Abstract
Background
Failure or complications following laparoscopic adjustable gastric banding (LAGB) may necessitate band removal and conversional surgery. Band position and band-induced chronic vomiting create ideal conditions for de novo hiatal hernia (HH) formation. HH presence impedes and complicates conversional surgery by obscuring crucial anatomical landmarks and hindering precise gastric sleeve or pouch formation. The aim of this study was to evaluate the incidence of a HH in patients with an LAGB undergoing conversion compared to patients undergoing primary bariatric surgery (BS).
Methods
Retrospective review of consecutive BS performed between 2010 and 2015. Data collected included demographics, anthropometrics, comorbidities, previous BS, preoperative and intra-operative HH detection, operation time, perioperative complications and length of hospital stay.
Results
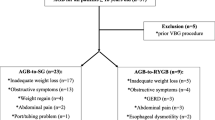
During the study period, 2843 patients (36% males) underwent BS. Of these, 2615 patients (92%) were “primary” (no previous BS—control group), 197 (7%) had a previous LAGB (study group), and 31 (1%) had a different previous BS and were excluded. Reasons for conversion included weight regain, band intolerance and band-related complications. Mean age and body mass index were similar between the study and the control groups. HH was preoperatively diagnosed by upper gastrointestinal (UGI) fluoroscopy in 9.1% and 9.0% of the LAGB and control groups (p = NS), respectively. However, HH was detected intra-operatively in 20.3% and 7.3%, respectively (p < 0.0001).
Conclusions
Preoperative diagnosis of a HH by UGI fluoroscopy for patients who have undergone LAGB is unreliable. Intra-operative hiatal exploration is highly recommended in all cases of conversional BS after LAGB.
Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25:1822–1832
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Livingston EH (2010) The incidence of bariatric surgery has plateaued in the U.S. Am J Surg 200:378–385
Brown WA, Burton PR, Anderson M, Korin A, Dixon JB, Hebbard G, O’Brien PE (2008) Symmetrical pouch dilatation after laparoscopic adjustable gastric banding: incidence and management. Obes Surg 18:1104–1108
Eid I, Birch DW, Sharma AM, Sherman V, Karmali S (2011) Complications associated with adjustable gastric banding for morbid obesity: a surgeon’s guides. Can J Surg 54:61–66
Mittermair RP, Aigner F, Nehoda H (2004) Results and complications after laparoscopic adjustable gastric banding in super-obese patients, using the Swedish band. Obes Surg 14:1327–1330
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA (2013) Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257:87–94
Goitein D, Feigin A, Segal-Lieberman G, Goitein O, Papa MZ, Zippel D (2011) Laparoscopic sleeve gastrectomy as a revisional option after gastric band failure. Surg Endosc 25:2626–2630
Lazzati A, De Antonio M, Paolino L, Martini F, Azoulay D, Iannelli A, Katsahian S (2017) Natural history of adjustable gastric banding: lifespan and revisional rate: a nationwide study on administrative data on 53,000 patients. Ann Surg 265:439–445
Victorzon M, Tolonen P (2013) Mean fourteen-year, 100% follow-up of laparoscopic adjustable gastric banding for morbid obesity. Surg Obes Relat Dis 9:753–757
Azagury DE, Varban O, Tavakkolizadeh A, Robinson MK, Vernon AH, Lautz DB (2013) Does laparoscopic gastric banding create hiatal hernias? Surg Obes Relat Dis 9:48–52
Goitein D, Sakran N, Rayman S, Szold A, Goitein O, Raziel A (2017) Barium swallow for hiatal hernia detection is unnecessary prior to primary sleeve gastrectomy. Surg Obes Relat Dis 13:138–142
Keidar A, Appelbaum L, Schweiger C, Elazary R, Baltasar A (2010) Dilated upper sleeve can be associated with severe postoperative gastroesophageal dysmotility and reflux. Obes Surg 20:140–147
Nedelcu M, Noel P, Iannelli A, Gagner M (2015) Revised sleeve gastrectomy (re-sleeve). Surg Obes Relat Dis 11:1282–1288
Goitein D, Raziel A, Szold A, Sakran N (2016) Assessment of perioperative complications following primary bariatric surgery according to the Clavien-Dindo classification: comparison of sleeve gastrectomy and Roux-Y gastric bypass. Surg Endosc 30:273–278
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H, Scopinaro N (2017) Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg 27:2279–2289
Losh JM, Sanchez B, Waxman K (2017) Refractory pseudoachalasia secondary to laparoscopically placed adjustable gastric band successfully treated with Heller myotomy. Surg Obes Relat Dis 13:e4–e8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. S. Rayman, M. Goldenshluger, O. Goitein, J. Dux, N. Sakran, A. Raziel and D. Goitein have no financial or commercial conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Rayman, S., Goldenshluger, M., Goitein, O. et al. Conversion for failed adjustable gastric banding warrants hiatal scrutiny for hiatal hernia. Surg Endosc 33, 2231–2234 (2019). https://doi.org/10.1007/s00464-018-6509-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6509-1