Abstract
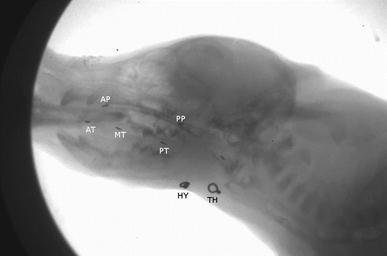
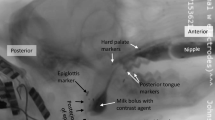
Recurrent laryngeal nerve (RLN) damage in infants leads to increased dysphagia and aspiration pneumonia. Recent work has shown that intraoral transport and swallow kinematics change following RLN lesion, suggesting potential changes in bolus formation prior to the swallow. In this study, we used geometric morphometrics to understand the effect of bolus shape on penetration and aspiration in infants with and without RLN lesion. We hypothesized (1) that geometric bolus properties are related to airway protection outcomes and (2) that in infants with RLN lesion, the relationship between geometric bolus properties and dysphagia is changed. In five infant pigs, dysphagia in 188 swallows was assessed using the Infant Mammalian Penetration–Aspiration Scale (IMPAS). Using images from high-speed VFSS, bolus shape, bolus area, and tongue outline were quantified digitally. Bolus shape was analyzed using elliptical Fourier analysis, and tongue outline using polynomial curve fitting. Despite large inter-individual differences, significant within individual effects of bolus shape and bolus area on airway protection exist. The relationship between penetration–aspiration score and both bolus area and shape changed post lesion. Tongue shape differed between pre- and post-lesion swallows, and between swallows with different IMPAS scores. Bolus shape and area affect airway protection outcomes. RLN lesion changes that relationship, indicating that proper bolus formation and control by the tongue require intact laryngeal sensation. The impact of RLN lesion on dysphagia is pervasive.






Similar content being viewed by others
References
Benjamin JR, Smith PB, Cotten CM, Jaggers J, Goldstein RF, Malcolm WF. Long-term morbidities associated with vocal cord paralysis after surgical closure of a patent ductus arteriosus in extremely low birth weight infants. J Perinatol. 2010;30:408–13.
Pereira KR, Firpo C, Gasparin M, Teixeira AR, Dornelles S, Bacaltchuk T, et al. Evaluation of swallowing in infants with congenital heart defect. Int Arch Otorhinolaryngol. 2015;19:055–60.
Daya H, Hosni A, Bejar-Solar I, Evans JNG, Bailey CM. Pediatric vocal fold paralysis: a long-term retrospective study. Arch Otolaryngol Head Neck Surg. 2000;126:21.
Périé S, Laccourreye O, Bou-Malhab F, Brasnu D. Aspiration in unilateral recurrent laryngeal nerve paralysis after surgery. Am J Otolaryngol. 1998;19:18–23.
de Gaudemar I, Roudaire M, François M, Narcy P. Outcome of laryngeal paralysis in neonates: a long term retrospective study of 113 cases. Int J Pediatr Otorhinolaryngol. 1996;34:101–10.
Nichols BG, Jabbour J, Hehir DA, Ghanayem NS, Beste D, Martin T, et al. Recovery of vocal fold immobility following isolated patent ductus arteriosus ligation. Int J Pediatr Otorhinolaryngol. 2014;78:1316–9.
Gould FDH, Ohlemacher J, Lammers AR, Gross A, Ballester A, Fraley L, et al. Central nervous system integration of sensorimotor signals in oral and pharyngeal structures: oropharyngeal kinematics response to recurrent laryngeal nerve lesion. J Appl Physiol. 2016;120:495–502.
Holman SD, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Lukasik SL, Waranch DR, et al. Swallowing kinematics and airway protection after palatal local anesthesia in infant pigs: swallowing after palatal anesthesia. Laryngoscope. 2014;124:436–45.
German RZ, Crompton AW, Owerkowicz T, Thexton AJ. Volume and rate of milk delivery as determinants of swallowing in an infant model animal (Sus scrofa). Dysphagia. 2004;19:147–54.
Bookstein FL. A brief history of the morphometric synthesis. In: Marcus LF, editor. Advances in morphometrics. Cambridge: University Press; 1993.
German RZ, Crompton AW, Hertweck DW, Thexton AJ. Determinants of rhythm and rate in suckling. J Exp Zool. 1997;278:1–8.
Gould FDH, Lammers AR, Ohlemacher J, Ballester A, Fraley L, Gross A, et al. The physiologic impact of unilateral recurrent laryngeal nerve (RLN) lesion on infant oropharyngeal and esophageal performance. Dysphagia. 2015;30:714–22.
German RZ, Crompton AW, Thexton AJ. The role of animal models in understanding feeding behavior in infants. Int J Orofacial Myology. 2004;30:20–30.
Thexton AJ, Crompton AW, German RZ. Transition from suckling to drinking at weaning: a kinematic and electromyographic study in miniature pigs. J Exp Zool. 1998;280:327–43.
German RZ, Crompton AW, Levitch LC, Thexton AJ. The mechanism of suckling in two species of infant mammal: miniature pigs and long-tailed macaques. J Exp Zool. 1992;261:322–30.
