Abstract
Purpose
Although association between colorectal cancer (CRC) and metabolic syndrome (MetS) is established, specific features of CRC arising in patients presenting with MetS have not been clearly identified.
Method
All patients who underwent colectomy for CRC from January 2005 to December 2014 at Institut Mutualiste Montsouris were identified from a prospectively collected database and characteristics were compared in the entire population and in a 1:2 matched case-control analysis [variables on which matching was performed were CRC localization (right- or left-sided) and AJCC stage (0 to IV)].
Results
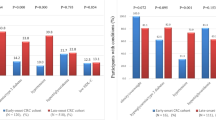
Out of the 772 identified patients, 98 (12.7%) presented with MetS. Entire population analysis revealed that CRC associated with MetS was more frequent in men (71.4 vs. 47.8%, p < 0.001), more often right-sided (71.4 vs. 50.4%, p < 0.001) and presented with less synchronous liver metastasis (4.1 vs. 8.7%, p = 0.002). Case-control analysis confirmed the gender association (p < 0.001) and showed HNPCC (p < 0.001) and history family of CRC (p = 0.010) to be significantly more frequent in Non-MetS patients.
Conclusions
CRC associated with MetS is more frequent in men, more often right-sided, and presents with fewer synchronous metastasis. Further investigations should be designed in order to confirm these results and to enhance our knowledge of carcinogenesis related to MetS.


Similar content being viewed by others
Abbreviations
- MetS:
-
Metabolic syndrome
- DM:
-
Diabetes mellitus
- ASA:
-
American Society of Anesthesiology
- COPD:
-
Chronic obstructive pulmonary disease
- CRC:
-
Colorectal cancer
- BMI:
-
Body mass index
- AJCC:
-
American Joint Committee on Cancer
- MSI:
-
Microsatellite instability
- HNPCC:
-
Hereditary non-polyposis colorectal cancer
- HCC:
-
Hepatocellular carcinoma
References
Haggar FA, Boushey RP (2009) Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg 22(4):191–197. https://doi.org/10.1055/s-0029-1242458
Suchanek S, Grega T, Ngo O, Vojtechova G, Majek O, Minarikova P, Brogyuk N, Bunganic B, Seifert B, Dusek L, Zavoral M (2016) How significant is the association between metabolic syndrome and prevalence of colorectal neoplasia? World J Gastroenterol 22:8103–8111. https://doi.org/10.3748/wjg.v22.i36.8103
Favoriti P, Carbone G, Greco M, Pirozzi F, Pirozzi RE, Corcione F (2016) Worldwide burden of colorectal cancer: a review. Updat Surg 68:7–11. https://doi.org/10.1007/s13304-016-0359-y
Rogers J, Stratta RJ, Lo A, Alloway RR (2005) Impact of the metabolic syndrome on long-term outcomes in simultaneous kidney-pancreas transplantation. Transplant Proc 37:3549–3551
Kimura K, Sawa A, Akagi S, Kihira K (2007) Development of a surgical site infection (SSI) surveillance system, calculation of SSI rates and specification of important factors affecting SSI in a digestive organ surgical department. Hiroshima J Med Sci 56:1–9
Champagne BJ, Nishtala M, Brady JT, Crawshaw BP, Franklin ME, Delaney CP, Steele SR (2017) Laparoscopic colectomy in the obese, morbidly obese, and super morbidly obese: when does weight matter? Int J Color Dis 32:1447–1451. https://doi.org/10.1007/s00384-017-2865-x
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F, American Heart Association, National Heart, Lung, and Blood Institute (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 112:2735–2752
Jeppesen J, Hansen TW, Rasmussen S, Ibsen H, Torp-Pedersen C, Madsbad S (2007) Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease: a population-based study. J Am Coll Cardiol 49:2112–2119
Lin SX, Pi-Sunyer EX (2007) Prevalence of the metabolic syndrome among US middle-aged and older adults with and without diabetes-a preliminary analysis of the NHANES 1999–2002 data. Ethn Dis 17:35–39
