Abstract
Purpose
The clinical investigation of exertional intolerance generally focuses on cardiopulmonary diseases, while peripheral factors are often overlooked. We hypothesize that a subset of patients exists whose predominant exercise limitation is due to abnormal systemic oxygen extraction (SOE).
Methods
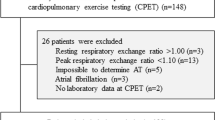
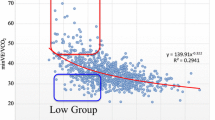
We reviewed invasive cardiopulmonary exercise test (iCPET) results of 313 consecutive patients presenting with unexplained exertional intolerance. An exercise limit due to poor SOE was defined as peak exercise (Ca-vO2)/[Hb] ≤ 0.8 and VO2max < 80% predicted in the absence of a cardiac or pulmonary mechanical limit. Those with peak (Ca-vO2)/[Hb] > 0.8, VO2max ≥ 80%, and no cardiac or pulmonary limit were considered otherwise normal. The otherwise normal group was divided into hyperventilators (HV) and normals (NL). Hyperventilation was defined as peak PaCO2 < [1.5 × HCO3 + 6].
Results
Prevalence of impaired SOE as the sole cause of exertional intolerance was 12.5% (32/257). At peak exercise, poor SOE and HV had less acidemic arterial blood compared to NL (pHa = 7.39 ± 0.05 vs. 7.38 ± 0.05 vs. 7.32 ± 0.02, p < 0.001), which was explained by relative hypocapnia (PaCO2 = 29.9 ± 5.4 mmHg vs. 31.6 ± 5.4 vs. 37.5 ± 3.4, p < 0.001). For a subset of poor SOE, this relative alkalemia, also seen in mixed venous blood, was associated with a normal PvO2 nadir (28 ± 2 mmHg vs. 26 ± 4, p = 0.627) but increased SvO2 at peak exercise (44.1 ± 5.2% vs. 31.4 ± 7.0, p < 0.001).
Conclusions
We identified a cohort of patients whose exercise limitation is due only to systemic oxygen extraction, due to either an intrinsic abnormality of skeletal muscle mitochondrion, limb muscle microcirculatory dysregulation, or hyperventilation and left shift the oxyhemoglobin dissociation curve.





Similar content being viewed by others
Abbreviations
- BWH:
-
Brigham and Women’s Hospital
- CaO2 :
-
Oxygen content in arterial blood
- Ca-vO2 :
-
Difference between oxygen content in arterial and venous blood
- CI:
-
Cardiac index
- CvO2 :
-
Oxygen content in mixed venous blood
- DBP:
-
Diastolic blood pressure
- [Hb]:
-
Hemoglobin concentration
- HCO3 :
-
Bicarbonate
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HR:
-
Heart rate
- HV:
-
Hyperventilators
- iCPET:
-
Invasive cardiopulmonary exercise testing
- LVEF:
-
Left ventricular ejection fraction
- MAP:
-
Mean arterial pressure
- MM:
-
Mitochondrial myopathies
- mPAP:
-
Mean pulmonary arterial pressure
- NL:
-
Normal subjects
- PaCO2 :
-
Partial pressure of carbon dioxide in arterial blood
- PAH:
-
Pulmonary arterial hypertension
- PaO2 :
-
Partial pressure of oxygen in arterial blood
- PCWP:
-
Pulmonary capillary wedge pressure
- PH:
-
Pulmonary hypertension
- pHa:
-
Arterial pH
- pHv:
-
Venous pH
- PML:
-
Pulmonary mechanical limit
- PvCO2 :
-
Partial pressure of carbon dioxide in venous blood
- PvO2 :
-
Partial pressure of oxygen in venous blood
- PVR:
-
Pulmonary vascular resistance
- Q t :
-
Cardiac output
- Q tmax :
-
Cardiac output at maximum exercise
- RAP:
-
Right atrial pressure
- RER:
-
Respiratory exchange ratio
- RR:
-
Respiratory rate
- SaO2 :
-
Oxygen saturation in arterial blood
- SBP:
-
Systolic blood pressure
- SOE:
-
Systemic oxygen extraction
- SOEH :
-
Poor SOE group with high PvO2
- SOEL:
-
Poor SOE group with low PvO2
- SVR:
-
Systemic vascular resistance
- SvO2 :
-
Oxygen saturation in mixed venous blood
- VCO2 :
-
Carbon dioxide output
- V E :
-
Minute ventilation
- V Emax :
-
Minute ventilation at peak exercise
- VO2 :
-
Oxygen uptake
- VO2max :
-
Maximum oxygen uptake
References
Aaker A, Laughlin MH (2002) Diaphragm arterioles are less responsive to alpha1-adrenergic constriction than gastrocnemius arterioles. J Appl Physiol 92(5):1808–1816
