Abstract
Purpose
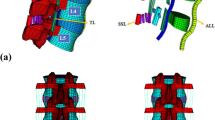
Hybrid stabilization with a dynamic implant has been suggested to avoid adjacent segment disease by creating a smoother transition zone from the instrumented segments to the untreated levels above. This study aims to characterize the transition zones of two-level posterior instrumentation strategies for elucidating biomechanical differences between rigid fixation and the hybrid stabilization approach with a pedicle screw-based dynamic implant.
Methods
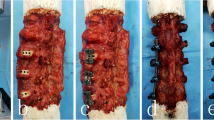
Eight human lumbar spines (L1–5) were loaded in a spine tester with pure moments of 7.5 Nm and with a hybrid loading protocol. The range of motion (ROM) of all segments for both loading protocols was evaluated and normalized to the native ROM.
Results
For pure moment loading, ROM of the segments cranial to both instrumentations were not affected by the type of instrumentation (p > 0.5). The dynamic instrumentation in L3–4 reduced the ROM compared to intact (p < 0.05) but allowed more motion than the rigid fixation of the same segment (p < 0.05). Under hybrid loading testing, the cranial segments (L1–2, L2–3) had a significant higher ROM for both instrumentations compared to the intact (p < 0.05). Comparing the two instrumentations with each other, the rigid fixation resulted in a higher increased ROM of L1–2 and L2–3 than hybrid stabilization.
Conclusions
Regardless of the implant, two-level posterior instrumentation was accompanied by a considerable amount of compensatory movement in the cranial untreated segments under the hybrid protocol. Hybrid stabilization, however, showed a significant reduction of this compensatory movement in comparison to rigid fixation. These results could support the surgical strategy of hybrid stabilization, whereas the concept of topping-off, including a healthy segment, is discouraged.






Similar content being viewed by others
References
Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B (2011) Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 11:11–20. https://doi.org/10.1016/j.spinee.2010.09.026
Pan A, Hai Y, Yang J, Zhou L, Chen X, Guo H (2016) Adjacent segment degeneration after lumbar spinal fusion compared with motion-preservation procedures: a meta-analysis. Eur Spine J 25:1522–1532. https://doi.org/10.1007/s00586-016-4415-6
Norvell DC, Dettori JR, Skelly AC, Riew KD, Chapman JR, Anderson PA (2012) Methodology for the systematic reviews on an adjacent segment pathology. Spine 37:10–17. https://doi.org/10.1097/BRS.0b013e31826cd9c8
Lawrence BD, Wang J, Arnold PM, Hermsmeyer J, Norvell DC, Brodke DS (2012) Predicting the risk of adjacent segment pathology after lumbar fusion: a systematic review. Spine 37:123–132. https://doi.org/10.1097/BRS.0b013e31826d60d8
He B, Yan L, Guo H, Liu T, Wang X, Hao D (2014) The difference in superior adjacent segment pathology after lumbar posterolateral fusion by using 2 different pedicle screw insertion techniques in 9-year minimum follow-up. Spine 39:1093–1098. https://doi.org/10.1097/BRS.0000000000000353
Ou CY, Lee TC, Lee TH, Huang YH (2015) Impact of body mass index on adjacent segment disease after lumbar fusion for degenerative spine disease. Neurosurgery 76:396–401. https://doi.org/10.1227/NEU.0000000000000627
Yamasaki K, Hoshino M, Omori K et al (2017) Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine 42:E86–E92. https://doi.org/10.1097/BRS.0000000000001728
Wang H, Ma L, Yang D et al (2017) Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine 96:e6032. https://doi.org/10.1097/MD.0000000000006032
Putzier M, Hoff E, Tohtz S, Gross C, Perka C, Strube P (2010) Dynamic stabilization adjacent to single-level fusion: part II. No clinical benefit for asymptomatic, initially degenerated adjacent segments after 6 years follow-up. Eur Spine J 19:2181–2189. https://doi.org/10.1007/s00586-010-1517-4
Strube P, Tohtz S, Hoff E, Gross C, Perka C, Putzier M (2010) Dynamic stabilization adjacent to single-level fusion: part I. Biomechanical effects on lumbar spinal motion. Eur Spine J 19:2171–2180. https://doi.org/10.1007/s00586-010-1549-9
