Abstract
Background
Endoscopic retrograde cholangiopancreatography (ERCP) for extraction of common bile duct (CBD) stones in Billroth II anatomy patients is still a technical challenge and factors affecting stone extraction have not yet been clarified. This study aimed to analyze our experience and evaluate potential factors affecting CBD stone extraction.
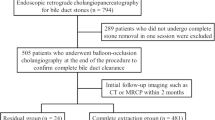
Methods
A retrospective analysis of CBD stones patients with a history of Billroth II gastrectomy, who underwent therapeutic ERCP for stone extraction at our center from August 1999 to December 2017, was conducted. The outcomes of ERCP and potential factors affecting stone extraction were examined.
Results
A total of 227 patients were enrolled, and 176 patients (77.5%) achieved technical success. The success rate of duodenal ampullary access and selective biliary cannulation was 84.1% (191/227) and 92.1% (176/191), respectively. The mean CBD diameter was 15 mm (range 6–35 mm), and the largest stone size was 13 mm (range 4–36 mm). CBD stones were ultimately removed in 137 patients (77.8%), and 105 patients (59.7%) for the first session. Mechanical lithotripsy was used in 17 patients (9.7%). The overall ERCP-related complication rate was 6.3% (11/176), including bleeding in 3 patients (1.7%) and mild pancreatitis in 6 patients (3.4%). The multivariate analysis indicated that CBD stone number ≥ 2 (OR 2.171; 95% CI 1.095–4.306; p = 0.027), and the largest CBD stone size ≥ 12 mm (OR 3.646; 95% CI 1.833–7.251; p < 0.001) were patient-related risk factors for failed stone removal; while the use of endoscopic papillary (large) balloon dilation (EPBD/EPLBD) (OR 0.291; 95% CI 0.147–0.576; p < 0.001) was a procedure-related protective factor for successful stone extraction.
Conclusions
ERCP is safe and effective for extraction of CBD stones in Billroth II anatomy patients. The number and the largest size of CBD stones, and the use of EPBD/EPLBD are predictive factors for CBD stone extraction.
Similar content being viewed by others
References
Bove V, Tringali A, Familiari P et al (2015) ERCP in patients with prior Billroth II gastrectomy: report of 30 years’ experience. Endoscopy 47(7):611–616
Park TY, Kang JS, Song TJ et al (2016) Outcomes of ERCP in Billroth II gastrectomy patients. Gastrointest Endosc 83(6):1193–1201
Li JS, Zou DW, Jin ZD et al (2019) Endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients: outcomes and potential factors affecting technical failure. Saudi J Gastroenterol. https://doi.org/10.4103/sjg.sjg_118_19
Cotton PB, Eisen GM, Aabakken L et al (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71(3):446–454
Choi CW, Choi JS, Kang DH et al (2012) Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol 27(2):256–260
Jang HW, Lee KJ, Jung MJ et al (2013) Endoscopic papillary large balloon dilatation alone is safe and effective for the treatment of difficult choledocholithiasis in cases of Billroth II gastrectomy: a single center experience. Dig Dis Sci 58(6):1737–1743
Kim KH, Kim TN (2014) Endoscopic papillary large balloon dilation for the retrieval of bile duct stones after prior Billroth II gastrectomy. Saudi J Gastroenterol 20(2):128–133
Ogura T, Higuchi K (2016) A review of treatment options for bile duct stones. Expert Rev Gastroenterol Hepatol 10(11):1271–1278
Williams EJ, Ogollah R, Thomas P et al (2012) What predicts failed cannulation and therapy at ERCP? Results of a large-scale multicenter analysis. Endoscopy 44(7):674–683
Doshi B, Yasuda I, Ryozawa S et al (2018) Current endoscopic strategies for managing large bile duct stones. Dig Endosc 30(Suppl 1):59–66
Nakai Y, Kogure H, Yamada A et al (2018) Endoscopic management of bile duct stones in patients with surgically altered anatomy. Dig Endosc 30(Suppl 1):67–74
Ödemiş B, Kuzu UB, Öztaş E et al (2016) Endoscopic management of the difficult bile duct stones: a Single tertiary center experience. Gastroenterol Res Pract 2016:8749583
Lee SH, Park JK, Yoon WJ et al (2007) How to predict the outcome of endoscopic mechanical lithotripsy in patients with difficult bile duct stones? Scand J Gastroenterol 42(8):1006–1010
Williams E, Beckingham I, El Sayed G et al (2017) Updated guideline on the management of common bile duct stones (CBDS). Gut 66(5):765–782
Testoni PA, Mariani A, Aabakken L et al (2016) Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 48(7):657–683
Bergman JJ, van Berkel AM, Bruno MJ et al (2001) A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc 53(1):19–26
Park CH, Jung JH, Nam E et al (2018) Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc 87(1):43–57
Dong SQ, Singh TP, Zhao Q et al (2019) Sphincterotomy plus balloon dilation versus sphincterotomy alone for choledocholithiasis: a meta-analysis. Endoscopy. https://doi.org/10.1055/a-0848-8271
Aujla UI, Ladep N, Dwyer L et al (2017) Endoscopic papillary large balloon dilatation with sphincterotomy is safe and effective for biliary stone removal independent of timing and size of sphincterotomy. World J Gastroenterol 23(48):8597–8604
Tringali A, Rota M, Rossi M et al (2019) A cumulative meta-analysis of endoscopic papillary balloon dilation versus endoscopic sphincterotomy for removal of common bile duct stones. Endoscopy 51:548–559. https://doi.org/10.1055/a-0818-3638
Dumonceau JM, Tringali A, Papanikolaou IS et al (2018) Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated October 2017. Endoscopy 50(9):910–930
Mohammed N, Pinder M, Harris K et al (2016) Endoscopic biliary stenting in irretrievable common bile duct stones: stent exchange or expectant management-tertiary-centre experience and systematic review. Frontline Gastroenterol 7(3):176–186
Akazawa Y, Ohtani M, Nosaka T et al (2018) Long-term prognosis after biliary stenting for common bile duct stones in high-risk elderly patients. J Dig Dis 19(10):626–634
Horiuchi A, Nakayama Y, Kajiyama M et al (2010) Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc 71(7):1200–1203
Attaallah W, Cingi A, Karpuz S et al (2016) Do not rush for surgery; stent placement may be an effective step for definitive treatment of initially unextractable common bile duct stones with ERCP. Surg Endosc 30(4):1473–1479
Author information
Authors and Affiliations
Contributions
Study conception and design (FL, ZL); acquisition, analysis, and interpretation of data (JL); drafting of the manuscript (JL); critical revision of the manuscript for important intellectual content (FL, LZ); technical or material support (DZ, ZJ, XS, JC, ZL, and FL); study supervision (FL, ZL). The article has been approved by all authors to be published.
Corresponding authors
Ethics declarations
Disclosures
Jia-su Li, Duo-wu Zou, Zhen-dong Jin, Xin-gang Shi, Jie Chen, Zhao-shen Li, and Feng Liu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Js., Zou, Dw., Jin, Zd. et al. Predictive factors for extraction of common bile duct stones during endoscopic retrograde cholangiopancreatography in Billroth II anatomy patients. Surg Endosc 34, 2454–2459 (2020). https://doi.org/10.1007/s00464-019-07039-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07039-8