Abstract
Background and objectives
To compare effectiveness and safety of dinoprostone, misoprostol and Cook’s balloon as labour-inducing agents in women with intrauterine growth restriction (IUGR) at term.
Methods
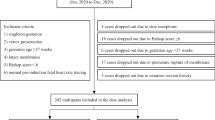
Retrospective cohort chart review of women diagnosed with foetal growth restriction at term in Reina Sofia Hospital, Cordoba, Spain from January 2014 to December 2015. Registration of baseline characteristics and method of induction was made. The main outcome was time from induction to delivery. Obstetric and perinatal outcomes were also collected.
Results
A total of 99 women were diagnosed with IUGR in the mentioned period. Of them, 21 women were induced with dinoprostone [dinoprostone group (DG)], 20 with misoprostol (MG) and in 58 with Cook’s balloon (CG). Groups were homogeneous regarding pre-induction Bishop score and parity. The CG required more time (24.36 vs. 19.23 h; p = 0.02) and more oxytocin dose for conduction of labour from induction to delivery (6.75 vs. 1.24 mUI; p < 0.01) than DG. Moreover, the CG also needed more oxytocin than MG, 6.75 vs. 2.37 mUI (p < 0.001). Caesarean rate was 5, 14.9 and 17.3% in MG, DG and CG, respectively. No differences were observed in rates of uterine tachysystole, non-reassuring foetal status and neonatal adverse events.
Interpretation and conclusions
Prostaglandins were more effective than Cook’s balloon to induce labour and achieve vaginal birth in this sample of women with IUGR at term, with a similar safety profile.
Similar content being viewed by others
References
Lawani OL, Onyebuchi AK, Iyoke CA, Okafo CN, Ajah LO (2014) Obstetric outcome and significance of labour induction in a health resource poor setting. Obstet Gynecol Int 2014:419621
Mozurkewich E, Chilimigras J, Koepke E, Keeton K, King VJ (2009) Indications for induction of labour: a best-evidence review. BJOG 116(5):626–636
Parkes I, Kabiri D, Hants Y, Ezra Y (2016) The indication for induction of labor impacts the risk of cesarean delivery. J Matern Foetal Neonatal Med 29(2):224–228
Rijal P (2014) Identification of risk factors for cesarean delivery following induction of labour. J Nepal Health Res Counc 12(27):73–77
Kelly AJ, Malik S, Smith L, Kavanagh J, Thomas J (2009) Vaginal prostaglandin (PGE2 and PGF2a) for induction of labour at term. Cochrane Database Syst Rev 4:CD003101
Keirse MJ (2006) Natural prostaglandins for induction of labor and preinduction cervical ripening. Clin Obstet Gynecol 49(3):609–626
Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW, Irion O, Boulvain M (2012) Mechanical methods for induction of labour. Cochrane Database Syst Rev 3:CD001233
Pevzner L, Rayburn WF, Rummey P, Wing DA (2009) Factors predicting successful labor induction with dinoprostone and misoprostol vaginal inserts. Obstet Gynecol 114(2 Pt 1):261–267
Resnik R (2002) Intrauterine growth restriction. Obstet Gynecol 99(3):490–496
Rhinehart-Ventura J, Eppes C, Sangi-Haghpeykar H, Davidson C (2014) Evaluation of outcomes after implementation of an induction-of-labor protocol. Am J Obstet Gynecol 211(3):301.e1–301.e7
Crane JM (2006) Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol 49(3):573–584
Liu A, Lv J, Hu Y, Lang J, Ma L, Chen W (2014) Efficacy and safety of intravaginal misoprostol versus intracervical dinoprostone for labor induction at term: a systematic review and meta-analysis. J Obstet Gynaecol Res 40(4):897–906
Du C, Liu Y, Ding H, Zhang R, Tan J (2015) Double-balloon catheter vs. dinoprostone vaginal insert for induction of labor with an unfavorable cervix. Arch Gynecol Obstet 291(6):1221–1227
