Abstract
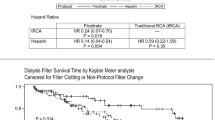
Recent years has seen an increasing use of regional citrate anticoagulation in pediatric dialysis. Several approaches have been described for monitoring anticoagulation in the extracorporeal circuit, such as serum citrate levels, post-filter ionized calcium (iCa), and activated coagulation time (ACT). However, no standard recommendations have yet been established for applying any of these parameters, especially for iCa. The objective of this retrospective analysis was to establish adequate coagulation management using post-filter iCa values. Normal values for ACTester-based ACT were established using a group of 64 children who were divided into two subgroups, with one subgroup comprising children without chronic kidney disease or coagulation disorder (age 1.2–17.5 years, median 9.7 years) and one consisting of 32 uremic patients (age 0.6–17.5 years, median 13.7 years). In a second group of 13 patients (aged 7–17 years), all of whom were undergoing high-flux dialysis (HD) with regional citrate anticoagulation (RCA), we assessed 73 post-filter blood samples for ionized calcium and ACT. A receiver operating characteristic graph was used to identify the iCa threshold needed to achieve adequate anticoagulation. Normal values for ACT were 90 s [2 standard deviations (SD) 72–109] in healthy children and 94 s (2 SD 75–113) in the uremic children. There was no statistically significant difference between the groups. In the children undergoing HD with RCA, the post-filter iCa level correlated with ACT (r = −0.94, p < 0.001). A post-filter iCa level of ≤0.30 mmol/l reliably predicted an ACT >120 s. Our citrate protocol [citrate 3% rate (ml/h) ≈ blood flow rate (ml/min) × 2] meets the established criteria with a high sensitivity. Based on these results, we conclude that the post-filter iCa level can be reliably used for the management of extracorporeal anticoagulation with citrate in pediatric HD. We recommend the application of our citrate prescription protocol in the setting of pediatric intermittent hemodialysis.


Similar content being viewed by others
Abbreviations
- ACD:
-
Anticoagulant citrate dextrose
- ACT:
-
Activated coagulation time
- CRRT:
-
Continuous renal replacement therapy
- iCa:
-
Ionized calcium
- iHD:
-
Intermittent hemodialysis
- PTT:
-
Partial thromboplastin time
- RCA:
-
Regional citrate anticoagulation
References
Morita Y, Johnson RW, Dorn RE, Hall DS (1961) Regional anticoagulation during hemodialysis using citrate. Am J Med Sci 242:32–43
Pinnick RV, Wiegmann TB, Diederich DA (1983) Regional citrate anticoagulation for hemodialysis in the patient at high risk for bleeding. N Engl J Med 308:258–261
Mehta R, McDonald B, Aguilar M, Ward DM (1990) Regional citrate anticoagulation for continuous arteriovenous hemodialysis in critically ill patients. Kidney Int 38:976–981
Gubensek J, Buturovic-Ponikvar J, Ponikvar R (2007) Regional citrate anticoagulation for single-needle hemodialysis: a prospective clinical study. Blood Purif 25:454–456
Schneider M, Thomas K, Liefeldt L, Kindgen-Milles D, Peters H, Neumayer HH, Morgera S (2007) Efficacy and safety of intermittent hemodialysis using citrate as anticoagulant: a prospective study. Clin Nephrol 68:302–307
Bunchman TE, Maxvold NJ, Barnett J, Hutchings A, Benfield MR (2002) Pediatric hemofiltration. Normocarb dialysate solution with citrate anticoagulation. Pediatr Nephrol 17:150–154
Bunchman TE, Maxvold NJ, Brophy PD (2003) Pediatric convective hemofiltration: Normocarb replacement fluid and citrate anticoagulation. Am J Kidney Dis 42:1248–1252
Chadha V, Garg U, Warady BA, Alon US (2002) Citrate clearance in children receiving continuous venovenous renal replacement therapy. Pediatr Nephrol 17:819–824
Elhanan N, Skippen P, Nuthall G, Krahn G, Seear M (2004) Citrate anticoagulation in pediatric continuous venovenous hemofiltration. Pediatr Nephrol 19:208–212
