Abstract
Purpose
High-grade salivary gland carcinoma (SGC) shows a high rate of metastasis and post-treatment recurrence, resulting in poor patient survival. Therefore, we evaluated the utility of pre-treatment 18F-FDG PET/CT parameters in predicting metastasis, tumor progression, and survival of high-grade SGC patients.
Methods
This observational study included 75 patients with previously untreated high-grade SGC who underwent pre-treatment 18F-FDG PET/CT scanning and subsequent treatment. Standardized uptake values (SUV), metabolic tumor volume (MTV), and total lesion glycolysis (TLG) were measured on pre-treatment 18F-FDG PET/CT. Logistic regression analysis was used to identify the relationship of these factors with metastasis. Cox proportional hazard regression analyses were used to identify associations between PET parameters and both progression-free survival (PFS) and overall survival (OS).
Results
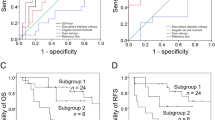
A total of 36 (48%) patients had neck or distant metastases at initial staging. After controlling for clinical factors, MTV (> 8.8 mL) was an independent factor for initial metastasis (adjusted odds ratio 4.80, 95% confidence interval 1.09–21.20; P = 0.039). All PET parameters of SUVmax (> 4.3), SUVmean (> 3.0), SUVpeak (3.9), MTV (> 8.8 mL), and TLG (> 31.1 g) were significant variables for PFS (all P < 0.05), while MTV and TLG were significant factors for OS. After controlling for clinicopathological factors, MTV (adjusted hazard ratio 4.36, 95% confidence interval 1.69–11.26; P = 0.002) and TLG (3.41, 1.47–7.91; P = 0.004) were significantly associated with PFS, but not OS.
Conclusions
MTV is useful among quantitative PET measurements for predicting initial metastasis and PFS in patients with high-grade SGC.


Similar content being viewed by others
References
Abgral R, Keromnes N, Robin P, Le Roux PY, Bourhis D, Palard X, Rousset J, Valette G, Marianowski R, Salaun PY (2014) Prognostic value of volumetric parameters measured by 18F-FDG PET/CT in patients with head and neck squamous cell carcinoma. Eur J Nucl Med Mol Imaging 41(4):659–667
Adelstein DJ, Rodriguez CP (2011) What is new in the management of salivary gland cancers?. Curr Opin Oncol 23(3):249–253
Ali S, Palmer FL, Yu C, DiLorenzo M, Shah JP, Kattan MW, Patel SG, Ganly I (2014) Postoperative nomograms predictive of survival after surgical management of malignant tumors of the major salivary glands. Ann Surg Oncol 21(2):637–642
Boellaard R, O’Doherty MJ, Weber WA, Mottaghy FM, Lonsdale MN, Stroobants SG, Oyen WJ, Kotzerke J, Hoekstra OS, Pruim J, Marsden PK, Tatsch K, Hoekstra CJ, Visser EP, Arends B, Verzijlbergen FJ, Zijlstra JM, Comans EF, Lammertsma AA, Paans AM, Willemsen AT, Beyer T, Bockisch A, Schaefer-Prokop C, Delbeke D, Baum RP, Chiti A, Krause BJ (2010) FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging 37(1):181–200
Cho JK, Lim BW, Kim EH, Ko YH, Oh D, Noh JM, Ahn YC, Baek KH, Jeong HS (2016) Low-grade salivary gland cancers: treatment outcomes, extent of surgery and indications for postoperative adjuvant radiation therapy. Ann Surg Oncol 23(13):4368–4375
Chong A, Ha JM, Han YH, Kong E, Choi Y, Hong KH, Park JH, Kim SH, Park JM (2017) ‘Preoperative lymph node staging by FDG PET/CT with contrast enhancement for thyroid cancer: a multicenter study and comparison with neck CT’. Clin Exp Otorhinolaryngol 10(1):121–128
Denaro N, Merlano MC, Russi EG (2016) Follow-up in head and neck cancer: do more does it mean do better? A systematic review and our proposal based on our experience. Clin Exp Otorhinolaryngol 9(4):287–297
Edge SB, Compton BD, Fritz CC, Greene AG, Trotti FL A (2010) Major salivary gland. In: AJCC cancer staging manual, 7th edn. Springer, New York, pp 79–86
Ettl T, Gosau M, Brockhoff G, Schwarz-Furlan S, Agaimy A, Reichert TE, Rohrmeier C, Zenk J, Iro H (2014) Predictors of cervical lymph node metastasis in salivary gland cancer. Head Neck 36(4):517–523
