Abstract
Purpose
The semantics of defining cancer cachexia over the last decade has resulted in uncertainty as to the prevalence. This has further hindered the recognition and subsequent treatment of this condition. Following the consensus definition for cancer cachexia in 2011, there is now a need to establish estimates of prevalence. Therefore, the primary aim of the present study was to assess the prevalence of cachexia in an unselected cancer population. A secondary aim was to assess patient-perceived need of attention to cachexia.
Methods
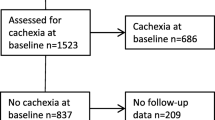
A cross-sectional study in hospital patients was undertaken. Key inclusion criteria were the following: age > 18 years, cancer diagnosis, and no surgery the preceding 24 h. Data on demographics, disease, performance status, symptoms, cachexia, and patients’ perceived need of attention to weight loss and nutrition were registered.
Results
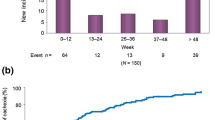
Data were available on 386 of 426 eligible patients. Median age (IQR) was 65 years (56–72), 214 (55%) were male and 302 (78%) had a performance status of 0–1 (Eastern Cooperative Oncology Group). Prevalence of cachexia (inpatients/outpatients) was 51/22%. Prevalence was highest in patients with gastrointestinal cancer (62/42%) and lung cancer (83/36%). There was no major difference in prevalence between patients with metastatic (55/24%) and localized disease (47/19%). Twenty percent of inpatients and 15% of outpatients wanted more attention to weight loss and nutrition. Cachexia (p < 0.001), symptoms of mood disorder (p < 0.001), and male gender (p < 0.01) were independently associated with increased need of attention.
Conclusion
Cachexia is a prevalent condition, affecting both patients with localized and metastatic cancer. Clinical attention to the condition is a sizeable unmet need.

Similar content being viewed by others
References
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N, Mantovani G, Davis M, Muscaritoli M, Ottery F, Radbruch L, Ravasco P, Walsh D, Wilcock A, Kaasa S, Baracos VE (2011) Definition and classification of cancer cachexia: an international consensus. The Lancet Oncology 12(5):489–495. https://doi.org/10.1016/S1470-2045(10)70218-7
Hinsley R, Hughes R (2007) The reflections you get: an exploration of body image and cachexia. Int J Palliat Nurs 13(2):84–89. https://doi.org/10.12968/ijpn.2007.13.2.23068
McClement S (2005) Cancer anorexia-cachexia syndrome: psychological effect on the patient and family. J Wound, Ostomy, Continence Nurs: Off Publ Wound, Ostomy Continence Nurses Soc/ WOCN 32(4):264–268. https://doi.org/10.1097/00152192-200507000-00012
Ross PJ, Ashley S, Norton A, Priest K, Waters JS, Eisen T, Smith IE, O’Brien ME (2004) Do patients with weight loss have a worse outcome when undergoing chemotherapy for lung cancers? Br J Cancer 90(10):1905–1911. https://doi.org/10.1038/sj.bjc.6601781
Tisdale MJ (2002) Cachexia in cancer patients. Nat Rev Cancer 2(11):862–871. https://doi.org/10.1038/nrc927
Farkas J, von Haehling S, Kalantar-Zadeh K, Morley JE, Anker SD, Lainscak M (2013) Cachexia as a major public health problem: frequent, costly, and deadly. J Cachexia Sarcopenia Muscle 4(3):173–178. https://doi.org/10.1007/s13539-013-0105-y
Konishi M, Ishida J, Springer J, Anker SD, von Haehling S (2016) Cachexia research in Japan: facts and numbers on prevalence, incidence and clinical impact. J Cachexia Sarcopenia Muscle 7(5):515–519. https://doi.org/10.1002/jcsm.12117
von Haehling S, Anker SD (2014) Prevalence, incidence and clinical impact of cachexia: facts and numbers-update 2014. J Cachexia Sarcopenia Muscle 5(4):261–263. https://doi.org/10.1007/s13539-014-0164-8
Blum D, Omlin A, Baracos VE, Solheim TS, Tan BH, Stone P, Kaasa S, Fearon K, Strasser F, European Palliative Care Research C (2011) Cancer cachexia: a systematic literature review of items and domains associated with involuntary weight loss in cancer. Crit Rev Oncol Hematol 80(1):114–144. https://doi.org/10.1016/j.critrevonc.2010.10.004
Wallengren O, Lundholm K, Bosaeus I (2013)) Diagnostic criteria of cancer cachexia: relation to quality of life, exercise capacity and survival in unselected palliative care patients. Supportive Care Cancer : Off J Multinatl Assoc Support Care Cancer 21(6):1569–1577. https://doi.org/10.1007/s00520-012-1697-z
Sun L, Quan XQ, Yu S (2015) An epidemiological survey of cachexia in advanced cancer patients and analysis on its diagnostic and treatment status. Nutr Cancer 67(7):1056–1062. https://doi.org/10.1080/01635581.2015.1073753
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, Cohen MH, Douglass HO, Jr., Engstrom PF, Ezdinli EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW, Tormey DC (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 69 (4):491–497, DOI: https://doi.org/10.1016/S0149-2918(05)80001-3
Temel JS, Abernethy AP, Currow DC, Friend J, Duus EM, Yan Y, Fearon KC (2016) Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. The Lancet Oncology 17(4):519–531. https://doi.org/10.1016/S1470-2045(15)00558-6
