Abstract
Background
Few studies about long-term glucose homeostasis in bariatric patients are available. In a prospective protocol that included retrospective information, outcome of patients with both impaired and normal fasting blood glucose (FBG) was monitored to assess frequencies and correlates.
Methods
Patients submitted to Roux-en-Y gastric bypass were classified as group I, elevated FBG, and group II, normal controls. Those in group I with improvement in FBG were defined as responsive and the others as refractory. Group II participants progressing to new-onset diabetes (NOD) or prediabetes represented NOD cases; the remaining were listed as stable controls. FBG was the main endpoint, but HbA1c results were considered, along with diet composition and general biochemical profile.
Results
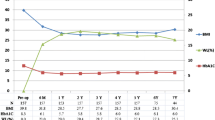
Among 97 selected patients, 51 belonged to group I (52.4 ± 10.5 years, 29.6 % males, initial body mass index (BMI) 58.4 ± 13.4, current BMI 35.1 ± 8.4 kg/m2) and 46 to group II (48.2 ± 10.5 years, 19.6 % males, initial BMI 55.5 ± 8.8, current BMI 33.9 ± 6.9 kg/m2). Follow-up was 7–9 years, and 31.4 % (16/51) of group I were classified as refractory, whereas 15.2 % (7/46) of the controls converted to NOD. Multivariate analysis pointed out higher current BMI, older age, consumption of antidiabetic drugs, and male gender as features of refractory cases, whereas NOD participants were not significantly different from non-progressing controls.
Conclusions
This is the first investigation, to the best of our knowledge, to underscore the correlates of refractory and NOD within the bariatric context. Further studies are recommended as such information could be valuable for patient selection, prognostic scoring, and outcome monitoring.

Similar content being viewed by others
References
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP, Sledge I (2009) Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 122:248–256
Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjostrom CD, Sullivan M, Wedel H (2004) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 351:2683–2693
DiGiorgi M, Rosen DJ, Choi JJ, Milone L, Schrope B, Olivero-Rivera L, Restuccia N, Yuen S, Fisk M, Inabnet WB, Bessler M (2010) Re-emergence of diabetes after gastric bypass in patients with mid- to long-term follow-up. Surg Obes Relat Dis 6:249–253
Gunther K, Vollmuth J, Weissbach R, Hohenberger W, Husemann B, Horbach T (2006) Weight reduction after an early version of the open gastric bypass for morbid obesity: results after 23 years. Obes Surg 16:288–296
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, Barakat HA, de Ramon RA, Israel G, Dolezal JM (1995) Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222:339–350
Long SD, O’Brien K, MacDonald KG Jr, Leggett-Frazier N, Swanson MS, Pories WJ, Caro JF (1994) Weight loss in severely obese subjects prevents the progression of impaired glucose tolerance to type II diabetes. A longitudinal interventional study. Diabetes Care 17:372–375
Al Harakeh AB, Burkhamer KJ, Kallies KJ, Mathiason MA, Kothari SN (2010) Natural history and metabolic consequences of morbid obesity for patients denied coverage for bariatric surgery. Surg Obes Relat Dis 6:591–596
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 34(Suppl 1):S62–S69
Ishida RK, Faintuch J, Kuga R, Ribeiro AS, Sakai P, Barbeiro HV, Barbeiro DF, Soriano FG, Cecconello I (2007) Microbial flora of the stomach after gastric bypass for morbid obesity. Obes Surg 17:752–758
MacDonald KG Jr, Long SD, Swanson MS, Brown BM, Morris P, Dohm GL, Pories WJ (1997) The gastric bypass operation reduces the progression and mortality of non-insulin-dependent diabetes mellitus. J Gastrointest Surg 1:213–220
Sugerman HJ, Wolfe LG, Sica DA, Clore JN (2003) Diabetes and hypertension in severe obesity and effects of gastric bypass induced weight loss. Ann Surg 237:751–756
Higa K, Ho T, Tercero F, Yunus T, Boone KB (2010) Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis 16:1151–1152
Gracia-Solanas JA, Elia M, Aguilella V, Ramirez JM, Martínez J, Bielsa MA, Martínez M (2011) Metabolic syndrome after bariatric surgery. Results depending on the technique performed. Obes Surg 21:179–185
Petrie JR, Pearson ER, Sutherland C (2011) Implications of genome wide association studies for the understanding of type 2 diabetes pathophysiology. Bioche Pharmacol 81:471–477
Rubino F, Gagner M (2002) Potential of surgery for curing type 2 diabetes mellitus. Ann Surg 236:554–559
Hussain A, Mahmood H, El-Hasani S (2009) Can Roux-en-Y gastric bypass provide a lifelong solution for diabetes mellitus? Can J Surg 52:E269–E275
Morais AA, Faintuch J, Leal AA, Noe JA, Bertollo DM, Morais RC, Cabrini D (2011) Inflammation and biochemical features of bariatric candidates: does gender matter? Obes Surg 21:71–77
Dias MCG, Ribeiro AG, Scabim VM, Faintuch J, Zilberstein B, Gama-Rodrigues JJ (2006) Dietary intake of female bariatric patients after anti-obesity gastroplasty. Clinics (Sao Paulo) 61:93–98
Papakonstantinou E, Triantafillidou D, Panagiotakos DB, Koutsovasilis A, Saliaris M, Manolis A, Melidonis A, Zampelas A (2010) A high-protein low-fat diet is more effective in improving blood pressure and triglycerides in calorie-restricted obese individuals with newly diagnosed type 2 diabetes. Eur J Clin Nutr 64:595–602
Acknowledgments
The support of CNPq Research Grant 300392/2008-7 and CAPES Postgraduate Scholarships (CMY and SYH) is appreciated.
Disclosures
C. M. Yamaguchi, J. Faintuch, S. Y. Hayashi, J. J. Faintuch, and I. Cecconello have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamaguchi, C.M., Faintuch, J., Hayashi, S.Y. et al. Refractory and new-onset diabetes more than 5 years after gastric bypass for morbid obesity. Surg Endosc 26, 2843–2847 (2012). https://doi.org/10.1007/s00464-012-2256-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2256-x