Abstract
Purpose
The purpose of this study is to describe cornea verticillata in Fabry disease and in amiodarone-induced keratopathy and to compare the corneal microstructure of both types.
Patients and methods
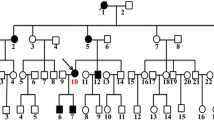
Ten eyes from ten normal subjects, 28 eyes from 22 patients with Fabry disease confirmed by molecular genetic studies, and 16 eyes from 11 patients receiving amiodarone were examined by slit-lamp microscopy and in-vivo confocal laser-scanning microscopy (CLSM) with following three-dimensional reconstruction of the individual corneal layers. Five patients with Fabry disease were monitored during the course of enzyme replacement therapy (ERT).
Results
Evidence of cornea verticillata was found by slit-lamp microscopy both in patients with Fabry disease and in those with amiodarone-induced keratopathy; CLSM revealed the same pattern of hyper-reflective deposits in the basal cell layer of corneal epithelium in both sets of patients. Microdot changes in the anterior stroma were more prevalent in patients receiving amiodarone but do not presuppose the simultaneous presence of cornea verticillata. The bulbar conjunctiva was found to be normal in all patients. The tarsal conjunctival epithelium contained round hyper-reflective structures, which are also encountered physiologically, but these were more common in patients with Fabry disease. In one out of the five patients examined, monitoring of corneal changes over time during ERT disclosed a regressive tendency of the deposits in the epithelial basal cell layer documented by CLSM.
Conclusions
The microstructural corneal changes typically seen in cornea verticillata in both Fabry disease and in amiodarone-induced keratopathy can be successfully visualized by confocal in-vivo microscopy at the level of the basal cell layer. By analogy, with the grading system for cornea verticillata based on slit-lamp microscopy, staging of these deposits in the basal cell layer can also be performed following in-vivo CLSM. The microdots in the anterior stroma as well as the changes observed in the tarsal conjunctiva should be regarded as having less diagnostic value because such changes may also occur in normal subjects. The utility of CLSM as a tool for monitoring ERT in Fabry disease over time needs to be confirmed in studies with larger sample sizes conducted over a longer period.





Similar content being viewed by others
References
Fleischer B (1910) Über eine eigenartige bisher nicht bekannte Hornhauttrübung. Albrecht Graefes Arch Ophthalmologie 77:136–140 doi:10.1007/BF02229811
François J (1969) Cornea verticillata. Doc Ophthalmol 27:235–251 Den Haag doi:10.1007/BF00208693
François J, Hanssens M, Teuchy H (1978) Corneal ultrastructural changes in Fabry’s disease. Ophthalmologica 176:313–330
Denden A (1966) Über die Erblichkeit der Dystrophia cornea verticillata. Albrecht Von Graefes Arch Klin Exp Ophthalmol 169:264–271 doi:10.1007/BF00429345
Grau AJ, Schwaninger M, Goebel HH, Beck M (2003) Morbus Fabry: Eine lysosomale Stoffwechselerkrankung mit neuen therapeutischen Möglichkeiten. Nervenarzt 74:489–496 doi:10.1007/s00115-003-1577-3
Witschel H, Meyer W (1968) Der Morbus Fabry als Beispiel einer erblichen Lipoidspeicherkrankheit: neuere Gesichtspunkte zur Pathogenese, Klinik und Morphologie. Klin Wochenschr 46:72–76 doi:10.1007/BF01747471
Mehta A, Ricci R, Widmer U et al (2004) Fabry disease defined: baseline clinical manifestations of 366 patients in the Fabry Outcome Survey. Eur J Clin Invest 34:236–242 doi:10.1111/j.1365-2362.2004.01309.x
Ries M, Ramaswami U, Parini R et al (2003) The early clinical phenotype of Fabry disease: a study on 35 European children and adolescents. Eur J Pediatr 162:767–772 doi:10.1007/s00431-003-1299-3
