Results
We found that within 15 years, the overall proportion of spinal fractures has increased by 64% (from 0.47 to 0.77% of all discharged patients) with the greatest increase noted in fractures of the cervical spine (123%) and specifically of the second cervical vertebra (84%). Age was found to have increased more in patients with spinal fractures than in the general discharged population. Surprisingly, other non-spinal fractures among patients above 60 remained relatively stable, demonstrating a spine-specific effect.
Conclusions
Our findings confirm a recent increase in all spinal fractures and in the cervical and sacral regions in particular. Advanced age may be an important underlying factor.





Similar content being viewed by others
References
Clark P, Letts M (2001) Trauma to the thoracic and lumbar spine in the adolescent. Can J Surg 44:337–345
Sayama C, Chen T, Trost G, Jea A (2014) A review of pediatric lumbar spine trauma. Neurosurg Focus 37:E6
Anissipour AK, Agel J, Bellabarba C, Bransford RJ (2017) Cervical facet dislocations in the adolescent population: a report of 21 cases at a level 1 trauma center from 2004 to 2014. Eur Spine J 26:1266–1271
Old JL, Calvert M (2004) Vertebral compression fractures in the elderly. Am Fam Phys 69:111–116
Tsuda T (2017) Epidemiology of fragility fractures and fall prevention in the elderly: a systematic review of the literature. Curr Orthop Pr 28:580–585
Pisani P, Renna MD, Conversano F et al (2016) Major osteoporotic fragility fractures: Risk factor updates and societal impact. World J Orthop 7:171–181
Bleibler F, Rapp K, Jaensch A et al (2014) Expected lifetime numbers and costs of fractures in postmenopausal women with and without osteoporosis in Germany: a discrete event simulation model. BMC Heal Serv Res 14:284
Smith HE, Kerr SM, Fehlings MG et al (2010) Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. J Spinal Disord Tech 23:501–505
Stevens JA, Corso PS, Finkelstein EA, Miller TR (2006) The costs of fatal and non-fatal falls among older adults. Inj Prev 12:290–295
Hardy I, McFaull S, Saint-Vil D (2015) Neck and spine injuries in Canadian cheerleaders: an increasing trend. J Pediatr Surg 50:790–792
Kim TY, Jang S, Park CM et al (2016) Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci 31:801–805
Ten Brinke JG, Saltzherr TP, Panneman MJM et al (2017) Incidence of spinal fractures in the Netherlands 1997–2012. J Clin Orthop Trauma 8:S67–S70
Oudshoorn C, Hartholt KA, Zillikens MC et al (2012) Emergency department visits due to vertebral fractures in the Netherlands, 1986–2008: steep increase in the oldest old, strong association with falls. Injury 43:458–461
Amin S, Achenbach SJ, Atkinson EJ et al (2014) Trends in fracture incidence: a population-based study over 20 years. J Bone Min Res 29:581–589
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. study of osteoporotic fractures research group. Arch Intern Med 159:1215–1220. https://doi.org/10.1001/archinte.159.11.1215
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28:1531–1542. https://doi.org/10.1007/s00198-017-3909-3
Kukreja S, Kalakoti P, Murray R et al (2015) National trends of incidence, treatment, and hospital charges of isolated C-2 fractures in three different age groups. Neurosurg Focus 38:E19
Dettori JR, Chapman JR, DeVine JG et al (2016) The risk of cancer with the use of recombinant human bone morphogenetic protein in spine fusion. Spine 41:1317–1324. https://doi.org/10.1097/BRS.0000000000001671
Melton LJ (1997) Epidemiology of spinal osteoporosis. Spine 22:2S–11S
Baaj AA, Uribe JS, Nichols TA et al (2010) Health care burden of cervical spine fractures in the United States: analysis of a nationwide database over a 10-year period. J Neurosurg Spine 13:61–66
Johnell O (2003) Economic implication of osteoporotic spine disease: cost to society. Eur Spine J 12(Suppl 2):S168–S169
Qu B, Ma Y, Yan M et al (2014) The economic burden of fracture patients with osteoporosis in western China. Osteoporos Int 25:1853–1860
Gehlbach SH, Burge RT, Puleo E, Klar J (2003) Hospital care of osteoporosis-related vertebral fractures. Osteoporos Int 14:53–60
van der Roer N, de Bruyne MC, Bakker FC et al (2005) Direct medical costs of traumatic thoracolumbar spine fractures. Acta Orthop 76:662–666
Siebenga J, Segers MJ, Leferink VJ et al (2007) Cost-effectiveness of the treatment of traumatic thoracolumbar spine fractures: nonsurgical or surgical therapy? Indian J Orthop 41:332–336
Fink HA, Ensrud KE, Nelson DB et al (2003) Disability after clinical fracture in postmenopausal women with low bone density: the fracture intervention trial (FIT). Osteoporos Int 14:69–76
Bartels SJ, Naslund JA (2013) The underside of the silver tsunami–older adults and mental health care. N Engl J Med 368:493–496
Bluethmann SM, Mariotto AB, Rowland JH (2016) Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomark Prev 25:1029–1036
Burge R, Dawson-Hughes B, Solomon DH et al (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Min Res 22:465–475
Gibon E, Lu L, Goodman SB (2016) Aging, inflammation, stem cells, and bone healing. Stem Cell Res Ther 7:44
Drazin D, Nuno M, Shweikeh F et al (2016) Outcomes and national trends for the surgical treatment of lumbar spine trauma. Biomed Res Int 2016:3623875
Goz V, Errico TJ, Weinreb JH et al (2015) Vertebroplasty and kyphoplasty: national outcomes and trends in utilization from 2005 through 2010. Spine J 15:959–965
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors hereby certify that the current research was conducted in its entirety in the Swedish Neuroscience Institute, Seattle, WA.
Appendix
Appendix
-
(1)
List of codes used for the identification of spinal fractures
ICD 9
Cervical: 8050*; 8051*; 8060*; 8061* (axis fractures: 80502; 80512)
Thoracic: 8052; 8053; 8062*; 8063*
Lumbar: 8054; 8055; 8064*; 8065*
Sacro-coccygeal: 8056; 8057; 8066*; 8067*
Distal radius: 81341*; 81342*; 81344*; 81351*; 81352*; 81354*
Proximal femur: 820*
ICD 10
Cervical: S120*; S121*; S122*; S123*; S124*; S125*; S126*; S129*
Thoracic: S2200*; S2201*; S2202*; S2203*; S2204*; S2205*; S2206*; S2207*; S2208*
Lumbar: S320*
Sacro-coccygeal: S321*
Distal radius: S525*
Proximal femur: S720*; S721*; S722*
Rights and permissions
About this article
Cite this article
Blecher, R., Yilmaz, E., Ishak, B. et al. Uptrend of cervical and sacral fractures underlie increase in spinal fractures in the elderly, 2003–2017: analysis of a state-wide population database. Eur Spine J 29, 2543–2549 (2020). https://doi.org/10.1007/s00586-020-06498-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06498-1