Abstract
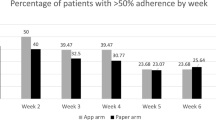
Dysphagia following treatment for head and neck cancer is one of the most significant morbidities impacting quality of life. Despite the value of prophylactic exercises to mitigate the impact of radiation on long-term swallowing function, adherence to treatment is limited. The purpose of this investigation was to explore the feasibility of a mobile health application to support patient adherence to swallowing therapy during radiation-based treatment. 36 patients undergoing radiation therapy were provided with the Vibrent™ mobile application as an adjunct to standard swallowing therapy. The application included exercise videos, written instructions, reminders, exercise logging, and educational content. 80% of participants used the app during treatment and logged an average of 102 exercise sessions over the course of treatment. 25% of participants logged at least two exercise sessions per day over the 7-week treatment period, and 53% recorded at least one session per day. Exit interviews regarding the patient experience with the Vibrent™ mobile application were largely positive, but also provided actionable strategies to improve future versions of the application. The Vibrent™ mobile application appears to be a tool that can be feasibly integrated into existing patient care practices and may assist patients in adhering to treatment recommendations and facilitate communication between patients and providers between encounters.



Similar content being viewed by others
References
Chaturvedi AK, Engels EA, Anderson WF, et al. Incidence trends for human papilloma virus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612–9.
King SN, Dunlap NE, Tennant PA, Pitts T. Pathophysiology of radiation-induced dysphagia in head and neck cancer. Dysphagia. 2016;31(3):339–51.
Starmer HM, Tippett D, Webster K, et al. Swallowing outcomes in patients with oropharyngeal cancer undergoing organ-preservation treatment. Head Neck. 2014;36(10):1392–7.
Lazarus C, Logeman J, Pauloski B, et al. Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy. Laryngoscope. 1996;106(9Pt1):1157–66.
Newman LA, Vieira F, Schwierzer V, et al. Eating and weight changes following chemoradiation therapy for advanced head and neck cancer. Arch Otolaryngol Head Neck Surg. 1998;124(5):589–92.
Hunter KU, Lee OE, Lyden TH, et al. Aspiration pneumonia after chemo-intensity-modulated radiation therapy of oropharyngeal carcinoma and its clinical and dysphagia-related predictors. Head Neck. 2014;36:120–5.
Carroll WR, Locher JL, Canon CL, et al. Pretreatment swallowing exercises improve swallow function after chemoradiation. Laryngoscope. 2008;118:39–43.
Kotz T, Federman AD, Kao J, et al. Prophylactic swallowing exercises in patients with head and neck cancer undergoing chemoradiation: a randomized trial. Arch Otolaryngol Head Neck Surg. 2012;138:376–82.
van der Molen L, van Rossum MA, Burkhead LM, et al. A randomized preventative rehabilitation trial in advanced head and neck cancer patients treated with chemoradiotherapy: feasibility, compliance, and short-term effects. Dysphagia. 2011;26:115–70.
Carnaby-Mann G, Crary MA, Schmalfus I, Amdur R. “Pharyngocise”: randomized control trial of preventative exercises to maintain muscle structure and swallowing function during head and neck chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012;83:210–9.
Langmore S, Krisciunas GP, Miloro KV, et al. Does PEG cause dysphagia in head and neck cancer patients? Dysphagia. 2012;27(2):251–9.
Hutcheson KA, Bhayani MK, Beadle BM, et al. Eat and exercise during radiotherapy or chemoradiotherapy for pharyngeal cancers. Use it or lose it. JAMA. Otolaryngol Head Neck Surg. 2013;139(11):1127–34.
Ward MC, Bjateja P, Nwizu T, et al. Impact of feeding tube choice on severe late dysphagia after definitive chemoradiotherapy for human papilloma virus-negative head and neck cancer. Head Neck. 2016;38(Suppl 1):E1054–60.
