Abstract
Purpose
Our objective was to investigate the combinatorial effect of maternal age and second-trimester maternal lipid profiles for pregnancy complications.
Methods
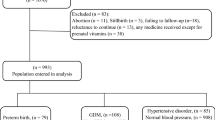
With 1:4 matching, this retrospective study selected 499 advanced maternal age women and 1996 younger controls. Logistic regression analysis was used to estimate the correlation between second-trimester lipid profiles [total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C)] and pregnancy complications [gestational diabetes mellitus (GDM), pregnancy-induced hypertension syndrome (PIH), preterm labor (PTL), and macrosomia]. Optimal cutoff points were determined by ROC curve analysis.
Results
In women aged 20–34 years, TG are a risk factor for PIH (OR 1.54, 95% CI 1.16–2.04) and PTL (OR 1.34, 95% CI 1.04–1.72). LDL-C was positively associated with macrosomia (OR 1.25, 95% CI 1.04–1.50), while HDL-C was negatively associated with PIH (OR 0.45, 95% CI 0.21–0.93). The optimal cutoff points for TG predicting PIH and PTL were separately ≥ 2.135 and 2.305 mmol/L. The optimal cutoff point for HDL-C identifying PIH was ≤ 1.995 mmol/L and for LDL-C identifying macrosomia was ≥ 3.425 mmol/L. As for advanced maternal age, only TG was an independent risk factor for PIH (OR 1.60, 95% CI 1.01–2.54), and its optimal cutoff point was ≥ 2.375 mmol/L.
Conclusions
Second-trimester lipid profiles might predict pregnancy complications varied by maternal age. This suggested that individualized prenatal care strategies should be established for women with advanced and normal maternal age to prevent pregnancy complications.

Similar content being viewed by others
References
Goisis A, Remes H, Barclay K, Martikainen P, Myrskylä M (2017) Advanced maternal age and the risk of low birth weight and preterm delivery: a within-family analysis using finnish population registers. Am J Epidemiol 186(11):1219
Matthews TJ, Hamilton BE (2014) First births to older women continue to rise. NCHS Data Brief 152(152):1–8
Kenny LC, Tina L, Roseanne MN, O’Neill SM, Tracey M, Khashan AS (2013) Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PLoS One 8(2):e56583
Hsieh TT, Liou JD, Hsu JJ, Lo LM, Chen SF, Hung TH (2010) Advanced maternal age and adverse perinatal outcomes in an Asian population. Eur J Obstet Gynecol Reprod Biol 148(1):21–26
Laopaiboon M, Lumbiganon P, Intarut N, Mori R, Ganchimeg T, Vogel JP, Souza JP, Gülmezoglu AM (2014) Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG 121(s1):49–56
Lean SC, Derricott H, Jones RL, Aep H (2017) Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One 12(10):e0186287
Ogawa K, Urayama KY, Tanigaki S, Sago H, Sato S, Saito S, Morisaki N (2017) Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC Pregnancy Childbirth 17(1):349
Herrera E (2002) Lipid metabolism in pregnancy and its consequences in the fetus and newborn. Endocrine 19(1):43–55
Catov JM, Bodnar LM, Kip KE, Hubel C, Ness RB, Harger G, Roberts JM (2007) Early pregnancy lipid concentrations and spontaneous preterm birth. Am J Obstet Gynecol 197(6):1–7
Vrijkotte TG, Krukziener N, Hutten BA, Vollebregt KC, Van EM, Twickler MB (2012) Maternal lipid profile during early pregnancy and pregnancy complications and outcomes: the ABCD study. J Clin Endocrinol Metab 97(11):3917
Zheng W, Huang W, Zhang L, Tian Z, Wang T, Zhang T, Zhang Z, Zhang W, Li G (2018) Changes in serum lipid levels during pregnancy and association with neonatal outcomes: a large cohort study. Reprod Sci 25:1406–1412
Diabetes IAO (2015) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(7):e97
Brown MA, Lindheimer MD, Swiet M, Assche A, Moutquin JM (2001) The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Clin Exp Hypertens B 20(1):ix–xiv
Choo V (2002) WHO reassesses appropriate body-mass index for Asian populations. Lancet 360(9328):235