Bishop EH (1964) Pelvic scoring for elective induction. Obstet Gynecol 24:266–268
Chavakula PR, Benjamin SJ, Abraham A, Londhe V, Jeyaseelan V, Mathews JE (2015) Misoprostol versus Foley catheter insertion for induction of labor in pregnancies affected by foetal growth restriction. Int J Gynaecol Obstet 129(2):152–155
Hofmeyr GJ, Gulmezoglu AM, Alfirevic Z (1999) Misoprostol for induction of labour: a systematic review. Br J Obstet Gynaecol 106(8):798–803
Goldberg AB, Greenberg MB, Darney PD (2001) Misoprostol and pregnancy. N Engl J Med 344(1):38–47
Culver J, Strauss RA, Brody S, Dorman K, Timlin S, McMahon MJ (2004) Randomized trial comparing vaginal misoprostol versus Foley catheter with concurrent oxytocin for labor induction in nulliparous women. Am J Perinatol 21(3):139–146
Ben-Haroush A, Yogev Y, Glickman H, Kaplan B, Hod M, Bar J (2004) Mode of delivery in pregnancies with suspected foetal growth restriction following induction of labor with vaginal prostaglandin E2. Acta Obstet Gynecol Scand 83(1):52–57
Fox NS, Saltzman DH, Roman AS, Klauser CK, Moshier E, Rebarber A (2011) Intravaginal misoprostol versus Foley catheter for labour induction: a meta-analysis. BJOG 118(6):647–654
He Y, Hu J, Zhang X, Huang H, Chen Q (2014) Clinical analysis of double-balloon catheter for cervical ripening in 66 cases. Zhonghua Fu Chan Ke Za Zhi 49(10):741–745
Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP (2001) Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 345(1):3–8
De Bonrostro Torralba C, Tejero Cabrejas EL, Marti Gamboa S, Lapresta Moros M, Campillos Maz JM, Castán Mateo S (2017) Double-balloon catheter for induction of labour in women with a previous cesarean section could it be the best choice? Arch Gynecol Obstet 295(5):1135–1143
Kehl S, Weiss C, Wamsler M et al (2016) Double-balloon catheter and sequential vaginal prostaglandin E2 versus vaginal prostaglandin E2 alone for induction of labor after previous cesarean section. Arch Gynecol Obstet 293(4):757–765
WHO (2011) WHO Recommendations for induction of labour. World Health Organization, Geneva. Available from: http://www.ncbi.nlm.nih.gov/books/NBK131963/. Accessed 31 July 2017
Duro-Gómez J, Garrido-Oyarzún MF, Rodríguez-Marín AB, de la Torre González AJ, Arjona-Berral JE, Castelo-Branco C (2017) What can we do to reduce the associated cost in induction of labour of intrauterine growth restriction foetuses at term? A cost-analysis study. Arch Gynecol Obstet. doi:10.1007/s00404-017-4458-x
Author information
Authors and Affiliations
Contributions
JDG: project development, data collection and analysis, and manuscript writing. MFGO: data analysis and manuscript editing. ABRM: data collection and management. AJTG: data collection and management. JEAB: data management and analysis, and manuscript editing. CC-B: data analysis, manuscript writing and editing
Corresponding author
Ethics declarations
Conflict of interest
We, the authors, declare that we have no conflict of interest.
Informed consent
This survey was conducted as an open prospective quasi-experimental cohort study and was approved by the institutional review board of the Reina Sofia Hospital (Córdoba, Spain. Reference 246-26/11/2015). All of the procedures were in accordance with the Helsinki Declaration of 1975.
Rights and permissions
About this article
Cite this article
Duro-Gómez, J., Garrido-Oyarzún, M.F., Rodríguez-Marín, A.B. et al. Efficacy and safety of misoprostol, dinoprostone and Cook’s balloon for labour induction in women with foetal growth restriction at term. Arch Gynecol Obstet 296, 777–781 (2017). https://doi.org/10.1007/s00404-017-4492-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4492-8