Holman SD, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Griffioen AM, Inokuchi H, et al. Development, reliability, and validation of an infant mammalian penetration–aspiration scale. Dysphagia. 2013;28:178–87.
Rasband WS. ImageJ. Bethesda: NIH; 1997. http://imagej.nih.gov/ij/.
Okada T, Aoyagi Y, Inamoto Y, Saitoh E, Kagaya H, Shibata S, et al. Dynamic change in hyoid muscle length associated with trajectory of hyoid bone during swallowing: analysis using 320-row area detector computed tomography. J Appl Physiol. 2013;115:1138–45.
Kuhl FP, Giardina CR. Elliptic Fourier features of a closed contour. Comput Gr Image Process. 1982;18:236–58.
Iwata H. SHAPE: a computer program package for quantitative evaluation of biological shapes based on elliptic Fourier descriptors. J Hered. 2002;93:384–5.
Bonhomme V, Picq S, Gaucherel C, Claude J. Momocs: outline analysis using R. J Stat Softw. 2014;56:1–24.
Ferson S, Rohlf FJ, Koehn RK. Measuring shape variation of two-dimensional outlines. Syst Biol. 1985;34:59–68.
Zelditch ML, Swiderski DL, Sheets HD. Geometric morphometrics for biologists: a primer. Cambridge: Academic Press; 2012.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015.
Ding P, Fung GSK, Lin M, Holman SD, German RZ. The effect of bilateral superior laryngeal nerve lesion on swallowing: a novel method to quantitate aspirated volume and pharyngeal threshold in videofluoroscopy. Dysphagia. 2014;30:47–56.
Ding P, Campbell-Malone R, Holman SD, Lukasik SL, Thexton AJ, German RZ. The effect of unilateral superior laryngeal nerve lesion on swallowing threshold volume. Laryngoscope. 2013;123:1942–7.
Belo LR, Gomes NAC, Coriolano MGWS, de Souza ES, Moura DAA, Asano AG, et al. The relationship between limit of dysphagia and average volume per swallow in patients with Parkinson’s disease. Dysphagia. 2014;29:419–24.
Zargaraan A, Rastmanesh R, Fadavi G, Zayeri F, Mohammadifar MA. Rheological aspects of dysphagia-oriented food products: a mini review. Food Sci Hum Wellness. 2013;2:173–8.
Thexton A, Crompton A, Owerkowicz T, German R. Correlation between intraoral pressures and tongue movements in the suckling pig. Arch Oral Biol. 2004;49:567–75.
Inamoto Y, Saitoh E, Okada S, Kagaya H, Shibata S, Ota K, et al. The effect of bolus viscosity on laryngeal closure in swallowing: kinematic analysis using 320-row area detector CT. Dysphagia. 2013;28:33–42.
Ding P, Campbell-Malone R, Holman SD, Lukasik SL, Fukuhara T, Gierbolini-Norat EM, et al. Unilateral superior laryngeal nerve lesion in an animal model of dysphagia and its effect on sucking and swallowing. Dysphagia. 2013;28:404–12.
Holman SD, Waranch DR, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Lukasik SL, et al. Sucking and swallowing rates after palatal anesthesia: an electromyographic study in infant pigs. J Neurophysiol. 2013;110:387–96.
Michou E, Hamdy S. Cortical input in control of swallowing. Curr Opin Otolaryngol Head Neck Surg. 2009;17:166–71.
Leopold NA, Daniels SK. Supranuclear control of swallowing. Dysphagia. 2010;25:250–7.
Herring SW. Ontogeny of bone strain: the zygomatic arch in pigs. J Exp Biol. 2005;208:4509–21.
German RZ, Crompton AW, McCluskey C, Thexton AJ. Coordination between respiration and deglutition in a preterm infant mammal, Sus scrofa. Arch Oral Biol. 1996;41:619–22.
De Groote I, Aiello LC. Letter to the editor: response to Deane and Kremer’s comment: 3D, or not to 3D. Am J Phys Anthropol. 2011;144:498–9.
Brainerd EL, Baier DB, Gatesy SM, Hedrick TL, Metzger KA, Gilbert SL, et al. X-ray reconstruction of moving morphology (XROMM): precision, accuracy and applications in comparative biomechanics research. J Exp Zoo Part A Ecol Genet Physiol. 2010;313A:262–79.
Acknowledgements
The authors would like to thank the staff and the NEOMED comparative medicine unit, as well as Jackie Kulish, Katie DeLozier, and Tim Ohlemacher for their assistance in data collection.
Funding
This work was funded by NIH Grant R01 009980 to Rebecca German.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
None of the authors have any conflicts of interests to report.
Rights and permissions
About this article
Cite this article
Gould, F.D.H., Yglesias, B., Ohlemacher, J. et al. Pre-pharyngeal Swallow Effects of Recurrent Laryngeal Nerve Lesion on Bolus Shape and Airway Protection in an Infant Pig Model. Dysphagia 32, 362–373 (2017). https://doi.org/10.1007/s00455-016-9762-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9762-2