Abstract
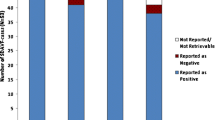
MRI is the primary screening tool for patients with myelopathy. The decision to obtain additional imaging, notably spinal angiography, is generally based on initial MRI findings. This study retrospectively analyzed the yield of initial MRI in a cohort of patients with angiographically confirmed vascular malformations. MRI obtained at symptom onset was available in 115 patients with either high-flow (29 cases) or low-flow (86 cases) vascular malformations. MRI was classified as “positive” when the report mentioned a vascular malformation or “negative” when considered normal or when another diagnosis was suggested. Initial MRI was positive in 61 patients (53.0%), correctly identifying 28 high-flow (96.6%) but only 33 low-flow (38.4%) lesions. Flow voids were noted in 96.6% of the high-flow lesions and 38.4% of the low-flow ones. T2-signal anomalies (77.4%) and parenchymal enhancement (54.5%) were also common in low-flow anomalies. Patients with negative MRI had an average delay of 111 days before angiography and 239 days before therapy; these intervals were 27 and 76 days for those with positive MRIs. In summary, MRI shows a high yield for high-flow vascular malformations, i.e., characterized by prominent flow voids on T2-weighted images, but misdiagnosed over 60% of low-flow lesions. The percentage of correctly identified anomalies matched the percentage of observed flow voids in both groups, indicating over-reliance on this sign for the diagnosis of slow-flow lesions. MRI findings in slow-flow vascular malformation overlap with other conditions, notably transverse myelitis, which was initially misattributed to 40% of the slow-flow lesions in our cohort.


Similar content being viewed by others
References
Rangel-Castilla L, Russin JJ, Zaidi HA, Martinez-Del-Campo E, Park MS, Albuquerque FC, McDougall CG, Nakaji P, Spetzler RF (2014) Contemporary management of spinal AVFs and AVMs: lessons learned from 110 cases. Neurosurg Focus 37(3):E14. doi:10.3171/2014.7.FOCUS14236
Flores BC, Klinger DR, White JA, Batjer HH (2016) Spinal vascular malformations: treatment strategies and outcome. Neurosurg Rev. doi:10.1007/s10143-016-0713-z
Gilbertson JR, Miller GM, Goldman MS, Marsh WR (1995) Spinal dural arteriovenous fistulas: MR and myelographic findings. AJNR Am J Neuroradiol 16(10):2049–2057
Özkan N, Kreitschmann-Andermahr I, Goerike SL, Wrede KH, Kleist B, Stein KP, Gembruch O, Sandalcioglu IE, Wanke I, Sure U (2015) Single center experience with treatment of spinal dural arteriovenous fistulas. Neurosurg Rev 38(4):683–692. doi:10.1007/s10143-015-0645-z
Lanzino G, D’Urso PI, Kallmes DF, Cloft HJ (2012) Onyx embolization of extradural spinal arteriovenous malformations with intradural venous drainage. Neurosurgery 70(2):329–333. doi:10.1227/NEU.0b013e318230929e
Merland JJ, Riche MC, Chiras J (1980) Intraspinal extramedullary arteriovenous fistulae draining into the medullary veins. J Neuroradiol 7(4):271–320
Thiex R, Mulliken JB, Revencu N, Boon LM, Burrows PE, Cordisco M, Dwight Y, Smith ER, Vikkula M, Orbach DB (2010) A novel association between RASA1 mutations and spinal arteriovenous anomalies. AJNR Am J Neuroradiol 31(4):775–779. doi:10.3174/ajnr.A1907
Saraf-Lavi E, Bowen BC, Quencer RM, Sklar EM, Holz A, Falcone S, Latchaw RE, Duncan R, Wakhloo A (2002) Detection of spinal dural arteriovenous fistulae with MR imaging and contrast-enhanced MR angiography: sensitivity, specificity, and prediction of vertebral level. AJNR Am J Neuroradiol 23(5):858–867
