Abstract
Background
Objective assessment of the difficulty of laparoscopic liver resection (LLR) preoperatively is key in improving its uptake. Difficulty scores are proposed but are not used routinely in practice. We identified and appraised predictive models to estimate LLR difficulty.
Methods
We systematically searched the literature for tools predicting LLR difficulty. Two independent reviewers selected studies, abstracted data and assessed methodology. We evaluated tools’ quality and clinical relevance using the Critical Appraisal and Data Extraction for Systematic Reviews of Prediction Modelling Studies (CHARMS) guidelines.
Results
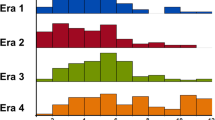
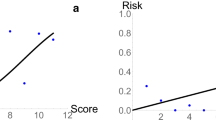
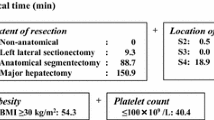
From 1037 citations, we included 8 studies reporting on 4 predictive tools using data from 1995 to 2016 in Asia and Europe. In 4 development studies, tools were designed to predict difficulty as assigned by experts using a 10-level difficulty index, operative time, post-operative morbidity or intra-operative complications. Internal validation and performance metrics were reported in one development study. One tool was subjected to external validations in 4 studies (1 independent and geographic). Validations compared post-operative outcomes (operative time, blood loss, transfusion, major morbidity and conversion) between the risk categories. One study validated discrimination (AUROC 0.53). Calibration was not assessed.
Conclusion
Existing tools cannot be used confidently to predict LLR difficulty. Consistent objective clinical outcomes to predict to define LLR difficulty should be established, and better-quality tools developed and validated in a wide array of populations and clinical settings, following best practices for predictive tools development and validation. This will improve risk stratification for future trials and uptake of LLR.

Similar content being viewed by others
References
Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, Abdalla EK, Curley SA, Capussotti L, Clary BM, Vauthey JN (2007) Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am College Surg 204:854–862
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 236:397–406 (Discussion 406–7)
Sauerland S, Lefering R, Neugebauer EA (2004) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 4:CD001546
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 363:1187–1192
Lujan J, Valero G, Biondo S, Espin E, Parilla P (2013) Laparoscopic versus open surgery for rectal cancer: results of a prospective multicentre analysis of 4,970 patients. Surg Endosc 27:295–302
Ogiso S, Nomi T, Araki K, Conrad C, Hatano E, Uemoto S, Fuks D, Gayet B (2015) Laparoscopy-specific surgical concepts for hepatectomy based on the laparoscopic caudal view: a key to reboot surgeons’ minds. Ann Surg Oncol 22(Suppl 3):S327–S333
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B (2015) Learning curve for laparoscopic major hepatectomy. Br J Surg 102:796–804
Dagher I, Belli G, Fantini C, Laurent S, Tayar C, Lainas P, Tranchart H, Franco D, Cherqui D (2010) Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg 211:16–23
Nguyen KT, Gamblin TC, Geller D (2009) World review of laparoscopic liver resection—2,804 patients. Ann Surg 250:831–841
Wakabayashi G (2015) From Louisville to Morioka: where is now MILS? Updates Surg 67:101–104
Goutte N, Bendersky N, Barbier L, Falissard B, Farges O (2017) Laparoscopic left lateral sectionectomy: a population-based study. HPB 19:118–125
Varley PR, Tohme ST, Chidi AP, Goswami J, van der Windt D, Geller DA, Tsung A (2018) Dissemination of minimally invasive liver resection for primary malignancy: reevaluating effectiveness. Ann Surg Oncol 25:808–817
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, OʼRourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CHD, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen K-H, Schön MR, Sugioka A, Tang C-N, Herman P, Pekolj J, Chen X-P, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien P-A, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261(4):619–629
Ban D, Kudo A, Ito H, Mitsunori Y, Matsumura S, Aihara A, Ochiai T, Tanaka S, Tanabe M, Itano O, Kaneko H, Wakabayashi G (2015) The difficulty of laparoscopic liver resection. Updates Surg 67(2):123–128. https://doi.org/10.1007/s13304-015-0302-7
Allard M-A, Cunha AS, Gayet B, Adam R, Goere D, Bachellier P, Azoulay D, Ayav A, Navarro F, Pessaux P (2015) Early and long-term oncological outcomes after laparoscopic resection for colorectal liver metastases. Ann Surg 262:794–802
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepato-Biliary-Pancreat Sci 21:745–753
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2017) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267(1):13–17
