Abstract
Purpose
The aim of this study was to evaluate possible associations of genetic polymorphisms predisposing to cardiovascular disease with the development and/or the severity of preeclampsia.
Methods
A two hospital-based prospective case–control study was performed in Germany and Ghana. 470 blood samples of 250 Caucasian and 220 black African have been genotyped by pyrosequencing and fragment length analysis. We evaluated the distribution of the epoxide hydrolase 1 (EPHX1) polymorphism on exon 3, the endothelial nitric oxide synthase (eNOS) polymorphisms on exon 7 and on intron 4, the angiotensinogen polymorphism on exon 2 and the estrogen receptor 1 polymorphism in intron 1.
Results
74 Caucasian and 84 African were classified as preeclampsia with 27 Caucasian developing a hemolysis, elevated liver enzymes and low platelets (HELLP) syndrome and 17 African women experiencing eclampsia. Multivariate logistic regression analysis adjusting for ethnicity, age and parity revealed for carriers of eNOSI4 VNTR4a a 1.7-fold increased (95 % CI 1.10–2.711, p = 0.016) risk to develop preeclampsia and a 3.6-fold increase for carriers of the EPHX1 113Tyr (95 % CI 1.366–8.750, p = 0.009) to develop severest preeclampsia.
Conclusion
Our finding of eNOSI4 polymorphism predisposing to preeclampsia independently of ethnicity, age and parity supports the concept of NO being involved in the endothelial disorder preeclampsia. Since EPHX1 is highly expressed in the liver, can interact with various signaling pathways and is involved in central nervous system disorders, the association of EPHX1 polymorphism with the HELLP syndrome and eclampsia may hint to EPHX being a further key player in the pathogenesis of preeclampsia.
Similar content being viewed by others
Introduction
Preeclampsia, the leading cause of maternal and fetal morbidity, affects 3–8 % of all pregnancies worldwide, with an incidence of 3 % in the western Caucasian population and up to 10 % in black African. The symptoms of preeclampsia are all features of disturbed endothelial barrier function, including edema, hypertension with elevated brain pressure, liver swelling and alteration of the glomerular filtration leading to enhanced protein loss. The maternal syndrome potentially progresses to the life-threatening condition of hemolysis, elevated liver enzymes and low platelets (HELLP) syndrome, disseminated intravascular coagulation, acute renal failure, pulmonary edema or the development of eclampsia, associated with generalized seizures, stroke, intracerebral bleeding and death [1]. Accordingly preeclampsia is categorized as severe in the presence of a HELLP syndrome or eclampsia. The HELLP syndrome complicates 10–20 % of cases of preeclampsia [2]. Eclampsia affects 1–2 % of the cases but has a tenfold higher incidence in black African women with preeclampsia [1]. Severe preeclampsia may run a fulminating course, necessitating immediate, frequently premature, delivery of the child. In contrast, in mild cases the disorder progresses more slowly, allowing time to control maternal blood pressure and the delivery of the child at appropriate gestational age.
Although the symptoms of preeclampsia resolve after delivery [3], the maternal vascular dysfunction persists and mothers suffering from preeclampsia during pregnancy have a significantly increased risk for future cardiovascular disease [4]. Furthermore, mothers with endothelial dysfunction prior to pregnancy (e.g. hypertension, lupus erythematodes, antiphospholipid antibody syndrome) are at high risk to develop preeclampsia during pregnancy [4–6].
Considering the central role of endothelial dysfunction in preeclampsia and the association of preeclampsia to maternal endothelial disease the maternal endothelium appears to be central in the pathophysiology of preeclampsia. The current hypothesis on the etiology of preeclampsia considers a two-stage model of the disease proposing a placental disorder resulting in the release of activating factor(s) into the maternal circulation leading to the manifestation of the multi systemic syndrome [7] where constitutional factors of the maternal endothelium determine the course of the disease [8].
It has been recognized for many years that preeclampsia has a familial component and the identification of susceptibility genes is one of a number of strategies designed to elucidate the underlying pathogenetic mechanisms [9]. Accepting preeclampsia to be a syndrome of endothelial disorder, genetic studies concentrated on the evaluation of gene polymorphism involved in impaired endothelial dysfunction associated with increased risk for cardiovascular disease. However, a decade of genetic molecular research has failed to identify a single susceptibility gene for preeclampsia. Interpretation of genetic studies on preeclampsia is impaired by differences in definition of the disease, size of study population, diverse ethnicity between studies and ethnic mixing within studies [9].