Koch C (2006) Spinal dural arteriovenous fistula. Curr Opin Neurol 19(1):69–75
Saladino A, Atkinson JL, Rabinstein AA, Piepgras DG, Marsh WR, Krauss WE, Kaufmann TJ, Lanzino G (2010) Surgical treatment of spinal dural arteriovenous fistulae: a consecutive series of 154 patients. Neurosurgery 67(5):1350–1357. doi:10.1227/NEU.0b013e3181ef2821 (discussion 1357–1358)
Eckart Sorte D, Obrzut M, Wyse E, Gailloud P (2016) Normal venous phase documented during angiography in patients with spinal vascular malformations: incidence and clinical implications. AJNR Am J Neuroradiol 37(3):565–571. doi:10.3174/ajnr.A4601
Mirbagheri S, Eckart Sorte D, Zamora CA, Mossa-Basha M, Newsome SD, Izbudak I (2016) Evaluation and management of longitudinally extensive transverse myelitis: a guide for radiologists. Clin Radiol 71(10):960–971. doi:10.1016/j.crad.2016.05.020
Choi KH, Lee KS, Chung SO, Park JM, Kim YJ, Kim HS, Shinn KS (1996) Idiopathic transverse myelitis: MR characteristics. AJNR Am J Neuroradiol 17(6):1151–1160
Kumral E, Polat F, Güllüoglu H, Uzunköprü C, Tuncel R, Alpaydin S (2011) Spinal ischaemic stroke: clinical and radiological findings and short-term outcome. Eur J Neurol 18(2):232–239. doi:10.1111/j.1468-1331.2010.02994.x
Cosnard G (2012) Tips and traps in spinal cord pathology. Diagn Interv Imaging 93(12):975–984. doi:10.1016/j.diii.2012.08.003
Jellema K, Canta LR, Tijssen CC, van Rooij WJ, Koudstaal PJ, van Gijn J (2003) Spinal dural arteriovenous fistulas: clinical features in 80 patients. J Neurol Neurosurg Psychiatry 74(10):1438–1440
Rosenblum B, Oldfield EH, Doppman JL, Di Chiro G (1987) Spinal arteriovenous malformations: a comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg 67(6):795–802. doi:10.3171/jns.1987.67.6.0795
Symon L, Kuyama H, Kendall B (1984) Dural arteriovenous malformations of the spine. Clinical features and surgical results in 55 cases. J Neurosurg 60(2):238–247. doi:10.3171/jns.1984.60.2.0238
Transverse Myelitis Consortium Working G (2002) Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology 59(4):499–505
Harzheim M, Schlegel U, Urbach H, Klockgether T, Schmidt S (2004) Discriminatory features of acute transverse myelitis: a retrospective analysis of 45 patients. J Neurol Sci 217(2):217–223
Amarouche M, Hart JL, Siddiqui A, Hampton T, Walsh DC (2015) Time-resolved contrast-enhanced MR angiography of spinal vascular malformations. AJNR Am J Neuroradiol 36(2):417–422. doi:10.3174/ajnr.A4164
Unsrisong K, Taphey S, Oranratanachai K (2016) Spinal arteriovenous shunts: accuracy of shunt detection, localization, and subtype discrimination using spinal magnetic resonance angiography and manual contrast injection using a syringe. J Neurosurg Spine 24(4):664–670. doi:10.3171/2015.7.SPINE15319
Lindenholz A, TerBrugge KG, van Dijk JM, Farb RI (2014) The accuracy and utility of contrast-enhanced MR angiography for localization of spinal dural arteriovenous fistulas: the Toronto experience. Eur Radiol 24(11):2885–2894. doi:10.1007/s00330-014-3307-6
Chen J, Gailloud P (2011) Safety of spinal angiography: Complication rate analysis in 302 diagnostic angiograms. Neurology 77(13):1235–1240. doi:10.1212/WNL.0b013e3182302068
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
El Mekabaty, A., Pardo, C.A. & Gailloud, P. The yield of initial conventional MRI in 115 cases of angiographically confirmed spinal vascular malformations. J Neurol 264, 733–739 (2017). https://doi.org/10.1007/s00415-017-8419-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8419-x