Halls MC, Cherqui D, Taylor MA, Primrose JN, Hilal MA, Aldrighetti L, Saati Al H, Alseidi A, Aroori S, Belli G, Besselink M, Edwin B, D’Hondt M, Dagher I, Dejong C, Geller D, Hamady Z, Hamoui M, Isaksson B, Ivanecz A, Le Roux G, Lesurtel M, O’Rouke N, Prasad R, Calvo MP, Reddy S, Rotellar F, Santoyo J, Soonawalla Z, Soubrane O, Stavrou G, Subar D, Sutcliffe R, Tanis P, Troisi R, Van Dam R, Wakabayashi G, White S (2017) Are the current difficulty scores for laparoscopic liver surgery telling the whole story? An international survey and recommendations for the future. HPB 20(3):231–236
Hasegawa Y, Wakabayashi G, Nitta H, Takahara T, Katagaru H, Umemura A, Makabe K, Sasaki A (2015) A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc 31(12):5356–5363
Geersing G-J, Bouwmeester W, Zuithoff P, Spijker R, Leeflang M, Moons K (2012) Search filters for finding prognostic and diagnostic prediction studies in medline to enhance systematic reviews. PLoS ONE 7:e32844–e32846
Moons KGM, de Groot JAH, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, Reitsma JB, Collins GS (2014) Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med 11:e1001744–e1001712
Collins GS, Reitsma JB, Altman DG, Moons KGM (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Br J Surg 102:148–158
Mahar AL, Compton C, Halabi S, Hess KR, Gershenwald JE, Scolyer RA, Groome PA (2016) Critical assessment of clinical prognostic tools in melanoma. Ann Surg Oncol 23:2753–2761
Mahar AL, Compton C, Halabi S, Hess KR, Weiser MR, Groome PA (2017) Personalizing prognosis in colorectal cancer: a systematic review of the quality and nature of clinical prognostic tools for survival outcomes. J Surg Oncol 116:969–982
Mahar AL, Compton C, McShane LM, Halabi S, Asamura H, Rami-Porta R, Groome PA, Molecular Modellers Working Group of American Joint Committee on Cancer (2015) Refining prognosis in lung cancer: a report on the quality and relevance of clinical prognostic tools. J Thorac Oncol 10:1576–1589
Moons KGM, Altman DG, Reitsma JB, Ioannidis JPA, Macaskill P, Steyerberg EW, Vickers AJ, Ransohoff DF, Collins GS (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:W1–W73
Hasegawa Y, Wakabayashi G, Nitta H, Takahara T, Katagiri H, Umemura A, Makabe K, Sasaki A (2017) A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc 31:5356–5363
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection. Ann Surg 267:13–17
Uchida H, Iwashita Y, Saga K, Takayama H, Watanabe K, Endo Y, Yada K, Ohta M, Inomata M (2016) Clinical utility of the difficulty scoring system for predicting surgical time of laparoscopic liver resection. J Laparoendosc Adv Surg Tech A 26:702–706
Im C, Cho JY, Han HS, Yoon Y-S, Choi Y, Jang JY, Choi H, Jang JS, Kwon SU (2016) Validation of difficulty scoring system for laparoscopic liver resection in patients who underwent laparoscopic left lateral sectionectomy. Surg Endosc 31:430–436
Tanaka S, Kubo S, Kanazawa A, Takeda Y, Hirokawa F, Nitta H, Nakajima T, Kaizu T, Kaneko H, Wakabayashi G (2017) Validation of a difficulty scoring system for laparoscopic liver resection: a multicenter analysis by the Endoscopic Liver Surgery Study Group in Japan. J Am Coll Surg 225:249–258
Periyasamy M, Cho JY, Ahn S, Han HS, Yoon Y-S, Choi Y, Jang JS, Kwon SU, Kim S, Choi JK, Guro H (2017) Prediction of surgical outcomes of laparoscopic liver resections for hepatocellular carcinoma by defining surgical difficulty. Surg Endosc 31:5209–5218
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240:205–213
Kazaryan AM, Røsok BI, Edwin B (2013) Morbidity assessment in surgery: refinement proposal based on a concept of perioperative adverse events. ISRN Surg 2013:625093–625097
Schlachta CM, Lefebvre KL, Sorsdahl AK, Jayaraman S (2010) Mentoring and telementoring leads to effective incorporation of laparoscopic colon surgery. Surg Endosc 24:841–844
Debray TPA, Vergouwe Y, Koffijberg H, Nieboer D, Steyerberg EW, Moons KGM (2015) A new framework to enhance the interpretation of external validation studies of clinical prediction models. J Clin Epidemiol 68:279–289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Julie Hallet has received speaker honoraria from Ipsen Biopharmaceuticals, Canada, and Novartis Oncology, and is the recipient of the Society of Surgery of the Alimentary Tract (SSAT) Career Development Award for Clinical/Outcomes/Education Research. Shiva Jayaraman has received speaker honoraria from Ethicon, Olympus and Baxter Corporation, and advisory board honoraria from Ipsen Biopharmaceuticals Canada and Pendopharm. Natalie Coburn holds the Sherif and Mary-Lou Hanna Chair in Surgical Oncology Research. Patrick Pessaux, Kaitlyn Beyfuss, Pablo Serrano, Guillaume Martel, Tullio Piardi and Alyson Mahar have no conflict of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hallet, J., Pessaux, P., Beyfuss, K.A. et al. Critical appraisal of predictive tools to assess the difficulty of laparoscopic liver resection: a systematic review. Surg Endosc 33, 366–376 (2019). https://doi.org/10.1007/s00464-018-6479-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6479-3