The aim of our study was to investigate the association of preeclampsia or severe preeclampsia with five polymorphisms linked to impaired vascular health in a group of solely white Caucasian and solely black African women. We hypothesized that maternal genetic endothelial susceptibility is critical for the severity of the course of the disease rather than for the onset of preeclampsia. Consequently, our goal was to define a susceptibility gene for the most severe courses of the disease, defined by the development of HELLP syndrome or eclampsia. We investigated the prevalence of the epoxide hydrolase 1 (EPHX1) polymorphism on exon 3 (codon 113, CAC/TAC, Tyr113His, rs1051740), the endothelial nitric oxide synthase (eNOS) polymorphisms on exon 7 (eNOSE7) (base 894 G/T, codon 298, Glu298Asp, rs1799983) and on intron 4 (eNOSI4) [a 27-bp repeat polymorphism, resulting in variable number of tandem repeats (VNTR): 4a/4b], the angiotensinogen (AGT) polymorphism on exon 2 (codon 235, ATG/ACG, Met235Thr, rs699) and the estrogen receptor 1 (ESR1) polymorphism in intron 1 (-401 T/C, rs2234693, pvull, PP).
Patients and methods
Patients
A two hospital-based prospective case–control study was performed at the Department of Obstetrics and Gynecology at University Hospital in Ulm, Germany, and the Department of Obstetrics and Gynecology at the Komfo Anokye Teaching Hospital, Kwame Nkrumah University of Science and Technology in Kumasi, Ghana. Ethical approval was obtained from the ethical committee of the University of Ulm (19/08) as well as from the local ethical committee in Kumasi. Informed consent was obtained from all participating women. In accordance with the American College of Obstetrics and Gynecology criteria, pregnancies were diagnosed as preeclamptic if blood pressure was ≥140/90 mmHg and there was ≥2+ proteinuria by dipstick determination on two occasions [10]. A HELLP-syndrome was diagnosed in cases with low platelet counts (less than 100,000/μl), elevated liver enzymes (AST and ALT) and positive hemolysis markers (LDH elevation and declining haptoglobin). Eclampsia was diagnosed if eclamptic convulsions occurred. In control subject pregnancies remained normotensive and non-proteinuric. Patients were enrolled as they were admitted to the hospital and agreed to participate in the study. Women with uncomplicated term pregnancies were consecutively recruited during the same time period as control group.
Genotyping
Peripheral blood was taken upon informed consent and genomic DNA was isolated using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany). Pyrosequencing was used for genotyping the polymorphisms of the genes EPHX1, ESR1, eNOS and AGT. The VNTR polymorphism in intron 4 of the eNOS gene was determined by amplified fragment length analysis as described previously [11, 12]. The PCR conditions and the used primers are shown in Table 1.
Data analysis
Distributions of each polymorphic genotype in control and PE group are described by absolute and relative frequencies, and Fisher’s exact test was applied to compare the occurrence of each polymorphism in both groups. The values for clinical parameters are expressed as mean ± standard deviation. Binary logistic regression models were fitted to estimate adjusted odds ratios (OR) with 95 % confidence intervals as measures of association between polymorphisms and preeclampsia, adjusted for ethnicity, age and parity. The null hypothesis of OR = 1 was tested by the Wald Chi-square statistic. A p value <0.05 was considered to be statistically significant. Statistical analysis was performed with SPSS 19.0 (SPSS Inc., 2010. Chicago, IL).
Results
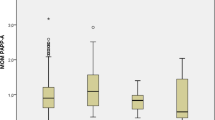
During the study period between 2000 and 2004 blood samples and clinical data of 81 Caucasian patients with preeclampsia and 188 Caucasian normotensive controls could be collected in the University Hospital of Ulm, Germany. In 2001, blood samples and clinical data of 95 black African preeclamptic and 146 black African normotensive control patients could be collected at the Obstetric Department of the Komfo Anokye Teaching Hospital, Kwame Nkrumah University of Science and Technology in Kumasi, Ghana. After exclusion of multiple pregnancies and cases with incomplete data-sets, 470 samples of 250 Caucasian and 220 black African have been genotyped. Of the 250 Caucasian, 74 were classified as preeclampsia, with 27 developing a HELLP-syndrome being categorized as severe preeclampsia. Of the 220 Black African 84 suffered preeclampsia, with 17 classified severe preeclampsia by developing eclampsia (Fig. 1). The clinical and main pregnancy outcome data are shown in Table 2.