Hopkinson JB, Wright DN, McDonald JW, Corner JL (2006) The prevalence of concern about weight loss and change in eating habits in people with advanced cancer. J Pain Symptom Manag 32(4):322–331. https://doi.org/10.1016/j.jpainsymman.2006.05.012
Reid J, McKenna HP, Fitzsimons D, McCance TV (2010) An exploration of the experience of cancer cachexia: what patients and their families want from healthcare professionals. Eur J Cancer Care 19(5):682–689. https://doi.org/10.1111/j.1365-2354.2009.01124.x
Millar C, Reid J, Porter S (2013) Healthcare professionals’ response to cachexia in advanced cancer: a qualitative study. Oncol Nurs Forum 40(6):E393–E402. https://doi.org/10.1188/13.onf.e393-e402
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol: Off J Am Soc Clin Oncol 2(3):187–193. https://doi.org/10.1200/JCO.1984.2.3.187
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655. https://doi.org/10.1097/00000421-198212000-00014
Buccheri G, Ferrigno D, Tamburini M (1996) Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer (Oxford, England : 1990) 32a(7):1135–1141
Blum D, Stene GB, Solheim TS, Fayers P, Hjermstad MJ, Baracos VE, Fearon K, Strasser F, Kaasa S, on behalf of E-I (2014) Validation of the consensus-definition for cancer cachexia and evaluation of a classification model—a study based on data from an international multicentre project (EPCRC-CSA). Ann Oncol: Off J Eur Soc Med Oncol/ ESMO 25(8):1635–1642. https://doi.org/10.1093/annonc/mdu086
Bauer J, Capra S, Ferguson M (2002) Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr 56(8):779–785. https://doi.org/10.1038/sj.ejcn.1601412
Klepstad P, Loge JH, Borchgrevink PC, Mendoza TR, Cleeland CS, Kaasa S (2002) The Norwegian brief pain inventory questionnaire: translation and validation in cancer pain patients. J Pain Symptom Manag 24(5):517–525. https://doi.org/10.1016/S0885-3924(02)00526-2
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace EP (1993) Development of a fatigue scale. J Psychosom Res 37(2):147–153. https://doi.org/10.1016/0022-3999(93)90081-P
Kroenke K, Spitzer RL, Williams JB, Lowe B (2009) An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 50(6):613–621. https://doi.org/10.1176/appi.psy.50.6.613
Thronaes M, Raj SX, Brunelli C, Almberg SS, Vagnildhaug OM, Bruheim S, Helgheim B, Kaasa S, Knudsen AK (2016) Is it possible to detect an improvement in cancer pain management? A comparison of two Norwegian cross-sectional studies conducted 5 years apart. Support Care Cancer : Off J Multinatl Assoc Support Care Cancer 24(6):2565–2574. https://doi.org/10.1007/s00520-015-3064-3
Kritchevsky SB, Wilcosky TC, Morris DL, Truong KN, Tyroler HA (1991) Changes in plasma lipid and lipoprotein cholesterol and weight prior to the diagnosis of cancer. Cancer Res 51(12):3198–3203
Fearon K, Arends J, Baracos V (2013) Understanding the mechanisms and treatment options in cancer cachexia. Nature reviews. Clin Oncol 10(2):90–99. https://doi.org/10.1038/nrclinonc.2012.209
Martignoni ME, Dimitriu C, Bachmann J, Krakowski-Rosen H, Ketterer K, Kinscherf R, Friess H (2009) Liver macrophages contribute to pancreatic cancer-related cachexia. Oncol Rep 21(2):363–369
Oberholzer R, Hopkinson JB, Baumann K, Omlin A, Kaasa S, Fearon KC, Strasser F (2013) Psychosocial effects of cancer cachexia: a systematic literature search and qualitative analysis. J Pain Symptom Manag 46(1):77–95. https://doi.org/10.1016/j.jpainsymman.2012.06.020
Skulason B, Hauksdottir A, Ahcic K, Helgason AR (2014) Death talk: gender differences in talking about one’s own impending death. BMC Palliative Care 13(1):8. https://doi.org/10.1186/1472-684x-13-8
Hui D, Kim YJ, Park JC, Zhang Y, Strasser F, Cherny N, Kaasa S, Davis MP, Bruera E (2015) Integration of oncology and palliative care: a systematic review. Oncologist 20(1):77–83. https://doi.org/10.1634/theoncologist.2014-0312
Blauwhoff-Buskermolen S, Langius JAE, Becker A, Verheul HMW, de van der Schueren MAE (2017) The influence of different muscle mass measurements on the diagnosis of cancer cachexia. J Cachexia Sarcopenia Muscle 8(4):615–622. https://doi.org/10.1002/jcsm.12200
Funding
This study has received funding from the Cancer Fund at St. Olav’s Hospital—Trondheim University Hospital and The Liaison Committee for education, research, and innovation in Central Norway. Additionally, the European Palliative Care Research Centre has received unrestricted grants from The Norwegian Cancer Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in this study were in accordance with the ethical standards of the regional ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Stein Kaasa reports stock ownership in Eir Soloutions AS. Barry Laird reports personal fees from Chugai, outside the submitted work. Ola Magne Vagnildhaug, Trude Rakel Balstad, Sigrun Saur Almberg, Cinzia Brunelli, Anne Kari Knudsen, Morten Thronæs, and Tora Skeidsvoll Solheim have nothing to disclose.
Rights and permissions
About this article
Cite this article
Vagnildhaug, O.M., Balstad, T.R., Almberg, S.S. et al. A cross-sectional study examining the prevalence of cachexia and areas of unmet need in patients with cancer. Support Care Cancer 26, 1871–1880 (2018). https://doi.org/10.1007/s00520-017-4022-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-4022-z