Abstract
Background
Traditionally, the common bile duct (CBD) has been closed with T-tube drainage after laparoscopic choledochotomy and removal of CBD stones. However, insertion of the T-tube is related to some potential postoperative complications, and patients must carry the T-tube for several weeks before its removal. Primary closure of the CBD without drainage has been proposed as a safe alternative to T-tube placement after laparoscopic choledochotomy. This randomized study aimed to compare the postoperative course and final outcome between the two methods applied after LCBDE.
Methods
Between January 2000 and January 2004, 80 patients treated with laparoscopic choledochotomy for CBD stones were randomly assigned to primary duct closure (n = 40) or T-tube drainage (n = 40). The primary end points were morbidity, operative time, postoperative stay, hospital expenses, and time until return to work.
Results
There were no differences in the demographic characteristics or clinical presentations between the two groups. In the primary closure group, the postoperative stay (5.2 ± 2.2 vs 8.3 ± 3.6 days) and the time until return to work (12.6 ± 5.1 vs 20.4 ± 13.2 days) were significantly shorter, the hospital expenses (8,638 ± 2,946 vs 12,531 ± 4,352 yuan) were significantly lower, and the incidences of postoperative complications (15% vs 27.5%) and biliary complications (10% vs 20%) were statistically and insignificantly lower than in the T-tube drainage group. In the primary closure group, six patients experienced postoperative complications, four of whom had biliary complications, compared, respectively, with 11 and 8 patients in the T-tube drainage group.
Conclusions
This study showed that primary CBC closure after laparoscopic choledochotomy was a viable alternative to mandatory T-tube drainage.
Similar content being viewed by others
Laparoscopic common bile duct exploration (LCBDE) for choledocholithiasis is feasible and has become increasingly popular with the development of instruments and the perfection of operative skills [1–7]. The LCBDE procedure can be performed transcystically or by choledochotomy. A successful transcystic extraction of common bile duct (CBD) stones usually makes external biliary drainage unnecessary, and this approach is preferred whenever feasible.
The transcystic approach, however, may be limited by stones too great in number or size and a cystic duct too small in diameter or implanted too low. In such cases, laparoscopic choledochotomy is an alternative solution [4–7], but it may carry higher morbidity rates, prolong recovery, and increase hospital expenses due to T-tube insertion [1, 7–9].
The disadvantage associated with the use of the T-tube led several authors to perform laparoscopic primary duct closure after choledochotomy. They found it safe to perform such closure after laparoscopic choledochotomy [6, 9, 10]. To date, however, no large, prospective, randomized trials have compared primary closure and T-tube drainage of the CBD after laparoscopic choledochotomy. Hence, we conducted a randomized study to compare the postoperative course and final outcome of primary closure and T-tube drainage of the CBD after laparoscopic choledochotomy.
Methods
Patients
Between January 2000 and January 2004, a total of 204 patients with CBD stones underwent LCBDE, with successful completion of 193 cases and the remaining 11 cases requiring conversion to open surgery because of LCBDE failure. Of the 193 successfully treated patients, 100 underwent laparoscopic transcystic stone extraction and 93 required laparoscopic choledochotomy.
The selection criteria for laparoscopic choledochotomy specified multiple large, or proximal ductal stones, failure of transcystic duct exploration, and a CBD diameter of 8 mm or greater. The diagnosis of CBD stones was based on clinical features, blood biochemical data, transabdominal ultrasonography, and cholangiography. Intraoperative cholangiography (IOC) was applied to all the patients. At preoperative assessment, the patients were classified according to the American Society of Anesthesiologists (ASA) classification.
The criteria for inclusion in the study specified a patient older than 12 years who had undergone a laparoscopic choledochotomy. The exclusion criteria specified a patient 12 years of age or younger who had acute suppurative cholangitis, severe acute biliary pancreatitis, ampullary stenosis, and a previous gastrectomy or failure of endoscopic retrograde cholangiopancreatography (ERCP). Among the patients who had undergone laparoscopic choledochotomy 13 were ineligible (1 of them ≤ 12 years of age, 5 with acute suppurative cholangitis, 3 with acute biliary pancreatitis, 2 with ampullary stenosis, and 2 with failure of ERCP).
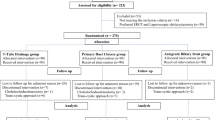
The 80 eligible patients were randomly assigned to two groups: primary closure group (n = 40) and T-tube drainage group (n = 40). Informed consent for randomization to primary closure or T-tube drainage was requested from all the patients involved. Randomization was performed with the use of a computer-generated randomization schedule with blocks of four randomly assigned numbers. In each block, two patients were assigned to the primary duct closure group and two patients were assigned to the T-tube drainage group (Fig. 1).