Genotype frequencies
The distribution of each polymorphic variant is shown in Table 3. The different genotypes of eNOSI4 (4a4a, 4a4b, 4b4b) are significantly diverse distributed between preeclamptic and control patients in the entire study population (p = 0.009) and in the Caucasian collective (p = 0.015), but not in the African collective (p = 0.435). There was no further significant difference of genotype frequency in controls compared with preeclamptic patients or between patients suffering from severe or mild preeclampsia.
Multivariate logistic regression analysis
Ethnicity, age and parity are considered to be covariates, modifying the risk to develop preeclampsia. Thus we performed a multivariate logistic regression analysis adjusting for ethnicity, age and parity. Results are shown in Table 4. Under the assumption of the dominant model of heredity eNOSI4 4a polymorphism is significantly related to increased risk of developing preeclampsia (p = 0.016): Carriers of the 4a allele have a 1.7-fold increased risk to develop the disease (OR = 1.729, CI 1.10–2.71). The multivariate analysis assuming the recessive model revealed no significant association of polymorphisms and preeclampsia.
Furthermore, based on the hypothesis that constitution of the maternal endothelial is related to the susceptibility and thus severity of the disease, we performed multivariate logistic regression analysis to test the relation of the investigated polymorphisms with the severe course of the disease. Under assumption of the recessive model of heredity the EPHX1 113Tyr polymorphism is significantly related to a 3.5-fold increased risk of developing severe course of the disease in preeclampsia cases (OR = 3.457, CI 1.36–8.75, p = 0.009) Table 5.
Discussion
Postulating a common underlying endothelial susceptibility leading to cardiovascular disease and preeclampsia, this study investigated the prevalence of five polymorphisms known to be associated with cardiovascular disease in pregnant patients suffering from preeclampsia. Indeed, our results show a significant association of the eNOSI4 (VNTR) 4a polymorphism with the development of preeclampsia under the assumption of a dominant model of heredity. Furthermore, the EPHX1 113Tyr polymorphism, under the assumption of a recessive model of heredity, revealed a strong association with the severe course of preeclampsia, eclampsia and the HELLP-syndrome. These data strongly support the concept that the genetic background of the maternal endothelium does predispose to the development of preeclampsia in pregnancy and, furthermore, determines the severity of the disease.
Studies investigating the genetic background in preeclampsia have revealed inconsistent results so far. Consequently, a meta-analysis published in 2007 could not reveal one single polymorphism to have a major effect on the risk to develop preeclampsia [13]. In particular, ethnic diversity between the different study populations and, in part, within the individual studies has been made accountable for the inconclusiveness of these results [13]. Thus, our results reflecting parallel investigation of a large cohort of solely Caucasian and solely African women are especially eligible, as the performed multivariate regression analysis accounts for ethnicity.
In the normal adaptive mechanism of pregnancy, vascular resistance and blood pressure decrease and plasma volume increases under the influence angiotensinogen. In women with preeclampsia vascular resistance remains high and refractivity to pressor effects fail to develop. The function-perturbing polymorphisms of angiotensinogen AGT Met235Thr has been found to be associated with the development of hypertension [14, 15]. A recently published meta-analysis of studies investigating the association of the of AGT Met235Thr polymorphism with preeclampsia summary OR demonstrated that carriers of the polymorphism have an increased risk of developing preeclampsia [13]. However, results between studies were conflicting. After the first report of positive association on US Utah Caucasians and Japanese, the following studies performed in Australians and Chinese, US Hispanic, Koreans (twice), in Zulu South African and Colored South African did not confirm the association. New studies on Caucasians (UK, Austrian, Romanian and Greeks) and Japanese preeclamptic women showed contradictory results (summarized in [13]). Thus, ethnicity of the study population clearly persuades the results. Correspondingly, high differences in allele frequencies for 235Thr as 0.35–0.5 in Caucasian and as high as 0.87 in some non-Caucasian populations have already been shown [16]. Consistently, in our study the allele frequency for the 235Thr variant of the AGT was 0.57 for the Caucasian and 0.92 in the African. The allele frequencies did not differ between preeclamptic and control patients of neither ethnic group, and an increased risk of carriers of AGT 235Thr to develop preeclampsia could not be confirmed by our data.