Korovessis P, Repantis T, Zacharatos S, Zafiropoulos A (2009) Does Wallis implant reduce adjacent segment degeneration above lumbosacral instrumented fusion? Eur Spine J 18:830–840. https://doi.org/10.1007/s00586-009-0976-y
Fleege C, Rickert M, Werner I, Rauschmann M, Arabmotlagh M (2016) Hybrid stabilization technique with spinal fusion and interlaminar device to reduce the length of fusion and to protect symptomatic adjacent segments: clinical long-term follow-up. Orthopade 45:770–779. https://doi.org/10.1007/s00132-016-3312-3
Li C, Liu L, Shi JY, Yan KZ, Shen WZ, Yang ZR (2016) Clinical and biomechanical researches of polyetheretherketone (PEEK) rods for semi-rigid lumbar fusion: a systematic review. Neurosurg Rev. https://doi.org/10.1007/s10143-016-0763-2
Andrieu K, Allain J, Longis PM, Steib JP, Beaurain J, Delécrin J (2017) Comparison between total disc replacement and hybrid construct at two lumbar levels with minimum follow-up of 2 years. Orthop Traumatol Surg Res 103:39–43. https://doi.org/10.1016/j.otsr.2016.06.018
Tachibana N, Kawamura N, Kobayashi D et al (2017) Preventive effect of dynamic stabilization against adjacent segment degeneration after posterior lumbar interbody fusion. Spine 42:25–32. https://doi.org/10.1097/BRS.0000000000001654
Wilke HJ, Heuer F, Schmidt H (2009) Prospective design delineation and subsequent in vitro evaluation of a new posterior dynamic stabilization system. Spine 34:255–261. https://doi.org/10.1097/BRS.0b013e3181920e9c
Knop C, Lange U, Bastian L, Blauth M (2000) Three-dimensional motion analysis with Synex. Comparative biomechanical test series with a new vertebral body replacement for the thoracolumbar spine. Eur Spine J 9:472–485
Lange T, Schmoelz W, Gosheger G et al (2017) Is a gradual reduction of stiffness on top of posterior instrumentation possible with a suitable proximal implant? A biomechanical study. Spine J. https://doi.org/10.1016/j.spinee.2017.03.021
Wilke HJ, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7:148–154
Panjabi MM (2007) Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech 22:257–265. https://doi.org/10.1016/j.clinbiomech.2006.08.006
Schmoelz W, Huber JF, Nydegger T, Claes L, Wilke HJ (2003) Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech 16:418–423
Volkheimer D, Malakoutian M, Oxland TR, Wilke HJ (2015) Limitations of current in vitro test protocols for investigation of instrumented adjacent segment biomechanics: critical analysis of the literature. Eur Spine J 24:1882–1892. https://doi.org/10.1007/s00586-015-4040-9
Mageswaran P, Techy F, Colbrunn RW, Bonner TF, McLain RF (2012) Hybrid dynamic stabilization: a biomechanical assessment of adjacent and supraadjacent levels of the lumbar spine. J Neurosurg Spine 17:232–242. https://doi.org/10.3171/2012.6.SPINE111054
Cheng BC, Gordon J, Cheng J, Welch WC (2007) Immediate biomechanical effects of lumbar posterior dynamic stabilization above a circumferential fusion. Spine 32:2551–2557. https://doi.org/10.1097/BRS.0b013e318158cdbe
Malakoutian M, Street J, Wilke HJ, Stavness I, Dvorak M, Fels S, Oxland T (2016) Role of muscle damage on loading at the level adjacent to a lumbar spine fusion: a biomechanical analysis. Eur Spine J 25:2929–2937. https://doi.org/10.1007/s00586-016-4686-y
Acknowledgements
The laboratory costs of the study were supported by Paradigm Spine GmbH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. A. Hegewald received speaker honorarium and worked as a clinical consultant for Paradigm Spine GmbH. All other authors declare that they have no conflict of interest. The authors have full control of all primary data and agree to allow the journal to review the data if requested.
Rights and permissions
About this article
Cite this article
Hegewald, A.A., Hartmann, S., Keiler, A. et al. Biomechanical investigation of lumbar hybrid stabilization in two-level posterior instrumentation. Eur Spine J 27, 1887–1894 (2018). https://doi.org/10.1007/s00586-017-5415-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5415-x