Abstract
Purpose
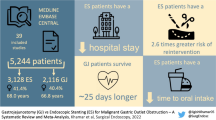
Gastrointestinal obstruction presents many burdens for patients with end-stage abdominal cancer, such as nausea and vomiting. Few detailed data on the efficacy of a percutaneous endoscopic gastrostomy (PEG) for decompression exists. This retrospective cohort study investigates the quantity of symptom relief realized with PEG and the corresponding complications.
Methods
Chart reviews of 75 patients with malignant gastrointestinal obstruction, who received a PEG for decompression, were performed. Abstracted data includes symptoms (vomiting, nausea, abdominal pain) and medication up to 7 days before and after the intervention, complications, demographics, potential influencing factors and survival. Generalized estimating equations (GEE) models determined symptom reduction.
Results
PEG decreased the mean frequency of vomiting per day from 2.2 (95% confidence interval (CI) 1.7–2.7) to 0.4 (95% CI 0.3–0.6) (p < 0.001). The probability of the occurrence of nausea on a given day was 80% (95% CI 74–85%) prior to the PEG placement and 40% (95% CI 34–47%) afterwards (p < 0.001). One hundred twelve complications were reported in 56 patients (none 19/75 patients (25%), minor 52/75 (69%), major 18/75 (24%)). Stomal leakage (18/75 patients), mild wound pain (17/75) and tube occlusion (13/75) occurred most frequently. The failure of the first attempt of the PEG placement (7/75) presented as the leading major complication.
Conclusions
The PEG for decompression significantly reduces vomiting and nausea in patients with malignant gastrointestinal obstruction (p < 0.001). Minor complications are common and should be discussed prior to the intervention. Nevertheless, the PEG appears to demonstrate prevailing benefits in comparison to the risks.

Similar content being viewed by others
References
Tuca A, Guell E, Martinez-Losada E, Codorniu N (2012) Malignant bowel obstruction in advanced cancer patients: epidemiology, management, and factors influencing spontaneous resolution. Cancer Manag Res 4:159–169. doi:10.2147/CMAR.S29297
Roeland E, von Gunten CF (2009) Current concepts in malignant bowel obstruction management. Curr Oncol Rep 11(4):298–303
Ripamonti CI, Easson AM, Gerdes H (2008) Management of malignant bowel obstruction. Eur J Cancer 44(8):1105–1115. doi:10.1016/j.ejca.2008.02.028
Tradounsky G (2012) Palliation of gastrointestinal obstruction. Can Fam Physician 58(6):648–652
Dolan EA (2011) Malignant bowel obstruction: a review of current treatment strategies. Am J Hosp Palliat Care 28(8):576–582. doi:10.1177/1049909111406706
DeEulis TG, Yennurajalingam S (2015) Venting gastrostomy at home for symptomatic management of bowel obstruction in advanced/recurrent ovarian malignancy: a case series. J Palliat Med 18(8):722–728. doi:10.1089/jpm.2014.0355
Zucchi E, Fornasarig M, Martella L, Maiero S, Lucia E, Borsatti E, Balestreri L, Giorda G, Annunziata MA, Cannizzaro R (2016) Decompressive percutaneous endoscopic gastrostomy in advanced cancer patients with small-bowel obstruction is feasible and effective: a large prospective study. Support Care Cancer 24(7):2877–2882. doi:10.1007/s00520-016-3102-9
Issaka RB, Shapiro DM, Parikh ND, Mulcahy MF, Komanduri S, Martin JA, Keswani RN (2014) Palliative venting percutaneous endoscopic gastrostomy tube is safe and effective in patients with malignant obstruction. Surg Endosc 28(5):1668–1673. doi:10.1007/s00464-013-3368-7