Orssaud C, Dufier JL, Germain DP (2003) Ocular manifestations in Fabry disease: a survey of 32 hemizygous male patients. Ophthalmic Genet 24:129–139 doi:10.1076/opge.24.3.129.15609
Sher NA, Letson RD, Desnick RJ (1979) The ocular manifestations in Fabry’s disease. Arch Ophthalmol 97:671–676
Andersen M, Dahl H, Fledelius H, Nielsen N (1994) Central artery occlusion in a patient with Fabry’s disease documented by scanning laser ophthalmoscopy. Acta Ophthalmol (Copenh) 72:635–638
Nguyen TT, Gin T, Nicholls K et al (2005) Ophthalmological manifestations of Fabry disease: a survey of patients at the Royal Melbourne Fabry Disease Treatment Centre. Clin Experiment Ophthalmol 33:164–168 doi:10.1111/j.1442-9071.2005.00990.x
Ohkubo H (1988) Several functional and fluorescein fundus angiographic findings in Fabry’s disease. Ophthalmologica 196:132–136
Sodi A, Ioannidis AS, Mehta A et al (2007) Ocular manifestations of Fabry’s disease: data from the Fabry Outcome Survey. Br J Ophthalmol 91:210–214 doi:10.1136/bjo.2006.100602
Eng CM, Banikazemi M, Gordon RE 3rd et al (2001) A phase 1/2 clinical trial of enzyme replacement in Fabry disease: pharmacokinetic, substrate clearance, and safety studies. Am J Hum Genet 68:711–722 doi:10.1086/318809
Schiffmann R, Kopp JB, Austin HA 3rd et al (2001) Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA 285:2743–2749 doi:10.1001/jama.285.21.2743
Roussel T, Grutzmacher R, Coster D (1984) Patterns of superficial keratopathy. Aust J Ophthalmol 12:301–316 doi:10.1111/j.1442-9071.1984.tb01174.x
Seiler KU, Thiel HJ, Wassermann O (1977) Die Chloroquinkeratopathie als Beispiel einer arzneimittelinduzierten Phospholipidosis (zugleich ein Beitrag zur Pathogenese der Cornea verticillata). Klin Monatsbl Augenheilkd 170:64–73
Bangham AD, Dawson RMC (1959) The relation between the activity of a lecithinase and the electrophoretic charge of the substrate. Biochem J 72:486–492
Stave J, Zinser G, Grümmer G, Guthoff RF (2002) Der modifizierte Heidelberg-Retina-Tomograph HRT. Erste Ergebnisse einer In-vivo-Darstellung von kornealen Strukturen. Ophthalmologe 99:276–280 doi:10.1007/s003470100535
Eckard A, Stave J, Guthoff RF (2006) In vivo investigations of the corneal epithelium with the confocal Rostock Laser Scanning Microscope (RLSM). Cornea 25:127–131 doi:10.1097/01.ico.0000170694.90455.f7
Guthoff RF, Stave J (2006) In vivo micromorphology of the cornea: confocal microscopy principles and clinical applications. In: Reinhard T, Larkin F (eds) Essentials in ophthalmology: cornea and external eye disease. Springer, Berlin Heidelberg New York, pp 173–208
Guthoff RF, Wienss H, Hahnel C, Wree A (2005) Epithelial innervation of human cornea: a three-dimensional study using confocal laser scanning fluorescence microscopy. Cornea 24:608–613 doi:10.1097/01.ico.0000154384.05614.8f
Hahnel C, Somodi S, Weiss DG, Guthoff RF (2000) The keratocyte network of human cornea: a three-dimensional study using confocal laser scanning fluorescence microscopy. Cornea 19:185–193 doi:10.1097/00003226-200003000-00012
Orlando RG, Dangel ME, Schaal SF (1984) Clinical experience and grading of amiodarone keratopathy. Ophthalmology 91:1184–1187
Dolan BJ, Flach AJ, Peterson JS (1985) Amiodarone keratopathy and lens opacities. J Am Optom Assoc 56:468–470
Ciancaglini M, Carpineto P, Zuppardi E et al (2001) In vivo confocal microscopy of patients with amiodarone-induced keratopathy. Cornea 20:368–373 doi:10.1097/00003226-200105000-00007
Rath R, Stave J, Guthoff RF et al (2006) In-vivo-Darstellung des Bindehautepithels: eine vergleichende morphologische Untersuchung mittels konfokaler Laser-Scanning-Mikroskopie und Impressionszytologie. Ophthalmologe 103:401–405 doi:10.1007/s00347-006-1337-4