Operative techniques
All the operations were performed by two experienced laparoscopic surgeons, and they were of similar experience in both groups. All the patients underwent general anesthesia.
Laparoscopic cholecystectomy was performed by a standardized technique using a 30° video laparoscope placed through a 10-mm umbilical port and two additional laparoscopic sheaths: one at the subxiphoid site and one on the right subcostal line. Transcystic IOC was performed to assess biliary anatomy and stones or filling defects of the CBD. An IOC was performed typically by introducing a 14-gauge cholangiocatheter through a small puncture site in the right upper quadrant. The catheter then was inserted into a small incision in the cystic duct and secured in place with a clip. A half-strength contrast solution was injected under fluoroscopy for visualization of the biliary anatomy. Biliary anatomy as well as the number, size, and location of bile duct stones was considered in choosing a trancystic approach or a choledochotomy.
After demonstration of CBD stones, a fourth port (10 mm) was placed on the right subcostal line just above the gallbladder, through which a 5-mm flexible choledochoscope (Olympus, Tokyo, Japan) was inserted and connected to a second video system. The bile duct was dissected and exposed by pulling Hartmann’s pouch with an intact cystic duct to the right or by pulling the cystic duct stump. A longitudinal incision no longer than the largest stone was made in the anterior surface of the CBD and below the cystic duct, through which a choledochscope was inserted into the CBD at a right angle and maneuvered both proximally and distally in the biliary tree. A Dormia basket or irrigating balloon catheter was used to retrieve the stones. Biliary lithotripsy was used if necessary to fragment large stones or stones impacted at the ampulla.
After complete clearance of the CBD, the patients were randomly assigned to primary duct closure or T-tube drainage. In the primary closure group, the choledochotomy was closed primarily with a running absorbable suture (4–0 Vicryl), whereas in the T-tube drainage group, a latex rubber T-tube of appropriate size (14–20 Fr) was inserted into the CBD incision. After the tube had been positioned in place, the CBD incision was closed using interrupted sutures (4-0 Vicryl). Saline was flushed through the T-tube or the transcystic cholangiography catheter to rule out leakage. At the end of the procedure, a peritoneal drain was placed in the subhepatic space.
Discharge and follow-up evaluation
Patients resumed diet gradually. The peritoneal drain was removed on postoperative day 2 or 3, giving no evidence of bile leakage. Patients with T-tube drainage had the T-tube clamped on day 5. A postoperative cholangiograhy was performed 7 days after the operation, and the patients were discharged with the clamped T-tube if the cholangiogram was normal. The T-tube then was removed 3 to 4 weeks after the operation in the outpatient clinic. If there were retained stones, the T-tube was left in place for another 3 to 4 weeks. Patients with primary closure were discharged once the peritoneal drain was removed. All patients received regular follow-up assessments every 3 to 6 months in the specialty clinic.
Statistical analysis
Categorical variables were presented as count and percentage, and the statistical difference between the two groups was determined by chi-square testing. Continuous variables were expressed as mean ± standard derivation (SD) or as median and interquartile range (IQR), and comparisons of data were performed with Student’s t-test or the Mann–Whitney test. Statistical significance was determined by a p value less than 0.05.
Results
There were no statistically significant differences in the demographic characteristics (Table 1) and clinical presentations of CBD stones (Table 2) between the two groups. All the patients underwent choledochotomy except the six who failed in the transcystic extraction of stones. The bile duct exploration findings were negative for three patients (1 from the primary closure group and 2 from the T-tube drainage group) due to false-positive cholangiography results. Two patients had retained stones after laparoscopic clearance of the bile duct. One patient in the primary closure group underwent an endoscopic retrograde cholangiography for recurrent pain and jaundice, and the retained stone was removed by endoscopic sphincterotomy (EST). Another patient in the T-tube drainage group underwent postoperative cholangiograhy. Her retained stones were removed through the sinus tract of the T-tube using the choledochoscope.
As shown in Table 3, the median postoperative hospital stay was shorter in the primary closure group (5.2 ± 2.2 days) than in T-tube group (8.3 ± 3.6 days; p = 0.006). The median time until return to work and full physical activity also was shorter in the primary closure group (12.6 ± 5.1 days) than in the T-tube group (20.4 ± 13.2 days; p = 0.005). The median hospital expenses were lower in the primary closure group (8,638 ± 2,946 RMB yuan) than in the T-tube group (12,531 ± 4,352 RMB yuan; p = 0.028). The median operative time was statistically and insignificantly shorter in the primary closure group than in the T-tube group, but there was no difference in the median time until removal of the peritoneal drain between the two groups.