Aaron EA, Johnson BD, Seow CK, Dempsey JA (1992) Oxygen cost of exercise hyperpnea: measurement. J Appl Physiol 72(5):1810–1817
Abudiab MM, Redfield MM, Melenovsky V, Olson TP, Kass DA, Johnson BD, Borlaug BA (2013) Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail 15(7):776–785
Albert MS, Dell RB, Winters RW (1967) Quantitative displacement of acid–base equilibrium in metabolic acidosis. Ann Intern Med 66(2):312–322
Amann M, Blain GM, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA (2010) Group III and IV muscle afferents contribute to ventilatory and cardiovascular response to rhythmic exercise in humans. J Appl Physiol 109(4):966–976
Arena R, Meyers J, Aslam SS, Varughese EB, Peberdy MA (2003) Technical considerations related to the minute ventilation/carbon dioxide output slope in patients with heart failure. Chest 124(2):720–727
Argov Z, Bank WJ, Maris J, Peterson P, Chance B (1987) Bioenergetic heterogeneity of human mitochondrial myopathies: phosphorus magnetic resonance spectroscopy study. Neurology 37(2):257–262
Arnold DL, Taylor DJ, Radda GK (1985) Investigation of human mitochondrial myopathies by phosphorus magnetic resonance spectroscopy. Ann Neurol 18(2):189–196
Bested AC, Marshall LM (2015) Review of myalgic encephalomyelitis/chronic fatigue syndrome: an evidenced-based approach to diagnosis and management by clinicians. Rev Environ Health 30(4):223–249
Bhella PS, Prasad A, Heinicke K, Hastings JL, Arbab-Zadeh A, Adams-Huet B, Pacini EL, Shibata S, Palmer MD, Newcomer BR, Levine BD (2011) Abnormal haemodynamic response to exercise in heart failure with preserved ejection fraction. Eur J Heart Fail 13(12):1296–1304
Boerrigter BG, Waxman AB, Westerhof N, Vonk-Noordegraaf A, Systrom DM (2014) Measuring central pulmonary pressures during exercise in COPD: how to cope with respiratory effects. Eur Respir J 43(5):1316–1325
Borlaug BA, Nishimura RA, Sorajja P, Lam CSP, Redfield MM (2010) Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail 3(5):588–595
Bravo DM, Gimenes AC, Nascimento RB, Ferreira EV, Siqueira AC, Meda ED, Neder JA, Nery LE (2012) Skeletal muscle reoxygenation after high-intensity exercise in mitochondrial myopathy. Eur J Appl Physiol 112(5):1763–1771
Brudin T (1975) Temperature of mixed venous blood during exercise. Scand J Clin Lab Invest 35(6):539–543
Calbet JA, Boushel R (2015) Assessment of cardiac output with transpulmonary thermodilution during exercise in humans. J Appl Physiol 118(1):1–10
Carrick-Ranson G, Hastings JL, Bhella PS, Fujimoto N, Shibata S, Palmer MD, Boyd K, Livingston S, Dijk E, Levine BD (2014) The effect of lifelong exercise dose on cardiovascular function during exercise. J Appl Physiol 116(7):736–745
Chin LM, Heigenhauser GJ, Paterson DH, Kowalchuk JM (2010) Pulmonary O2 uptake and leg blood flow kinetics during moderate exercise are slowed by hyperventilation-induced hypocapnic alkalosis. J Appl Physiol 108(6):1641–1650
Chin LM, Heigenhauser GJ, Paterson DH, Kowalchuk JM (2013) Effect of voluntary hyperventilation with supplemental CO2 on pulmonary O2 uptake and leg blood flow kinetics during moderate-intensity exercise. Exp Physiol 98(12):1668–1682
Chinnery PF, Johnson MA, Wardell TM, Singh-Kler R, Hayes C, Brown DT, Taylor RW, Bindoff LA, Turnbull DM (2000) The epidemiology of pathogenic mitochondrial DNA mutations. Ann Neurol 48(2):188–193
Dhakal BP, Malhotra R, Murphy RM, Pappagianopoulos PP, Baggish AL, Weiner RB, Houstis NE, Eisman AS, Hough SS, Lewis GD (2015) Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: the role of abnormal peripheral oxygen extraction. Circ Heart Fail 8(2):286–294
Eldridge FL (1994) Central integration of mechanisms in exercise hyperpnea. Med Sci Sports Exerc 26(3):319–327