Fumex-Boizard L, Cochat P, Fouilhoux A et al (2005) Relation entre les manifestations ophtalmologiques et les atteintes générales chez dix patients atteints de la maladie de Fabry. J Fr Ophtalmol 28:45–50 doi:10.1016/S0181-5512(05)81024-1
Mastropasqua L, Nubile M, Lanzini M et al (2006) Corneal and conjunctival manifestations in Fabry disease: in vivo confocal microscopy study. Am J Ophthalmol 141:709–718 doi:10.1016/j.ajo.2005.11.053
Tsutsumi A, Uchida Y, Kanai T (1984) Corneal findings in a foetus with Fabry’s disease. Acta Ophthalmol (Copenh) 62:923–931
Hirano K, Murata K, Miyagawa A et al (2001) Histopathologic findings of cornea verticillata in a woman heterozygous for Fabry’s disease. Cornea 20:233–236 doi:10.1097/00003226-200103000-00028
Slowik C, Somodi S, von Gruben C et al (1997) Erfassung morphologischer Hornhautveränderungen infolge Chloroquintherapie mit Hilfe der konfokalen In-vivo-Mikroskopie. Ophthalmologe 94:147–151 doi:10.1007/s003470050096
Libert J, Tondeur M, Van Hoof F (1976) The use of conjunctival biopsy and enzyme analysis in tears for the diagnosis of homozygotes and heterozygotes with Fabry disease. Birth Defects Orig Artic Ser 12:221–239
Guthoff RF, Baudouin C, Stave J (2006) Atlas of confocal laser scanning in-vivo microscopy in ophthalmology. Springer, Berlin Heidelberg New York
Bastion ML, Mohamad MH (2006) Study of the factors associated with the presence of white dots in the corneas of regular soft contact lens users from an Asian country. Eye Contact Lens 32:223–227 doi:10.1097/01.icl.0000199891.35160.68
Macrae WG, Ghosh M, McCulloch C (1985) Corneal changes in Fabry’s disease: a clinico-pathologic case report of a heterozygote. Ophthalmic Paediatr Genet 5:185–190 doi:10.3109/13816818509006132
McCulloch C, Ghosh M (1984) Ultrastructural changes in the cornea and conjunctiva of a heterozygous woman with Fabry’s disease. Can J Ophthalmol 19:192–198
Knop E, Knop N (2005) The role of eye-associated lymphoid tissue in corneal immune protection. J Anat 206:271–285 doi:10.1111/j.1469-7580.2005.00394.x
Knop N, Knop E (2000) Conjunctiva-associated lymphoid tissue in the human eye. Invest Ophthalmol Vis Sci 41:1270–1279
D’Amico DJ, Kenyon KR (1981) Drug-induced lipidoses of the cornea and conjunctiva. Int Ophthalmol 4:67–76 doi:10.1007/BF00139581
Morris S, Tranos P, Evans S et al (2003) Ocular manifestations of Fabry disease: effect of enzyme replacement therapy. Acta Paediatr 92(Suppl 443):110–115 doi:10.1080/08035320310000492
Funding
The study was supported in part by the DFG (Transregio 37, Micro- und Nanosystems in Medicine - Reconstruction of Biological Functions) and by an internal grant from the University of Rostock (FORUN N 889009).
Author information
Authors and Affiliations
Corresponding author
Additional information
Partly presented during the annual meeting of the German Society of Ophthalmology (DOG) in Berlin 2007.
Competing interests
Andrey Zhivov, MD, and Rudolf F. Guthoff, MD are consultants to Heidelberg Engineering, Heidelberg, Germany. Karen Falke, Armin Büttner MD, Michael Schittkowski MD, Oliver Stachs PhD, Robert Kraak MD, have no financial interests to declare.
Rights and permissions
About this article
Cite this article
Falke, K., Büttner, A., Schittkowski, M. et al. The microstructure of cornea verticillata in Fabry disease and amiodarone-induced keratopathy: a confocal laser-scanning microscopy study. Graefes Arch Clin Exp Ophthalmol 247, 523–534 (2009). https://doi.org/10.1007/s00417-008-0962-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-0962-9