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ (2010) The metabolic syndrome. Lancet 375:181–183
Ahmed RL, Schmitz KH, Anderson KE, Rosamond WD, Folsom AR (2006) The metabolic syndrome and risk of incident colorectal cancer. Cancer 107:28–36
Stocks T, Lukanova A, Bjorge T, Ulmer H, Manjer J, Almquist M et al (2011) Metabolic factors and the risk of colorectal cancer in 580,000 men and women in the metabolic syndrome and cancer project (Me-Can). Cancer 117:2398–2407
Lu Y, Ness-Jensen E, Hveem K, Martling A (2015) Metabolic predispositions and increased risk of colorectal adenocarcinoma by anatomical location: a large population-based cohort study in Norway. Am J Epidemiol 182:883–893. https://doi.org/10.1093/aje/kwv141
Yki-Järvinen H (2014) Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol 2:901–910. https://doi.org/10.1016/S2213-8587(14)70032-4
Arnlöv J, Sundström J, Ingelsson E, Lind L (2011) Impact of BMI and the metabolic syndrome on the risk of diabetes in middle-aged men. Diabetes Care 34:61–65. https://doi.org/10.2337/dc10-0955
Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo M, Pukkala E, Skytthe A, Hemminki K (2000) Environmental and heritable factors in the causation of cancer—analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med 343:78–85
Carethers JM, Stoffel EM (2015) Lynch syndrome and Lynch syndrome mimics: the growing complex landscape of hereditary colon cancer. World J Gastroenterol 21:9253–9261
Itzkowitz SH, Present DH (2005) Consensus conference: colorectal cancer screening and surveillance in inflammatory bowel disease. Inflamm Bowel Dis 11:314–321
Ficari F, Cama A, Valanzano R, Curia MC, Palmirotta R, Aceto G, Esposito DL, Crognale S, Lombardi A, Messerini L, Mariani-Costantini R, Tonelli F, Battista P (2000) APC gene mutations and colorectal adenomatosis in familial adenomatous polyposis. Br J Cancer 82:348–353
Boland CR, Goel A (2010) Microsatellite instability in colorectal cancer. Gastroenterology 138:2073–2087.e3
Edge SBBDR, Compton CC, Fritz AG, Green FL, Trotti A (eds) (2010) AJCC Cancer staging manual (ed 7th edition). Springer, New York
Washington MK, Berlin J, Branton P, Burgart LJ, Carter DK, Fitzgibbons PL, Halling K, Frankel W, Jessup J, Kakar S, Minsky B, Nakhleh R, Compton CC (eds) (2009) Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum. Arch Pathol Lab Med 133:1539–1551
Lohsiriwat V, Pongsanguansuk W, Lertakyamanee N, Lohsiriwat D (2010) Impact of metabolic syndrome on the short-term outcomes of colorectal cancer surgery. Dis Colon rectum 53:186–191. https://doi.org/10.1007/DCR.0b013e3181bdbc32
Tee MC, Ubl DS, Habermann EB, Nagorney DM, Kendrick ML, Sarr MG, Truty MJ, Que FG, Reid-Lombardo K, Smoot RL, Farnell MB (2016) Metabolic syndrome is associated with increased postoperative morbidity and hospital resource utilization in patients undergoing elective pancreatectomy. J Gastrointest Surg 20:189–98; discussion 198. https://doi.org/10.1007/s11605-015-3007-9
Zarzavadjian Le Bian A, Costi R, Constantinides V, Smadja C (2012) Metabolic disorders, non-alcoholic fatty liver disease and major liver resection: an underestimated perioperative risk. J Gastrointest Surg 16:2247–2255. https://doi.org/10.1007/s11605-012-2044-x
Cauchy F, Zalinski S, Dokmak S, Fuks D, Farges O, Castera L, Paradis V, Belghiti J (2013) Surgical treatment of hepatocellular carcinoma associated with the metabolic syndrome. Br J Surg 100:113–121. https://doi.org/10.1002/bjs.8963
Piscaglia F, Svegliati-Baroni G, Barchetti A, Pecorelli A, Marinelli S, Tiribelli C, Bellentani S, HCC-NAFLD Italian Study roup (2016) Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: a multicenter prospective study. Hepatology 63:827–838. https://doi.org/10.1002/hep.28368.