Kawata N, Kakushima N, Tanaka M, Sawai H, Imai K, Hagiwara T, Takao T, Hotta K, Yamaguchi Y, Takizawa K, Matsubayashi H, Ono H (2014) Percutaneous endoscopic gastrostomy for decompression of malignant bowel obstruction. Dig Endosc 26(2):208–213. doi:10.1111/den.12139
Rath KS, Loseth D, Muscarella P, Phillips GS, Fowler JM, O’Malley DM, Cohn DE, Copeland LJ, Eisenhauer EL, Salani R (2013) Outcomes following percutaneous upper gastrointestinal decompressive tube placement for malignant bowel obstruction in ovarian cancer. Gynecol Oncol 129(1):103–106. doi:10.1016/j.ygyno.2013.01.021
Pothuri B, Montemarano M, Gerardi M, Shike M, Ben-Porat L, Sabbatini P, Barakat RR (2005) Percutaneous endoscopic gastrostomy tube placement in patients with malignant bowel obstruction due to ovarian carcinoma. Gynecol Oncol 96(2):330–334
Brooksbank MA, Game PA, Ashby MA (2002) Palliative venting gastrostomy in malignant intestinal obstruction. Palliat Med 16(6):520–526
Campagnutta E, Cannizzaro R, Gallo A, Zarrelli A, Valentini M, De Cicco M, Scarabelli C (1996) Palliative treatment of upper intestinal obstruction by gynecological malignancy: the usefulness of percutaneous endoscopic gastrostomy. Gynecol Oncol 62(1):103–105
Marks WH, Perkal MF, Schwartz PE (1993) Percutaneous endoscopic gastrostomy for gastric decompression in metastatic gynecologic malignancies. Surg Gynecol Obstet 177(6):573–576
Herman LL, Hoskins WJ, Shike M (1992) Percutaneous endoscopic gastrostomy for decompression of the stomach and small bowel. Gastrointest Endosc 38(3):314–318
Shaw C, Bassett RL, Fox PS, Schmeler KM, Overman MJ, Wallace MJ, Gupta S, Tam A (2013) Palliative venting gastrostomy in patients with malignant bowel obstruction and ascites. Ann Surg Oncol 20(2):497–505. doi:10.1245/s10434-012-2643-5
Raghunathan TW, Lepkowksi JM, Van Hoewyk J et al (2001) A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology 27:85–95
R Core Team (2015) R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria. Available from: http://www.R-project.org/.
Sacks D, McClenny TE, Cardella JF, Lewis CA (2003) Society of Interventional Radiology clinical practice guidelines: introduction. J Vasc Interv Radiol 14:199–202
Jolicoeur L, Faught W (2003) Managing bowel obstruction in ovarian cancer using a percutaneous endoscopic gastrostomy (PEG) tube. Can Oncol Nurs J 13(4):212–219
Vashi PG, Dahlk S, Vashi RP, Gupta D (2011) Percutaneous endoscopic gastrostomy tube occlusion in malignant peritoneal carcinomatosis-induced bowel obstruction. Eur J Gastroenterol Hepatol 23(11):1069–1073. doi:10.1097/MEG.0b013e32834b0e2a
Diver E, O’Connor O, Garrett L, Boruta D, Goodman A, Del Carmen M, Schorge J, Mueller P, Growdon W (2013) Modest benefit of total parenteral nutrition and chemotherapy after venting gastrostomy tube placement. Gynecol Oncol 129(2):332–335. doi:10.1016/j.ygyno.2013.02.002
Van Hooft JE, Dijkgraaf MG, Timmer R, Siersema PD, Fockens P (2010) Independent predictors of survival in patients with incurable malignant gastric outlet obstruction: a multicenter prospective observational study. Scand J Gastroenterol 45(10):1217–1222. doi:10.3109/00365521.2010.487916
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the institutional review board at the Technical University Dresden (EK 102032014).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Dittrich, A., Schubert, B., Kramer, M. et al. Benefits and risks of a percutaneous endoscopic gastrostomy (PEG) for decompression in patients with malignant gastrointestinal obstruction. Support Care Cancer 25, 2849–2856 (2017). https://doi.org/10.1007/s00520-017-3700-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3700-1