Symons JM, Chua AN, Somers MJ, Baum MA, Bunchman TE, Benfield MR, Brophy PD, Blowey D, Fortenberry JD, Chand D, Flores FX, Hackbarth R, Alexander SR, Mahan J, McBryde KD, Goldstein SL (2007) Demographic characteristics of pediatric continuous renal replacement therapy: a report of the prospective pediatric continuous renal replacement therapy registry. Clin J Am Soc Nephrol 2:732–738
Ward DM (1997) The approach to anticoagulation in patients treated with extracorporeal therapy in the intensive care unit. Adv Ren Replace Ther 4:160–173
Ataullakhanov F, Pohilko A, Sinauridze E (1994) Calcium threshold in human plasma clotting kinetics. Thromb Res 75:383–394
Calatzis A, Toepfer M, Schramm W, Spannagl M, Schiffl H (2001) Citrate anticoagulation for extracorporeal circuits: effects on whole blood coagulation activation and clot formation. Nephron 89:233–236
Hattersley PG (1966) Activated coagulation time of whole blood. JAMA 196:436–440
Taneja R, Fernandes P, Marwaha G, Cheng D, Bainbridge D (2008) Perioperative coagulation management and blood conservation in cardiac surgery: a Canadian Survey. J Cardiothorac Vasc Anesth 22:662–669
Slight RD, Buell R, Nzewi OC, McClelland DB, Mankad PS (2008) A comparison of activated coagulation time-based techniques for anticoagulation during cardiac surgery with cardiopulmonary bypass. J Cardiothorac Vasc Anesth 22:47–52
Martindale SJ, Shayevitz JR, D’Errico C (1996) The activated coagulation time: suitability for monitoring heparin effect and neutralization during pediatric cardiac surgery. J Cardiothorac Vasc Anesth 10:458–463
Hattersley PG (1971) The activated coagulation time of whole blood as a routine pre-operative sceening test. Calif Med 114:15–18
Siskin GP, Reiner E, Stainken BF, Dowling K, Dolen EG, Quarfordt S, Albons G (2001) Activated clotting time as a screening test prior to catheter-based cardiovascular procedures. Catheter Cardiovasc Interv 54:191–195
Davenport A (2003) Anticoagulation options for pediatric hemodialysis. Hemodial Int 7:168–176
Rani TR, Gopinath R (2008) An unusual cause of a prolonged activated coagulation time during cardiac surgery: congenital hypofibrinogenemia. J Cardiothorac Vasc Anesth 22:725–726
Chang RJ, Doherty TM, Goldberg SL (1998) How does warfarin affect the activated coagulation time? Am Heart J 136:477–479
Stefanidis I, Hägel J, Maurin N (1995) Influence of coagulation parameters on filter running time during continuous venovenous hemofiltration. Contrib Nephrol 116:145–149
Lord H, Jean N, Dumont M, Kassis J, Leblanc M (2002) Comparison between tinzaparin and standard heparin for chronic hemodialysis in a Canadian center. Am J Nephrol 22:58–66
Hörl WH (2006) Thrombocytopathy and bleeding complications in Uremia. Wien Klin Wochenschr 118:134–150
Nuthall G, Skippen P, Daoust C, Al-Jofan F, Seear M (2002) Citrate anticoagulation in a piglet model of pediatric continuous renal replacement therapy. Crit Care Med 30:900–903
Bakker AJ, Boerma EC, Keidel H, Kingma P, van der Voort PH (2006) Detection of citrate overdose in critically ill patients on citrate-anticoagulated venovenous hemofiltration: use of ionized and total/ionized calcium. Clin Chem Lab Med 44:962–966
Opatrný K, Richtrová P, Polanská K, Wirth J, Sefrna F, Brandl M, Falkenhagen D (2007) Citrate anticoagulation control by ionized calcium levels does not prevent hemostasis and complement activation during hemodialysis. Artif Organs 31:200–207
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kreuzer, M., Ahlenstiel, T., Kanzelmeyer, N. et al. Management of regional citrate anticoagulation in pediatric high-flux dialysis: activated coagulation time versus post-filter ionized calcium. Pediatr Nephrol 25, 1305–1310 (2010). https://doi.org/10.1007/s00467-010-1483-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1483-4