Rahman R, Hammoud GM, Almashhrawi AA, Ahmed KT, Ibdah JA (2013) Primary hepatocellular carcinoma and metabolic syndrome: an update. World J Gastrointest Oncol 5:186–194. https://doi.org/10.4251/wjgo.v5.i9.186
Paradis V, Zalinski S, Chelbi E, Guedj N, Degos F, Vilgrain V, Bedossa P, Belghiti J (2009) Hepatocellular carcinomas in patients with metabolic syndrome often develop without significant liver fibrosis: a pathological analysis. Hepatology 49:851–859
Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D (2012) Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care 35:2402–2411
Russo A, Autelitano M, Bisanti L (2008) Metabolic syndrome and cancer risk. Eur J Cancer 44:293–297
Ibrahim YH, Yee D (2004) Insulin-like growth factor-I and cancer risk. Growth Hormon IGF Res 14:261–269
Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56:549–580
Pelucchi C, Negri E, Talamini R et al (2010) Metabolic syndrome is associated with colorectal cancer in men. Eur J Cancer 4610:1866–1872
Healy LA, Howard JM, Ryan AM et al (2012) Metabolic syndrome and leptin are associated with adverse pathological features in male colorectal cancer patients. Color Dis 142:157–165
Aleksandrova K, Boeing H, Jenab M et al (2011) Metabolic syndrome and risks of colon and rectal cancer: the European prospective investigation into cancer and nutrition study. Cancer Prev Res (Phila) 411:1873–1883
Kabat GC, Kim MY, Peters U et al (2012) A longitudinal study of the metabolic syndrome and risk of colorectal cancer in postmenopausal women. Eur J Cancer Prev 214:326–332
Harima S, Hashimoto S, Shibata H et al (2013) Correlations between obesity/metabolic syndrome-related factors and risk of developing colorectal tumors. Hepato-Gastroenterology 60124:733–737
Gupta S, Naini BV, Munoz R, Graham RP, Kipp BR, Torbenson MS, Mounajjed T (2016 Apr) Hepatocellular neoplasms arising in association with androgen use. Am J Surg Pathol 40(4):454–461. https://doi.org/10.1097/PAS.0000000000000576
Ko S, Yoon SJ, Kim D, Kim AR, Kim EJ, Seo HY (2016) Metabolic risk profile and cancer in Korean men and women. J Prev Med Public Health 49:143–152. https://doi.org/10.3961/jpmph.16.021
Calle EE, Kaaks R (2004) Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 4:579–591
McMichael AJ, Potter JD (1980) Reproduction, endogenous and exogenous sex hormones, and colon cancer: a review and hypothesis. J Natl Cancer Inst 65:1201–1207
Pucci G, Alcidi R, Tap L, Battista F, Mattace-Raso F, Schillaci G (2017 Jun) Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: a review of the literature. Pharmacol Res 120:34–42. https://doi.org/10.1016/j.phrs.2017.03.008
Chiu HM, Lin JT, Shun CT et al (2007) Association of metabolic syndrome with proximal and synchronous colorectal neoplasm. Clin Gastroenterol Hepatol 52:221–229 quiz 141
Komuro K, Tada M, Tamoto E, Kawakami A, Matsunaga A, Teramoto K, Shindoh G, Takada M, Murakawa K, Kanai M, Kobayashi N, Fujiwara Y, Nishimura N, Hamada JI, Ishizu A, Ikeda H, Kondo S, Katoh H, Moriuchi T, Yoshiki T (2005) Right- and left-sided colorectal cancers display distinct expression profiles and the anatomical stratification allows a high accuracy prediction of lymph node metastasis. J Surg Res 124:216–224
Robsahm TE, Aagnes B, Hjartåker A, Langseth H, Bray FI, Larsen IK (2013) Body mass index, physical activity, and colorectal cancer by anatomical subsites: a systematic review and meta-analysis of cohort studies. Eur J Cancer Prev 22:492–505. https://doi.org/10.1097/CEJ.0b013e328360f434
Ussar S, Griffin NW, Bezy O, Fujisaka S, Vienberg S, Softic S, Deng L, Bry L, Gordon JI, Kahn CR (2015) Interactions between gut microbiota, host genetics and diet modulate the predisposition to obesity and metabolic syndrome. Cell Metab 22:516–530. https://doi.org/10.1016/j.cmet.2015.07.007
Vogtmann E, Flores R, Yu G, Freedman ND, Shi J, Gail MH, Dye BA, Wang GQ, Klepac-Ceraj V, Paster BJ, Wei WQ, Guo HQ, Dawsey SM, Qiao YL, Abnet CC (2015) Association between tobacco use and the upper gastrointestinal microbiome among Chinese men. Cancer Causes Control 26:581–588
Murono K, Kitayama J, Tsuno NH, Nozawa H, Kawai K, Sunami E, Akahane M, Watanabe T (2013) Hepatic steatosis is associated with lower incidence of liver metastasis from colorectal cancer. Int J Color Dis 28:1065–1072. https://doi.org/10.1007/s00384-013-1656-2
Shen Z, Ye Y, Bin L, Yin M, Yang X, Jiang K, Wang S (2010) Metabolic syndrome is an important factor for the evolution of prognosis of colorectal cancer: survival, recurrence, and liver metastasis. Am J Surg 200:59–63. https://doi.org/10.1016/j.amjsurg.2009.05.005
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Zarzavadjian Le Bian, A., Denet, C., Tabchouri, N. et al. Specific features of colorectal cancer in patients with metabolic syndrome: a matched case-control analysis of 772 patients. Langenbecks Arch Surg 403, 443–450 (2018). https://doi.org/10.1007/s00423-018-1677-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1677-y