Abstract
Background
Walking dysfunction is common in people with multiple sclerosis (MS). Besides walking speed or endurance, one crucial feature of ambulatory function is the ability to adjust the gait pattern according to walking speed which relies on the integrity of spinal motor centres, their reciprocal connections to supraspinal networks and peripheral sensory input.
Objective
To investigate the capacity of people with MS to modify their gait pattern in response to changes in walking speed.
Methods
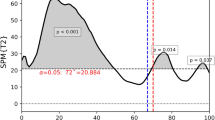
3D gait analysis during free treadmill walking was performed in 35 people with MS and 20 healthy controls. Twelve kinematic parameters ranging from basic spatiotemporal measures to complex indicators of intralimb coordination were assessed at different absolute and relative walking speeds.
Results
Cadence, double-limb support time, trunk movements and especially measures of intralimb coordination demonstrated significantly less speed-dependent modifications in MS than in controls. These limitations were more prominent in subjects with stronger MS-related impairment (worse outcome in clinical walking tests, higher Expanded Disability Status Scale).
Conclusion
The incapacity to modify specific elements of the walking pattern according to walking speed contributes to gait dysfunction in people with MS limiting activities of daily living. Gait modulation may serve as sensitive marker of walking function in MS.
Trial registration
Clinicaltrials.gov, NCT01576354; first posted April 12, 2012.




Similar content being viewed by others
Data availability
Not applicable.
References
Grieve DW, Gear RJ (1966) The relationships between length of stride, step frequency, time of swing and speed of walking for children and adults. Ergonomics 9(5):379–399. https://doi.org/10.1080/00140136608964399
Nilsson J, Thorstensson A, Halbertsma J (1985) Changes in leg movements and muscle activity with speed of locomotion and mode of progression in humans. Acta Physiol Scand 123(4):457–475. https://doi.org/10.1111/j.1748-1716.1985.tb07612.x
Grillner S, Wallen P (1985) Central pattern generators for locomotion, with special reference to vertebrates. Annu Rev Neurosci 8:233–261. https://doi.org/10.1146/annurev.ne.08.030185.001313
Dietz V (2003) Spinal cord pattern generators for locomotion. Clin Neurophysiol 114(8):1379–1389. https://doi.org/10.1016/s1388-2457(03)00120-2
Grillner S, Wallen P, Saitoh K, Kozlov A, Robertson B (2008) Neural bases of goal-directed locomotion in vertebrates–an overview. Brain Res Rev 57(1):2–12. https://doi.org/10.1016/j.brainresrev.2007.06.027
Kister I, Chamot E, Salter AR, Cutter GR, Bacon TE, Herbert J (2013) Disability in multiple sclerosis: a reference for patients and clinicians. Neurology 80(11):1018–1024. https://doi.org/10.1212/WNL.0b013e3182872855
Kelleher KJ, Spence W, Solomonidis S, Apatsidis D (2010) The characterisation of gait patterns of people with multiple sclerosis. Disabil Rehabil 32(15):1242–1250. https://doi.org/10.3109/09638280903464497
Remelius JG, Jones SL, House JD, Busa MA, Averill JL, Sugumaran K, Kent-Braun JA, Van Emmerik RE (2012) Gait impairments in persons with multiple sclerosis across preferred and fixed walking speeds. Arch Phys Med Rehabil 93(9):1637–1642. https://doi.org/10.1016/j.apmr.2012.02.019
Comber L, Galvin R, Coote S (2017) Gait deficits in people with multiple sclerosis: a systematic review and meta-analysis. Gait Post 51:25–35. https://doi.org/10.1016/j.gaitpost.2016.09.026
Filli L, Sutter T, Easthope CS, Killeen T, Meyer C, Reuter K, Lorincz L, Bolliger M, Weller M, Curt A, Straumann D, Linnebank M, Zorner B (2018) Profiling walking dysfunction in multiple sclerosis: characterisation, classification and progression over time. Sci Rep 8(1):4984. https://doi.org/10.1038/s41598-018-22676-0
Pau M, Coghe G, Atzeni C, Corona F, Pilloni G, Marrosu MG, Cocco E, Galli M (2014) Novel characterization of gait impairments in people with multiple sclerosis by means of the gait profile score. J Neurol Sci 345(1–2):159–163. https://doi.org/10.1016/j.jns.2014.07.032