Elliot DL, Buist NR, Goldberg L, Kennaway NG, Powell BR, Kuehl KS (1989) Metabolic myopathies: evaluation by graded exercise testing. Medicine (Baltimore) 68(3):163–172
Evans AB, Tsai LW, Oelberg DA, Kazemi H, Systrom DM (1998) Skeletal muscle ECF pH error signal for exercise ventilatory control. J Appl Physiol 84(1):90–96
Flaherty KR, Wald J, Weisman IM, Zeballos RJ, Schork MA, Blaivas M, Rubenfire M, Martinez FJ (2001) Unexplained exertional limitation: characterization of patients with a mitochondrial myopathy. Am J Respir Crit Care Med 164(3):425–432
Gimenes AC, Neder JA, Dal Corso S, Nogueira CR, Nápolis L, Mello MT, Bulle AS, Nery LE (2011) Relationship between work rate and oxygen uptake in mitochondrial myopathy during ramp-incremental exercise. Braz J Med Biol Res 44(4):354–360
Greaney JL, Schwartz CE, Edwards DG, Fadel PJ, Farquhar WB (2013) The neural interaction between the arterial baroreflex and muscle metaboreflex is preserved in older men. Exp Physiol 98(10):1422–1431
Groves BM, Reeves JT, Sutton JR, Wagner PD, Cymerman A, Malconian MK, Rock PB, Young PM, Houston CS (1987) Operation everest II: elevated high-altitude pulmonary resistance unresponsive to oxygen. J Appl Physiol 63(2):521–530
Guazzi M, Reina G, Tumminello G, Guazzi MD (2005) Exercise ventilation inefficiency and the cardiovascular mortality in heart failure: the critical independent prognostic value of the arterial CO2 partial pressure. Eur Heart J 26(5):472–480
Hansen JE (1989) Arterial bood gas. Clin in Chest Med 10(2):227–237
Hansen JE, Sue DY, Wasserman K (1984) Predicted values for clinical exercise testing. Am Rev Respir Dis 129(2):S49–S55
Hayashi N, Ishihara M, Tanaka A, Yoshida T (1999) Impeding O(2) unloading in muscle delays oxygen uptake repsonse to exercise onset in humans. Am J Physiol 277(5):R1274–1281
Haykowsky MJ, Brubaker PH, John JM, Stewart KP, Morgan TM, Kitzman DW (2011) Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. J Am Coll Cardiol 58(3):265–274
Heinicke K, Taivassalo T, Wyrick P, Wood H, Babb TG, Haller RG (2011) Exertional dyspnea in mitochondrial myopathy: clinical features and physiological mechanisms. Am J Physiol Regul Integr Comp Physiol 301(4):R873–R884
Jensen TD, Kazemi-Esfarjani P, Skomorowska E, Vissing J (2002) A forearm exercise screening test for mitochondrial myopathy. Neurology 58(10):1533–1538
Kaufman MP (2010) Control of breathing during dynamic exercise by thin fiber muscle afferents. J Appl Physiol 109(4):947–948
Kaufman MP, Hayes SG (2002) The exercise pressor reflex. Clin Auton Res 12(6):429–439
Kowalchuk JM, Heigenhauser GJ, Lindinger MI, Sutton JR, Jones NL (1988) Factors influences hydrogen ion concentration in muscle after intense exercise. J Appl Physiol 65(5):2080–2089
Lindholm H, Löfberg M, Somer H, Näveri H, Sovijärvi A (2004) Abnormal blood lactate accumulation after exercise in patients with multiple mitochondrial DNA deletions and minor muscular symptoms. Clin Physiol Funct Imaging 24(2):109–115
Mar PL, Raj SR (2014) Neuronal and hormonal perturbations in postural tachycardia syndrome. Front Physiol 5(220):1–8
Maron BA, Cockrill BA, Waxman AB, Systrom DM (2013) Invasive cardiopulmonary exercise test. Circulation 127(10):1157–1164
Meulemans A, Gerlo E, Seneca S, Lissens W, Smet J, Van Coster R, De Meirleir L (2007) The aerobic forearm exercise test, a non-invasive tool to screen for mitochondrial disorders. Acta Neurol Belg 107(3):78–83
Oelberg DA, Evans AB, Hrovat MI, Pappagianopoulos PP, Patz S, Systrom DM (1998) Skeletal muscle chemoreflex and pHi in exercise ventilatory control. J Appl Physiol 84(2):676–682
Piepoli MF, Crisafulli A (2014) Pathophysiology of human heart failure: importance of skeletal muscle myopathy and reflexes. Exp Physiol 99(4):609–615