Eveson JW, Auclair P, Gnepp DR, El-Naggar AK (2005) Tumours of the salivary glands. In: Leon B, Eveson JW, Reichart P, Sidransky D (eds) World health organization classification of tumours. Pathology & genetics—head and neck tumours. IARC Press, Lyon, pp 209–281
Ha SC, Oh JS, Roh JL, Moon H, Kim JS, Cho KJ, Choi SH, Nam SY, Kim SY (2017) ‘Pretreatment tumor SUVmax predicts disease-specific and overall survival in patients with head and neck soft tissue sarcoma’. Eur J Nucl Med Mol Imaging 44(1):33–40
Haderlein M, Scherl C, Semrau S, Lettmaier S, Uter W, Neukam FW, Iro H, Agaimy A, Fietkau R (2016) High-grade histology as predictor of early distant metastases and decreased disease-free survival in salivary gland cancer irrespective of tumor subtype. Head Neck, 38 Suppl 1:E2041–E2048
Hong HR, Roh JL, Cho KJ, Choi SH, Nam SY, Kim SY (2015) Prognostic value of lymph node density in high-grade salivary gland cancers. J Surg Oncol 111(6):784–789
Hosni A, Huang SH, Goldstein D, Xu W, Chan B, Hansen A, Weinreb I, Bratman SV, Cho J, Giuliani M, Hope A, Kim J, O’Sullivan B, Waldron J, Ringash J (2016) Outcomes and prognostic factors for major salivary gland carcinoma following postoperative radiotherapy. Oral Oncol 54:75–80
Hsieh CE, Ho KC, Hsieh CH, Yen TC, Liao CT, Wang HM, Lin CY (2017) Pretreatment primary tumor SUVmax on 18F-FDG PET/CT images predicts outcomes in patients with salivary gland carcinoma treated with definitive intensity-modulated radiation therapy. Clin Nucl Med 42(9):655–662
Ito T, Noguchi Y, Satoh S, Hayashi H, Inayama Y, Kitamura H (1998) Expression of facilitative glucose transporter isoforms in lung carcinomas: its relation to histologic type, differentiation grade, and tumor stage. Mod Pathol 11(5):437–443
Jeong HS, Chung MK, Son YI, Choi JY, Kim HJ, Ko YH, Baek CH (2007) Role of 18F-FDG PET/CT in management of high-grade salivary gland malignancies. J Nucl Med 48(8):1237–1244
Jung JH, Lee SW, Son SH, Kim CY, Lee CH, Jeong JH, Jeong SY, Ahn BC, Lee J (2017) Clinical impact of 18 F-FDG positron emission tomography/CT on adenoid cystic carcinoma of the head and neck. Head Neck 39(3):447–455
Kim MJ, Kim JS, Roh JL, Lee JH, Cho KJ, Choi SH, Nam SY, Kim SY (2013) ‘Utility of 18F-FDG PET/CT for detecting neck metastasis in patients with salivary gland carcinomas: preoperative planning for necessity and extent of neck dissection’. Ann Surg Oncol 20(3):899–905
Kim JW, Oh JS, Roh JL, Kim JS, Choi SH, Nam SY, Kim SY (2015) Prognostic significance of standardized uptake value and metabolic tumour volume on (1)(8)F-FDG PET/CT in oropharyngeal squamous cell carcinoma. Eur J Nucl Med Mol Imaging 42(9):1353–1361
Kim D, Kim W, Lee J, Ki Y, Lee B, Cho K, Kim S, Nam J, Lee J, Kim D (2016) Pretreatment maximum standardized uptake value of (18)F-fluorodeoxyglucose positron emission tomography as a predictor of distant metastasis in adenoid cystic carcinoma of the head and neck. Head Neck 38(5):755–761
Lasnon C, Desmonts C, Quak E, Gervais R, Do P, Dubos-Arvis C, Aide N (2013) Harmonizing SUVs in multicentre trials when using different generation PET systems: prospective validation in non-small cell lung cancer patients. Eur J Nucl Med Mol Imaging 40(7):985–996
Nair VJ, MacRae R, Sirisegaram A, Pantarotto JR (2014) Pretreatment [18F]-fluoro-2-deoxy-glucose positron emission tomography maximum standardized uptake value as predictor of distant metastasis in early-stage non-small cell lung cancer treated with definitive radiation therapy: rethinking the role of positron emission tomography in personalizing treatment based on risk status. Int J Radiat Oncol Biol Phys 88(2):312–318
Nam SJ, Roh JL, Cho KJ, Choi SH, Nam SY, Kim SY (2016) Risk Factors and survival associated with distant metastasis in patients with carcinoma of the salivary gland. Ann Surg Oncol 23(13):4376–4383