There was no postoperative death in either group. In the primary closure group, six patients experienced postoperative complications (15%), and four of them (10%) had biliary complications. Two patients experienced minor bile leakage, which stopped spontaneously with extended peritoneal drainage. One patient experienced bile leakage and ampullary edema-induced acute biliary pancreatitis on day 3 after the operation, which was treated by ERCP and stent insertion. One subhepatic bile accumulation occurred after removal of the peritoneal drain, which was removed successfully by a percutaneous drainage performed under ultrasonic guidance. Other complications included one wound infection at the trocar site of gallbladder extraction and a case of pneumonia.
In the T-tube drainage group, 11 patients (27.5%) experienced postoperative complications, 8 (20%) of whom had biliary complications. Seven patients had complications resulting from T-tube drainage. The incidences of total postoperative complications and biliary complications were statistically and insignificantly lower in the primary closure group than in the T-tube group (Table 3).
Leakage around the T-tube drainage was found in two patients, but it stopped spontaneously with extended peritoneal and T-tube drainage. One patient required percutaneous drain insertions for subhepatic bile accumulation. Transient acute pancreatitis developed in one patient, and responded to conservative treatment. Two patients were treated with T-tube replacement by repeated laparotomy. The one experienced worsening jaundice due to a twisted T-tube and subsequent bile duct obstruction, whereas biliary peritonitis developed in the other patient after the T-tube was mistakenly removed 5 days after the operation.
After T-tube removal, two patients had significant bile leakage, with one experiencing local biliary peritonitis and bile accumulation. This patient was treated using analgesia and antibiotics, with the drain tube reinserted through the T-tube sinus tract. Extensive biliary peritonitis developed in another patient, requiring open drainage (Table 4). Other complications included one case of wound cellulites around the T-tube and one case of deep venous thrombosis. In both groups, one patient was missing during the follow-up evaluation. The total follow-up rate was 97.5%, and the follow-up period was 6 to 54 months (average, 25 months). There was no occurrence of bile duct stones or bile duct stricture in either group.
Discussion
A T-tube is routinely inserted for biliary drainage after open or laparoscopic choledochotomy. Historically, postoperative T-tube drainage has been used to prevent bile stasis, decompress the biliary tree, and minimize the risk of bile leakage [11]. A T-tube also has provided an easy percutaneous access for cholangiography and extraction of retained stones [12].
Despite these advantages, a specific morbidity related to T-tube usage is reported to occur at a rate of 0% to 6.3% in series of open choledochotomy [13–15] and at a rate of 4% to 16.4% in laparoscopic series [3, 6, 16]. Accidental T-tube displacement leading to CBD obstruction [8, 17], bile leakage around the T-tube [17, 18], duodenal erosion [19], persistent biliary fistula [2, 17], wound cellulites around the T-tube [2], excoriation of the skin, and cholangitis caused by microorganisms entering through the T-tube [15] may retard recovery, prolong the hospital stay, and negate the benefits of laparoscopic surgery. Indwelling T-tubes are uncomfortable, require continuous management, and restrict the patient’s activity because of the risk for dislodgement [20]. Patients with an open T-tube are at risk for dehydration and saline depletion [21], and CBD stenosis has been reported as a long-term postoperative complication after T-tube removal [17].
Halsted [22] first described the use of primary closure after open CBD exploration in 1917. Thereafter, many authors reported that primary closure after open choledochotomy was feasible and safe [23–25]. A randomized trial by Williams et al. [25] found that primary closure after open choledochotomy significantly reduced the hospital stay without increasing the morbidity or mortality rate. Several retrospective studies have shown that primary duct closure after laparoscopic choledochotomy may be safe [6, 10]. Nevertheless, to date, no large prospective randomized trials have compared primary closure and T-tube drainage of the CBD after laparoscopic choledochotomy.
Our results support the aforementioned conclusion. In the current study, no postoperative mortality was found in either group. The postoperative hospital stay and the time until return to work were shorter and the hospital expenses lower in the primary closure group than in the T-tube group. The rates of total postoperative complication and biliary complication were statistically and insignificantly lower in the primary closure group than in the T-tube group. Most complications in the T-tube group were related to the use of the T-tube. In support of our findings, a recent retrospective study also showed that the rate of postoperative complications was higher in the T-tube group than in the primary closure group (15% vs 8%) [9].