Pinkstaff S, Peberdy MA, Kontos MC, Finucane S, Arena R (2010) Quantifying exertion level during exercise stress testing using percentage of age-predicted maximal heart rate, rate pressure product, and perceived exertion. Mayo Clin Proc 85(12):1095–1100
Reeves JT, Moon RE, Grover RF, Groves BM (1988) Increased wedge pressure facilitates decreased lung vascular resistance during upright exercise. Chest 93(3):97S–99S
Santos M, Opotowsky AR, Shah AM, Tracy J, Waxman AB, Systrom DM (2015) Central cardiac limit to aerobic capacity in patients with exertional pulmonary venous hypertension: implications for heart failure with preserved ejection fraction. Circ Heart Fail 8(2):278–285
Stewart JM (2002) Pooling in chronic orthostatic intolerance: arterial vasoconstrictive but not venous compliance defects. Circulation 105(19):2274–2281
Stringer W, Wasserman K, Casaburi R, Pórszász J, Maehara K, French W (1994) Lactic acidosis as a facilitator of oxyhemoglobin dissociation during exercise. J Appl Physiol 76(4):1462–1467
Taivassalo T, Abbott A, Wyrick P, Haller RG (2002) Venous oxygen levels during aerobic forearm exercise: an index of impaired oxidative metabolism in mitochondrial myopathy. Ann Neurol 51(1):38–44
Taivassalo T, Jensen TD, Kennaway N, DiMauro S, Vissing J, Haller RG (2003) The spectrum of exercise tolerance in mitochondrial myopathies: a study of 40 patients. Brain 126(2):413–423
Tarnopolsky M (2004) Exercise testing as a diagnostic entity in mitochondrial myopathies. Mitochondrion 4(5–6):529–542
Tarnopolsky MA, Raha S (2005) Mitochondrial myopathies: diagnosis, exercise intolerance, and treatment options. Med Sci Sports Exerc 37(12):2086–2093
Taylor DJ, Kemp GJ, Radda GK (1994) Bioenergetics of skeletal muscle in mitochondrial myopathy. J Neurol Sci 127(2):198–206
Tolle J, Waxman A, Systrom D (2008a) Impaired systemic oxygen extraction at maximum exercise in pulmonary hypertension. Med Sci Sports Exerc 40(1):3–8
Tolle JJ, Waxman AB, Van Horn TL, Pappagianopoulos PP, Systrom DM (2008b) Exercise-induced pulmonary arterial hypertension. Circulation 118(21):2183–2189
Trenell MI, Sue CM, Kemp GJ, Sachinwalla T, Thompson CH (2006) Aerobic exercise and muscle metabolism in patients with mitochondrial myopathy. Muscle Nerve 33(4):524–531
Vissing J, MacLean DA, Vissing SF, Sander M, Saltin B, Haller RG (2001) The exercise metaboreflex is maintained in the absence of muscle acidosis: insights from muscle microdialysis in humans with McArdle’s disease. J Physiol 537(2):641–649
Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsma KE, Sun XG, Whipp BJ (2012) Principles of exercise testing and interpretation, 5th edn. Lipincott Williams & Wilkins, Philadelphia
Wasserman K, Cox T, Sietsema KE (2014) Ventilatory regulation of arterial H(+) (pH) during exercise. Respir Physiol Neurobiol 190:142–148
Williamson JW (2010) The relevance of central command for the neural cardiovascular control of exercise. Exp Physiol 95(11):1043–1048
Acknowledgements
Julie Tracy, MS.
Funding
Funding was received from Solve ME/CFS Foundation (DS).
Author information
Authors and Affiliations
Contributions
KM, MS, RO, MU, AO, AW, and DS performed data collection and analysis. DF and DM performed study design. KM and DS wrote the manuscript. All the authors reviewed, edited, and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
ABW and DMS funded by NIH 2R01HL060234-12A1 and U01HL125215-01. ARO supported by the Dunlevie Family Fund. The remaining authors have no conflicts of interest.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by I. Mark Olfert.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Melamed, K.H., Santos, M., Oliveira, R.K.F. et al. Unexplained exertional intolerance associated with impaired systemic oxygen extraction. Eur J Appl Physiol 119, 2375–2389 (2019). https://doi.org/10.1007/s00421-019-04222-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-019-04222-6