Shinn EH, Basen-Engquist K, Baum G, et al. Adherence to preventative exercises and self-reported swallowing outcomes in post-radiation head and neck cancer patients. Head Neck. 2013;35(12):1707–12.
Mortensen HR, Jensen K, Aksglaede K, et al. Prophylactic swallowing exercises in head and neck cancer radiotherapy. Dysphagia. 2015;30(3):304–14.
Cnossen IC, van Uden-Kraan CF, Witte BL, et al. Prophylactic exercises among head and neck cancer patients during and after swallowing sparing intensity modulated radiation: adherence and exercise performance levels of a 12-week guided home-based program. Eur Arch Otorhinolaryngol. 2017;274:1129–38.
Wall LR, Ward EC, Cartmill B, Hill AJ, Porceddu SV. Adherence to a prophylactic swallowing therapy program during (chemo) radiotherapy: impact of service delivery model and patient factors. Dysphagia. 2017;32(2):279–92.
Guarino H, Acosta M, Marsch LA, Xie H, Aponte-Melendez Y. A mixed-methods evaluation of the feasibility, acceptability, and preliminary efficacy of a mobile intervention for methadone maintenance clients. Psychol Addict Behav. 2016;30(1):1–11.
Hui CY, Walton R, McKinstry B, et al. The use of mobile applications to support self-management for people with asthma: a systematic review of controlled studies to identify features associated with clinical effectiveness and adherence. J Am Med Inform Assoc. 2016;24:619–32.
Litman L, Rosen Z, Spierer D, et al. Mobile exercise apps and increased leisure time exercise activity: a moderated mediation analysis of the role of self-efficacy and barriers. J Med Internet Res. 2015;17(8):e195.
Badaway SM, Barrera L, Sinno MG, Kaviany S, O’Dwyer LC, Kuhns LM. Text messaging and mobile phone apps as interventions to improve adherence in adolescents with chronic health conditions: a systematic review. JMIR mHealth uHealth. 2017;5(5):e66.
Lambert TE, Harvey LA, Avdalis C, Chen LW, Jeyalingam S, et al. An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: a randomized trial. J Physiother. 2017;63:161–7.
Anderson M. Technology device ownership. Pew research center. Washington, DC. 2015. http://www.pewinternet.org/2015/10/29/technology-device-ownership-2015/. Accessed 8 oct 2017.
DiFillippo KN, Huang WH, Andrade JE, Chapman-Novakofski KM. The use of mobile apps to improve nutrition outcomes: a systematic literature review. J Telemed Telecare. 2015;21(5):243–53.
Rossi MCE, Nicolucci A, Pellegrini F, et al. Interactive diary for diabetes: a useful and easy-to-use new telemedicine system to support the decision making process in type 1 diabetes. Diabetes Tech Ther. 2009;11:19–24.
Kuijpers W, Groen WG, Aaronson NK, van Harten WH. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res. 2015;15(2):e37.
Govender R, Smith CH, Taylor SA, Barratt H, Gardner B. Swallowing interventions for the treatment of dysphagia after head and neck cancer: a systematic review of behavioural strategies used to promote patient adherence to swallowing exercises. BMC Cancer. 2017;17:43–58.
Dahlstrom KR, Bell D, Hanby D, et al. Socioeconomic characteristics of patients with oropharyngeal carcinoma according to tumor HPV status, patient smoking history, and sexual behavior. Oral Oncol. 2015;51(9):832–8.
Young D, Xiao CC, Murphy B, Moore M, Fakhry C, Day TA. Increase in head and neck cancer in younger patients due to human papillomavirus (HPV). Oral Oncol. 2015;51(8):727–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Starmer, H.M., Abrams, R., Webster, K. et al. Feasibility of a Mobile Application to Enhance Swallowing Therapy for Patients Undergoing Radiation-Based Treatment for Head and Neck Cancer. Dysphagia 33, 227–233 (2018). https://doi.org/10.1007/s00455-017-9850-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9850-y