Abstract
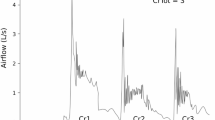
Progressive supranuclear palsy (PSP) is a neurodegenerative disease characterized by a high prevalence of dysphagia, cough dysfunction, and resultant aspiration pneumonia. Sensorimotor cough function is important for airway clearance in people with dysphagia. Upregulation of cough has been demonstrated in healthy adults and Parkinson’s disease; however, the feasibility of cough rehabilitation in PSP is unknown. We sought to assess feasibility by examining the immediate effects of a novel sensorimotor training in airway protection (smTAP) on upregulation of cough function in PSP. Fifteen individuals with PSP enrolled in this study. Baseline voluntary and reflex cough testing were completed. During smTAP, participants were presented with subthreshold capsaicin and instructed to cough with sufficient intensity to hit a target line (set 25% above baseline reflex peak cough flow) via cough airflow visual biofeedback. Twenty-five repetitions were targeted within a single session. Wilcoxon signed-rank tests compared cough airflow measures between baseline voluntary cough testing, the initial five trials of smTAP, and final five trials. Mean peak expiratory flow rate (PEFR) significantly increased from initial to final smTAP trials (p < 0.001). Fourteen participants increased PEFR, with gains of more than 10% in 11 participants. Variability of PEFR (p = 0.01) and cough expired volume (p = 0.01) significantly decreased across smTAP trials. This study is the first to demonstrate the ability of people with PSP to immediately upregulate cough function, providing preliminary support for the feasibility of cough rehabilitation in this population with this novel treatment approach. Future research examining the effects of multiple sessions of smTAP on cough outcomes is warranted.



Similar content being viewed by others
References
Dickson DW, Ahmed Z, Algom AA, Tsuboi Y, Josephs KA. Neuropathology of variants of progressive supranuclear palsy. Curr Opin Neurol. 2010;23(4):394–400.
Giagkou N, Höglinger GU, Stamelou M. Progressive supranuclear palsy. In: International review of neurobiology. Amsterdam: Elsevier; 2019. p. 49–86.
dell’Aquila C, Zoccolella S, Cardinali V, de Mari M, Iliceto G, Tartaglione B, et al. Predictors of survival in a series of clinically diagnosed progressive supranuclear palsy patients. Parkinsonism Relat Disord. 2013;19(11):980–5.
Mehanna R, Jankovic J. Respiratory problems in neurologic movement disorders. Parkinsonism Relat Disord. 2010;16(10):628–38.
Warnecke T, Oelenberg S, Teismann I, Hamacher C, Lohmann H, Ringelstein EB, et al. Endoscopic characteristics and levodopa responsiveness of swallowing function in progressive supranuclear palsy. Mov Disord. 2010;25(9):1239–45.
Johnston BT, Castell JA, Stumacher S, Colcher A, Gideon RM, Li Q, et al. Comparison of swallowing function in Parkinson’s disease and progressive supranuclear palsy. Mov Disord. 1997;12(3):322–7.
Clark HM, Stierwalt JAG, Tosakulwong N, Botha H, Ali F, Whitwell JL, et al. Dysphagia in progressive supranuclear palsy. Dysphagia. 2019;35(4):667–76.
Goetz CG, Leurgans S, Lang AE, Litvan I. Progression of gait, speech and swallowing deficits in progressive supranuclear palsy. Neurology. 2003;60(6):917–22.
Litvan I, Sastry N, Sonies BC. Characterizing swallowing abnormalities in progressive supranuclear palsy. Neurology. 1997;48(6):1654–62.
Matsuo K, Palmer JB. Coordination of mastication, swallowing and breathing. Jpn Dent Sci Rev. 2009;45(1):31–40.
Leopold NA, Kagel MC. Dysphagia in progressive supranuclear palsy: radiologic features. Dysphagia. 1997;12(3):140–3.
Glasmacher SA, Leigh PN, Saha RA. Predictors of survival in progressive supranuclear palsy and multiple system atrophy: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2017;88(5):402–11.
Litvan I, Mangone CA, McKee A, Verny M, Parsa A, Jellinger K, et al. Natural history of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome) and clinical predictors of survival: a clinicopathological study. J Neurol Neurosurg Psychiatry. 1996;60(6):615–20.
Mazzone SB, Farrell MJ. Heterogeneity of cough neurobiology: clinical implications. Pulm Pharmacol Ther. 2019;55:62–6.
Eccles R. Central mechanisms IV: conscious control of cough and the placebo effect. In: Chung KF, Widdicombe J, editors. Pharmacology and therapeutics of cough. Berlin: Springer; 2009. p. 241–62. https://doi.org/10.1007/978-3-540-79842-2_12.
Hegland KW, Bolser DC, Davenport PW. Volitional control of reflex cough. J Appl Physiol (1985). 2012;113(1):39–46.
Brandimore AE, Hegland KW, Okun MS, Davenport PW, Troche MS. Voluntary upregulation of reflex cough is possible in healthy older adults and Parkinson’s disease. J Appl Physiol (1985). 2017;123(1):19–26.
Davenport PW. Clinical cough I: the urge-to-cough: a respiratory sensation. In: Chung KF, Widdicombe J, editors. Pharmacology and therapeutics of cough [Internet]. Berlin, Heidelberg: Springer; 2009 [cited 2020 Jan 22]. p. 263–76. (Handbook of experimental pharmacology). Available from: https://doi.org/10.1007/978-3-540-79842-2_13.