Zorner B, Filli L, Reuter K, Kapitza S, Lorincz L, Sutter T, Weller D, Farkas M, Easthope CS, Czaplinski A, Weller M, Linnebank M (2016) Prolonged-release fampridine in multiple sclerosis: Improved ambulation effected by changes in walking pattern. Mult Scler. https://doi.org/10.1177/1352458515622695
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33(11):1444–1452. https://doi.org/10.1212/wnl.33.11.1444
Goldman MD, Marrie RA, Cohen JA (2008) Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult Scler 14(3):383–390. https://doi.org/10.1177/1352458507082607
Motl RW, Cohen JA, Benedict R, Phillips G, LaRocca N, Hudson LD, Rudick R, Multiple Sclerosis Outcome Assessments C (2017) Validity of the timed 25-foot walk as an ambulatory performance outcome measure for multiple sclerosis. Mult Scler 23(5):704–710. https://doi.org/10.1177/1352458517690823
Meyer C, Killeen T, Easthope CS, Curt A, Bolliger M, Linnebank M, Zorner B, Filli L (2019) Familiarization with treadmill walking: How much is enough? Sci Rep 9(1):5232. https://doi.org/10.1038/s41598-019-41721-0
Zeni JA Jr, Richards JG, Higginson JS (2008) Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Post 27(4):710–714. https://doi.org/10.1016/j.gaitpost.2007.07.007
Awai L, Curt A (2014) Intralimb coordination as a sensitive indicator of motor-control impairment after spinal cord injury. Front Hum Neurosci 8:148. https://doi.org/10.3389/fnhum.2014.00148
Pepin A, Norman KE, Barbeau H (2003) Treadmill walking in incomplete spinal-cord-injured subjects: 1. Adaptation to changes in speed. Spinal Cord 41(5):257–270. https://doi.org/10.1038/sj.sc.3101452
Bohannon RW (1997) Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing 26(1):15–19. https://doi.org/10.1093/ageing/26.1.15
Pepin A, Ladouceur M, Barbeau H (2003) Treadmill walking in incomplete spinal-cord-injured subjects: 2. Factors limiting the maximal speed. Spinal Cord 41(5):271–279. https://doi.org/10.1038/sj.sc.3101453
Zackowski KM, Smith SA, Reich DS, Gordon-Lipkin E, Chodkowski BA, Sambandan DR, Shteyman M, Bastian AJ, van Zijl PC, Calabresi PA (2009) Sensorimotor dysfunction in multiple sclerosis and column-specific magnetization transfer-imaging abnormalities in the spinal cord. Brain 132(Pt 5):1200–1209. https://doi.org/10.1093/brain/awp032
Gass A, Rocca MA, Agosta F, Ciccarelli O, Chard D, Valsasina P, Brooks JC, Bischof A, Eisele P, Kappos L, Barkhof F, Filippi M, Group MS (2015) MRI monitoring of pathological changes in the spinal cord in patients with multiple sclerosis. Lancet Neurol 14(4):443–454. https://doi.org/10.1016/S1474-4422(14)70294-7
Dietz V (2002) Proprioception and locomotor disorders. Nat Rev Neurosci 3(10):781–790. https://doi.org/10.1038/nrn939
Forssberg H, Grillner S, Halbertsma J (1980) The locomotion of the low spinal cat. I. Coordination within a hindlimb. Acta Physiol Scand 108(3):269–281. https://doi.org/10.1111/j.1748-1716.1980.tb06533.x
Barbeau H, Rossignol S (1987) Recovery of locomotion after chronic spinalization in the adult cat. Brain Res 412(1):84–95. https://doi.org/10.1016/0006-8993(87)91442-9
Dietz V, Muller R, Colombo G (2002) Locomotor activity in spinal man: significance of afferent input from joint and load receptors. Brain 125(Pt 12):2626–2634. https://doi.org/10.1093/brain/awf273
Pirko I, Lucchinetti CF, Sriram S, Bakshi R (2007) Gray matter involvement in multiple sclerosis. Neurology 68(9):634–642. https://doi.org/10.1212/01.wnl.0000250267.85698.7a
Calabrese M, Filippi M, Gallo P (2010) Cortical lesions in multiple sclerosis. Nat Rev Neurol 6(8):438–444. https://doi.org/10.1038/nrneurol.2010.93
Gilmore CP, Donaldson I, Bo L, Owens T, Lowe J, Evangelou N (2009) Regional variations in the extent and pattern of grey matter demyelination in multiple sclerosis: a comparison between the cerebral cortex, cerebellar cortex, deep grey matter nuclei and the spinal cord. J Neurol Neurosurg Psychiatry 80(2):182–187. https://doi.org/10.1136/jnnp.2008.148767