In the current study, we also found that the use of the T-tube directly related to an increased risk of biliary peritonitis and bile leakage. Bile leakage and biliary peritonitis were likely to occur when the T-tube was removed, and they may be associated with insufficient accretions in abdominal cavity because accretions were important for the formation of the T-tube sinus tract.
Our findings also showed that primary closure did not increase the risk of bile leakage after the operation. Therefore, postoperative T-tube drainage is unnecessary for decompression of the biliary tree. Decker et al. [10] reported 100 cases of primary duct closures, with only three cases of bile leakage after laparoscopic choledochotomy. In addition, the use of intraoperative choledochoscopy and cholangiography can to a great extent avoid overlooked biliary problems.
Several retrospective studies [9, 10] have showed the stone clearance rate to be 100% with respect to positive explorations by laparoscopic choledochotomy. In the current study, 2 (2.5%) of 80 patients had retained stones. Therefore, use the T-tube to provide easy percutaneous access for cholangiography and extraction of retained stones after laparoscopic choledochotomy is seldom necessary. Even if stones are retained in patients who have undergone primary closure, most stones can be removed by EST, with no additional surgery required.
Nevertheless, primary duct closure is not suitable for all patients undergoing laparoscopic choledochotomy. The use of primary duct closure is limited in the treatment of patients with severe acute biliary pancreatic, acute pyogenic cholangitis, or ampullary stenosis because they require CBD decompression and drainage as well as other preferable therapeutic options. We did not use primary closure for patients with a history of gastrectomy who failed ERCP because an endoscopic access and treatment were not possible for them in the case of bile leakage and retained stones. A CBD diameter that is too small ( < 8 mm) might be a contraindication to a laparoscopic choledochotomy because such a CBD might increase the risk of bile duct stricture [6].
We agree with Decker et al. [10] that hospital stay is not a major criterion for assessing the outcome of surgery because discharge policies differ among institutions. In the current study, patients with primary closure were discharged on day 3 or 4 once the peritoneal drain was removed, but we kept the patients with the T-tube in the hospital until after the T-tube cholangiogram on day 7.
The length of hospital stay was influenced by many factors. It was not dictated only by the clinical outcome of individual patients but reflected socioeconomic aspects of patients and medical institutions. The patients could not go home with a functioning T-tube until a T-tube cholangiogram had been performed. We believe that the risks of dehydration and saline depletion in patients with open T-tubes at home are contraindications to this technique. Furthermore, it is unacceptable to the majority of our patients to go home with a functioning T-tube. Because the hospitalization expense at our hospital is quite cheap, 25 to 40 yuan per day, prolonging the hospital stay would not significantly influence the total hospital expense. This study proceeded with our belief that hospital expenses are a good criterion for assessing the outcome of surgery. The higher expense in the T-tube group had something to do with the treatment, for its increased complications and transfusion.
This randomized study was aimed only at comparing the safety and feasibility of two methods used after laparoscopic choledochotomy. The size of the study was based on some retrospective clinical information we possessed. In theory, the postoperative biliary complications should be considered as a primary outcome variable for calculating the size of samples. According to the literature, the occurrence ratio of biliary complications is 8% for primary closure and 15% for T-tube drainage. This calculation is based on a sample size of 446 patients for each group according to the formula for comparing two means (α = 0.05, β = 0.1) [26]. A study with such a large sample size cannot be conducted with our hospital alone. A clinical random study with a large sample should be carried out by several centers.
In conclusion, this large, prospective, randomized trial study is the first to compare the safety and feasibility of primary duct closure and T-tube drainage after laparoscopic choledochotomy. The results confirm the safety and feasibility of primary duct closure after laparoscopic choledochotomy. In effect, primary closure avoids the disadvantages associated with the use of the T-tube. Therefore, we recommend performing primary duct closure in suitable patients after laparoscopic choledochotomy.