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland KW. Decreased cough sensitivity and aspiration in Parkinson disease. Chest. 2014;146(5):1294–9.
Troche MS, Schumann B, Brandimore AE, Okun MS, Hegland KW. Reflex cough and disease duration as predictors of swallowing dysfunction in Parkinson’s disease. Dysphagia. 2016;31(6):757–64.
Kolb B, Cioe J. Neuronal organization and change after neuronal injury. In: Ponsford J, editor. Cognitive and behavioral rehabilitation. From neurobiology to clinical practice. New York: The Guilford Press; 2004.
Elbert T, Rockstroh B. Reorganization of human cerebral cortex: the range of changes following use and injury. Neuroscientist. 2004;10(2):129–41.
Höglinger GU, Respondek G, Stamelou M, Kurz C, Josephs KA, Lang AE, et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria: MDS Clinical Diagnostic Criteria for PSP. Mov Disord. 2017;32(6):853–64.
Dicpinigaitis PV. Short- and long-term reproducibility of capsaicin cough challenge testingq. Pulm Pharmacol. 2003;16(1):61–5.
Mancopes R, Smaoui S, Steele CM. Effects of expiratory muscle strength training on videofluoroscopic measures of swallowing: a systematic review. Am J Speech Lang Pathol. 2020;29(1):335–56.
Chung KF, Widdicombe J, Belvisi MG. Pharmacology and therapeutics of cough. In: Handbook of experimental pharmacology. Berlin: Springer; 2009. 375 p.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates; 1988. p. 567.
Plowman EK, Watts SA, Robison R, Tabor L, Dion C, Gaziano J, et al. Voluntary cough airflow differentiates safe versus unsafe swallowing in amyotrophic lateral sclerosis. Dysphagia. 2016;31(3):383–90.
Pitts T, Troche M, Mann G, Rosenbek J, Okun MS, Sapienza C. Using voluntary cough to detect penetration and aspiration during oropharyngeal swallowing in patients with parkinson disease. Chest. 2010;138(6):1426–31.
Silverman EP, Carnaby G, Singletary F, Hoffman-Ruddy B, Yeager J, Sapienza C. Measurement of voluntary cough production and airway protection in Parkinson disease. Arch Phys Med Rehabil. 2016;97(3):413–20.
Ebihara S, Saito H, Kanda A, Nakajoh M, Takahashi H, Arai H, et al. Impaired efficacy of cough in patients with Parkinson disease. Chest. 2003;124(3):1009–15.
Bianchi C, Baiardi P, Khirani S, Cantarella G. Cough peak flow as a predictor of pulmonary morbidity in patients with dysphagia. Am J Phys Med Rehabil. 2012;91(9):783–8.
Lasserson D. Differences in motor activation of voluntary and reflex cough in humans. Thorax. 2006;61(8):699–705.
Brandimore AE, Troche MS, Huber JE, Hegland KW. Respiratory kinematic and airflow differences between reflex and voluntary cough in healthy young adults. Front Physiol. 2015;6:1–10.
Tabor-Gray L, Vasilopoulos T, Wheeler-Hegland K, Wymer J, Plowman EK. Reflexive airway sensorimotor responses in individuals with amyotrophic lateral sclerosis. Dysphagia. 2020. https://doi.org/10.1007/s00455-020-10171-6.
Setaka Y, Takao T, Kawamura K, Watanabe K, Yoshida R, Ohse H, et al. Reliability of voluntary cough assessments using respiratory flow waveform. J Phys Ther Sci. 2020;32(7):454–8.
Borders JC, Brandimore AE, Troche MS. Variability of voluntary cough airflow in healthy adults and Parkinson’s disease. Dysphagia. 2020. https://doi.org/10.1007/s00455-020-10190-3.
Sternad D. It’s not (only) the mean that matters: variability, noise and exploration in skill learning. Curr Opin Behav Sci. 2018;20:183–95.
Dhawale AK, Smith MA, Ölveczky BP. The role of variability in motor learning. Annu Rev Neurosci. 2017;40(1):479–98.
Curtis JA, Dakin AE, Troche MS. Respiratory-swallow coordination training and voluntary cough skill training: a single-subject treatment study in a person with Parkinson’s disease. J Speech Lang Hear Res. 2020;63(2):472–86.
Vovk A, Bolser DC, Hey JA, Danzig M, Vickroy T, Berry R, et al. Capsaicin exposure elicits complex airway defensive motor patterns in normal humans in a concentration-dependent manner. Pulm Pharmacol Ther. 2007;20(4):423–32.
Acknowledgements
Portions of this manuscript were presented at the Dysphagia Research Society Meeting, May 2020.
Funding
This work was funded by the Cure PSP Foundation (Grant # 644-2016-11 to Dr. Troche).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all participants prior to enrollment in this research study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Borders, J.C., Curtis, J.A., Sevitz, J.S. et al. Immediate Effects of Sensorimotor Training in Airway Protection (smTAP) on Cough Outcomes in Progressive Supranuclear Palsy: A Feasibility Study. Dysphagia 37, 74–83 (2022). https://doi.org/10.1007/s00455-021-10251-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10251-1