Gilmore CP, Geurts JJ, Evangelou N, Bot JC, van Schijndel RA, Pouwels PJ, Barkhof F, Bo L (2009) Spinal cord grey matter lesions in multiple sclerosis detected by post-mortem high field MR imaging. Mult Scler 15(2):180–188. https://doi.org/10.1177/1352458508096876
Dietz V (2001) Gait disorder in spasticity and Parkinson’s disease. Adv Neurol 87:143–154
Mirbagheri MM, Barbeau H, Ladouceur M, Kearney RE (2001) Intrinsic and reflex stiffness in normal and spastic, spinal cord injured subjects. Exp Brain Res 141(4):446–459. https://doi.org/10.1007/s00221-001-0901-z
Pau M, Coghe G, Corona F, Marrosu MG, Cocco E (2015) Effect of spasticity on kinematics of gait and muscular activation in people with multiple sclerosis. J Neurol Sci 358(1–2):339–344. https://doi.org/10.1016/j.jns.2015.09.352
Sheean G, McGuire JR (2009) Spastic hypertonia and movement disorders: pathophysiology, clinical presentation, and quantification. PM R 1(9):827–833. https://doi.org/10.1016/j.pmrj.2009.08.002
Coghe G, Pau M, Corona F, Frau J, Lorefice L, Fenu G, Spinicci G, Mamusa E, Musu L, Massole S, Massa R, Marrosu MG, Cocco E (2015) Walking improvements with nabiximols in patients with multiple sclerosis. J Neurol 262(11):2472–2477. https://doi.org/10.1007/s00415-015-7866-5
Dillmann U, Holzhoffer C, Johann Y, Bechtel S, Graber S, Massing C, Spiegel J, Behnke S, Burmann J, Louis AK (2014) Principal component analysis of gait in Parkinson’s disease: relevance of gait velocity. Gait Post 39(3):882–887. https://doi.org/10.1016/j.gaitpost.2013.11.021
Morris M, Iansek R, McGinley J, Matyas T, Huxham F (2005) Three-dimensional gait biomechanics in Parkinson’s disease: evidence for a centrally mediated amplitude regulation disorder. Movement Disord 20(1):40–50. https://doi.org/10.1002/mds.20278
Acknowledgements
We thank the individuals who participated in this study. The authors are grateful to Tabea Sutter, Sandra Kapitza and Katja Reuter for their assistance with subject recruitment and assessments. This study was supported by grants from the Betty and David Koetser Foundation, the Clinical Research Priority Program (CRPP) “NeuroRehab” of the University of Zurich, the Swiss MS Society, and Biogen.
Funding
This study was supported by grants from the Betty and David Koetser Foundation, the Clinical Research Priority Program (CRPP) “NeuroRehab” of the University of Zurich, the Swiss MS Society, and Biogen.
Author information
Authors and Affiliations
Contributions
DW, LF and BZ planed and designed the study, collected and analysed data, performed statistics, interpreted the data, produced figures, and prepared the manuscript. CM and LL collected and analysed data and CM produced figures. ML, MW, AC and BZ conceived and supervised the study and critically revised the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
CM received a travel grant from Biogen. ML received grants, honoraria or funding from Almirall, Bayer, Biogen, Genzyme, Merck, Novartis, Roche and Teva. MW received research grants from Abbvie, Adastra, Bristol Meyer Squibb (BMS), Dracen, Merck, Sharp & Dohme (MSD), Merck (EMD), Novocure, Piqur and Roche, and honoraria for lectures or advisory board participation or consulting from Abbvie, Basilea, Bristol Meyer Squibb (BMS), Celgene, Merck, Sharp and Dohme (MSD), Merck (EMD), Novocure, Orbus, Roche and Tocagen. BZ received honoraria, travel grants, and funding from Biogen and Roche. The other authors declare that there is no conflict of interest.
Ethics approval
The studies were approved by the Zurich cantonal ethics committee (KEK-2011-0445, KEK-2014-0004) in Switzerland.
Consent to participate
All participants gave written, informed consent.
Consent for publication
All authors read and approved the final manuscript and gave consent for publication.
Rights and permissions
About this article
Cite this article
Weller, D., Filli, L., Meyer, C. et al. Impaired speed-dependent modulation of the gait pattern in multiple sclerosis. J Neurol 267, 2998–3007 (2020). https://doi.org/10.1007/s00415-020-09965-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09965-3