Rasmussen KM, Yaktine AK, Rasmussen KM, Yaktine AK (2009) Weight gain during pregnancy: reexamining the guidelines. National Academies Press, Washington
Deng SQ, Wang ZL, Chen HT (2015) Analysis of the characteristics of serum lipids in pregnant women of second trimester at different ages. Chin J Obstet Gynecol 12:1129–1132
Herrera E, Amusquivar E, Lópezsoldado I, Ortega H (2006) Maternal lipid metabolism and placental lipid transfer. Horm Res 65(1):59–64
Khalil A, Syngelaki A, Maiz N, Zinevich Y, Nicolaides KH (2013) Maternal age and adverse pregnancy outcome: a cohort study. Ultrasound Obstet Gynecol 42(6):634–643
Ananth CV, Keyes KM, Wapner RJ (2013) Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ 347:6564
The Preterm Labor Syndrome: Biochemical, Cytologic, Immunologic, Pathologic, Microbiologic, and Clinical Evidence That Preterm Labor Is a Heterogeneous Disease (1993). Am J Obstet Gynecol 168 (1Part2):288
Catov JM, Newman AB, Suttontyrrell K, Harris TB, Tylavsky F, Visser M, Ayonayon HN, Ness RB (2008) Parity and cardiovascular disease risk among older women: how do pregnancy complications mediate the association? Ann Epidemiol 18(12):873–879
Enquobahrie DA, Williams MA, Butler CL, Frederick IO, Miller RS, Luthy DA (2004) Maternal plasma lipid concentrations in early pregnancy and risk of preeclampsia. Am J Hypertens 17(7):574
Shen H, Liu X, Chen Y, He B, Cheng W (2016) Associations of lipid levels during gestation with hypertensive disorders of pregnancy and gestational diabetes mellitus: a prospective longitudinal cohort study. Bmj Open 6(12):e013509
Mudd LM, Holzman CB, Catov JM, Senagore PK, Evans RW (2012) Maternal lipids at mid-pregnancy and the risk of preterm delivery. Acta Obstet Gynecol Scand 91(6):726–735
Catov JM, Bodnar LM, Ness RB, Barron SJ, Roberts JM (2007) Inflammation and dyslipidemia related to risk of spontaneous preterm birth. Am J Epidemiol 166(11):1312
Jin WY, Lin SL, Hou RL, Chen XY, Han T, Yan J, Li T, Zhu ZW, Zhao ZY (2016) Associations between maternal lipid profile and pregnancy complications and perinatal outcomes: a population-based study from China. BMC Pregnancy Childbirth 16(1):60
Bowers K, Laughon SK, Kiely M, Brite J, Chen Z, Zhang C (2013) Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: variations by race/ethnicity. Diabetologia 56(6):1263–1271
He XJ, Qin FY, Hu CL, Zhu M, Tian CQ, Li L (2015) Is gestational diabetes mellitus an independent risk factor for macrosomia: a meta-analysis? Arch Gynecol Obstet 291(4):729–735
Acknowledgements
This study was supported by the Foundation of Key Supporting Discipline of Zhejiang Province, Zhejiang Provincial & Ministry of Health Research Fund for Medical Sciences (WKJ-ZJ-1722), Key Project of Science and Technology Department of Zhejiang Province (2018C03010). We also thank Professor Peixin Yang from University of Maryland School of Medicine for guidance in data analysis.
Author information
Authors and Affiliations
Contributions
QW and LXZ: project development, data collection, data analysis, data interpretation, and manuscript writing. LH, YL and LC: data analysis and manuscript revision. ZXL, MLZ, HX, YMZ and FW: data collection and manuscript revision. DQC: project development, data interpretation, and manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no duality of interest associated with this manuscript.
Informed consent
In this study, we confirm that patient privacy was not compromised, which was approved by the hospital’s ethics committee. And specific informed consent for inclusion was waived because of using anonymized patient records.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, Q., Zhang, L., Huang, L. et al. Second-trimester maternal lipid profiles predict pregnancy complications in an age-dependent manner. Arch Gynecol Obstet 299, 1253–1260 (2019). https://doi.org/10.1007/s00404-019-05094-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05094-z