References
Franklin ME Jr, Pharand D, Rosenthal D (1994) Laparoscopic common bile duct exploration. Surg Laparosc Endosc 4:119–124
Rhodes M, Nathanson L, O’Rourke N, Fielding G (1995) Laparoscopic exploration of the common bile duct: lessons learned from 129 consecutive cases. Br J Surg 82:666–668
Rhodes M, Sussman L, Cohen L, Lewis MP (1998) Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet 351:159–161
Millat B, Atger J, Deleuze A, Briandet H, Fingerhut A, Guillon F, Marrel E, De Seguin C, Soulier P (1997) Laparoscopic treatment for choledocholithiasis: a prospective evaluation in 247 consecutive unselected patients. Hepatogastroenterology 44:28–34
Tokumura H, Umezawa A, Cao H, Sakamoto N, Imaoka Y, Ouchi A, Yamamoto K (2002) Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg 9:206–212
Martin IJ, Bailey IS, Rhodes M, O'Rourke N, Nathanson L, Fielding G (1998) Towards T-tube-free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg 228:29–34
Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, Faggioni A, Ribeiro VM, Jakimowicz J, Visa J, Hanna GB (1999) EAES multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc 13:952–957
Bernstein DE, Goldberg RI, Unger SW (1994) Common bile duct obstruction following T-tube placement at laparoscopic cholecystectomy. Gastrointest Endosc 40:362–365
Ha JP, Tang CN, Siu WT, Chau CH, Li MK (2004) Primary closure versus T-tube drainage after laparoscopic choledochotomy for common bile duct stones. Hepatogastroenterology 51:1605–1608
Decker G, Borie F, Millat B, Berthou JC, Deleuze A, Drouard F, Guillon F, Rodier JG, Fingerhut A (2003) One hundred laparoscopic choledochotomies with primary closure of the common bile duct. Surg Endosc 17:12–18
De Roover D, Vanderveken M, Gerard Y (1989) Choledochotomy: primary closure versus T-tube: a prospective trial. Acta Chir Belg 89:320–324
Paganini AM, Feliciotti F, Guerrieri M, Tamburini A, De Sanctis A, Campagnacci R, Lezoche E (2001) Laparoscopic common bile duct exploration. J Laparoendosc Adv Surg Tech A 11:391–400
Moreaux J (1995) Traditional surgical management of common bile duct stones: a prospective study during a 20-year experience. Am J Surg 169:220–226
Pappas TN, Slimane Brooks DC. Brooks DC (1990) 100 consecutive common duct explorations without mortality. Ann Surg 211: 260–262
Sheridan WG, Williams HO, Lewis MH (1987) Morbidity and mortality of common bile duct exploration. Br J Surg 74:1095–1099
Cuschieri A, Croce E, Faggioni A, Jakimowicz J, Lacy A, Lezoche E, Morino M, Ribeiro VM, Toouli J, Visa J, Wayand W (1996) EAES ductal stone study. Preliminary findings of multi-center prospective randomized trial comparing two-stage vs single-stage management. Surg Endosc 10:1130–1135
Qi Wei, Hong-Jie Hhu, Xiao-Yan Cai, Wei Q, Hu HJ, Cai XY, Li LB, Wang GY (2004) Biliary drainage after laparoscopic choledochotomy. World J Gastroenterol 10:3175–3178
Kacker LK, Mittal BR, Sikora SS, Ali W, Kapoor VK, Saxena R, Das BK, Kaushik SP (1995) Bile leak after T-tube removal: a scintigraphic study. Hepatogastroenterology 42:975–978
Mosimann F, Schneider R, Mir A, Gillet M (1994) Erosion of the duodenum by a biliary T-tube: an unusual complication of liver transplantation. Transplant Proc 26:3550–3551
Gersin KS, Fanelli RD (1998) Laparoscopic endobiliary stenting as an adjunct to common bile duct exploration. Surg Endosc 12:301–304
Wills VL, Gibson K, Karihaloot C, Jorgensen JO (2002) Complications of biliary T-tubes after choledochotomy. ANZ J Surg 72:177–180
Halsted WS (1924) Surgical papers. Vol. 2. Johns Hopkins University Press, Baltimore, MD pp 427–472
Vassilakis JS, Chattopadhyay DK, Irvin TT, Duthie HL (1979) Primary closure of the common bile duct after elective choledochotomy. J R Coll Surg Edinb 24:156–158
Sorensen VJ, Buck JR, Chung SK, Fath JJ, Horst HM, Obeid FN (1994) Primary common bile duct closure following exploration: an effective alternative to routine biliary drainage. Am Surg 60:451–454
Williams JA, Treacy PJ, Sidey P, Worthley CS, Townsend NC, Russell EA (1994) Primary duct closure versus T-tube drainage following exploration of the common bile duct. Aust N Z J Surg 64:823–826
Kirkwood BR (1988) Essentials of medical statistics. Blackwell Science, Malden, USA
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leida, Z., Ping, B., Shuguang, W. et al. A randomized comparison of primary closure and T-tube drainage of the common bile duct after laparoscopic choledochotomy. Surg Endosc 22, 1595–1600 (2008). https://doi.org/10.1007/s00464-007-9731-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9731-9