Pak K, Cheon GJ, Nam HY, Kim SJ, Kang KW, Chung JK, Kim EE, Lee DS (2014) Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: a systematic review and meta-analysis. J Nucl Med 55(6):884–890
Park GC, Roh JL, Cho KJ, Jin MH, Choi SH, Nam SY, Kim SY (2017a) ‘Incidence and risk factors of late recurrence in patients with salivary gland cancer’. Clin Otolaryngol 42(2):416–424
Park MJ, Oh JS, Roh JL, Kim JS, Lee JH, Nam SY, Kim SY (2017b) 18F-FDG PET/CT versus contrast-enhanced CT for staging and prognostic prediction in patients with salivary gland carcinomas. Clin Nucl Med 42(3):e149–e156
Pinkston JA, Cole P (1999) Incidence rates of salivary gland tumors: results from a population-based study. Otolaryngol Head Neck Surg 120(6):834–840
Razfar A, Heron DE, Branstetter BFt, Seethala RR, Ferris RL (2010) Positron emission tomography-computed tomography adds to the management of salivary gland malignancies. Laryngoscope 120(4):734–738
Roh JL, Ryu CH, Choi SH, Kim JS, Lee JH, Cho KJ, Nam SY, Kim SY (2007) Clinical utility of 18F-FDG PET for patients with salivary gland malignancies. J Nucl Med 48(2):240–246
Ryu IS, Kim JS, Roh JL, Lee JH, Cho KJ, Choi SH, Nam SY, Kim SY (2013) Prognostic value of preoperative metabolic tumor volume and total lesion glycolysis measured by 18F-FDG PET/CT in salivary gland carcinomas. J Nucl Med 54(7):1032–1038
Schoenfeld JD, Sher DJ, Norris CM Jr, Haddad RI, Posner MR, Balboni TA, Tishler RB (2012) Salivary gland tumors treated with adjuvant intensity-modulated radiotherapy with or without concurrent chemotherapy. Int J Radiat Oncol Biol Phys 82(1):308–314
Schwartz DL, Ford E, Rajendran J, Yueh B, Coltrera MD, Virgin J, Anzai Y, Haynor D, Lewellyn B, Mattes D, Meyer J, Phillips M, Leblanc M, Kinahan P, Krohn K, Eary J, Laramore GE (2005) FDG-PET/CT imaging for preradiotherapy staging of head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys 61(1):129–136
Seethala RR, Stenman G (2017) Tumours of the salivary gland. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ (eds) World Health Organization (WHO) classification of head and neck tumours, 4th edn. IARC Press, Lyon
Suh JD, Cho JH (2016) Trends in head and neck cancer in South Korea Between 1999 and 2012. Clin Exp Otorhinolaryngol 9(3):263–269
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Funding
This study was supported by a Grant (no. 2015R1A2A1A15054540) from Basic Science Research Program through the National Research Foundation of Korea (NRF), Ministry of Science and ICT, Seoul, Republic of Korea (J.L. Roh).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. Informed consent from all individual participants was waved because of the retrospective nature of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
432_2018_2760_MOESM1_ESM.tif
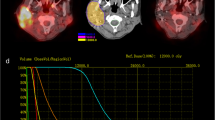
Supplementary Figure S1. Measurement of standardized uptake value (SUV) and metabolic tumor volume (MTV). The region of interest (circled) was set to include high grade salivary gland carcinoma (SGC) with metabolic activity, and software automatically calculated the SUVmax, SUVmean, SUVpeak and MTV. Total lesion glycolysis (TLG) was calculated as MTV × SUVmean. A 52-year old male patient (A) died of disease at 21 months after chemoradiotherapy for T4N2M1 salivary duct carcinoma, whereas 50-year old male patient (B) has been disease-free for 134 months since surgery plus radiotherapy for T2N0M0 high-grade carcinoma ex pleomorphic adenoma in the parotid gland. (TIF 3996 KB)
Rights and permissions
About this article
Cite this article
Almuhaimid, T.M., Lim, W.S., Roh, JL. et al. Pre-treatment metabolic tumor volume predicts tumor metastasis and progression in high-grade salivary gland carcinoma. J Cancer Res Clin Oncol 144, 2485–2493 (2018). https://doi.org/10.1007/s00432-018-2760-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-018-2760-z