Estrogen and its receptors are involved in the regulation of vascular function. Estrogen receptor α is expressed on endothelial cells, serving as a transcription factor upon estrogen binding and is linked to growth factor-induced signaling in endothelial cells [17]. Polymorphisms in the estrogen receptor alpha (ESR1) gene have been shown to be associated with cardiovascular disease and high blood pressure [18, 19]. The so-called ESR1 PvuII polymorphism in intron 1, exchanging 397T to 397C has been reported to result in the formation of a B-myb transcription factor binding site and functions as an intragenic enhancer, probably increasing estrogen receptor expression [20]. Increased estrogen receptor expression would subsequently lead to increased susceptibility of endothelial cells to growth factor-mediated activation [17]. The association of the ESR1 PvuII polymorphism with preeclampsia has been studied before. In a Caucasian study group of 119 preeclamptic women and 103 controls the authors showed an association of the 397T allele with preeclampsia [21]. However, Zhang et al. [22] could not confirm any association in a Chinese study group of 204 preeclamptic women and 236 controls. In agreement with the latter, our results could not show an association of the ESR1 PvuII polymorphism with preeclampsia.
Nitric oxide (NO) produced by eNOS has an important function in vascular control, especially vasodilatation [23]. When eNOS is activated by either chemical (acetylcholine and bradikinin) or mechanical stimulus (shear stress), l-arginine metabolism is raised to form l-citrulline and NO within the endothelial cell and vasodilatation occurs [23, 24]. Low NO concentration has been strongly associated with hypertension [25]. NO also influences the hemodynamic of pregnancy by increasing systemic arteriolar vasodilatation and attenuating vasopressor response [26].
Three polymorphisms of the eNOS gene have been reported. A point mutation of thymine (T) to cytosine (C) at nucleotide 786 (T786C) (rs2070744) results in significantly decreased eNOS gene promoter activity. However, lowering of NO-serum concentration in carriers could not be confirmed [27]. Although there is a positive correlation between T786C polymorphism and various cardiovascular diseases, a correlation to hypertension or hypertensive pregnancy disorders could not be confirmed [13, 28]. Hence this polymorphism was not considered in this study. Another point mutation on nucleotide 894 exchanging guanine (G) to thymine (T) leads to the substitution of glutamate (Glu) by aspartate (Asp) at amino acid position 298, the so-called Glu298Asp polymorphism (rs1799983). The 298Asp variant is associated with diminished eNOS activity and NO production [29] and has been implicated in the development of several vascular disorders in which NO bioactivity is reduced. These include essential hypertension, myocardial infarction, angiographic coronary artery disease and coronary spasm [30–32]. Furthermore, association of the 298Asp with preeclampsia has been shown [33, 34]. However, results of these studies have been controversial and the recent meta-analysis of Medica et al. [13] could not confirm significance of association. Again ethnic diversity in study populations and differing diagnostic criteria may account for these inconsistent results. In our study, clearly accounting for ethnicity, we failed to confirm any relation of the Glu298Asp polymorphism with elevated risk to develop preeclampsia or to suffer the more severe courses of the disease. Furthermore, our data revealed a low prevalence of the 298Asp allele (q = 0.08) in the African women studied compared with the white Caucasian women (q = 0.23), as has been described before [35]. Since black African in general show higher incidence of preeclampsia, the remarkably low prevalence of the polymorphism controvert the concept of increased susceptibility to preeclampsia in the presence of the polymorphism. Consistently, we did not find the 298Asp polymorphism to be associated with preeclampsia or severe preeclampsia.
The second investigated polymorphism of the eNOS gene is an insertion–deletion variant of a 27-bp repeat in intron 4, primarily resulting in two common alleles: the ‘a’ deletion, which has four tandem repeats, and the ‘b’ insertion, having five repeats. The eNOSI4 4a polymorphism has been associated with altered plasma NO concentrations [36, 37], hypertension [38] and vascular disease including stroke in young black women [39]. In addition to the 4a and 4b variant of the eNOSI4 polymorphism we detected a further VNTR variant carrying an additional 27-bp repeat: the variant 4c, in 22 of the 220 African women. This variant has been described before solely in black subjects and always in low frequency (8/100 Tanus-Santos et al. [35] 5/1,043 Sigusch et al. [40]). Since the low prevalence of the 4c allele does not allow association studies revealing significant evidence and, in accordance to observational studies where individuals carrying the 4c allele all suffered from either hypertension, depressed left ventricular function or myocardial infarction [40], as found in carriers of the 4a allele, it has been suggested before to subsume 4c and 4a [35]. In our African study group the allele frequencies were 0.33 for 4a, 0.62 for 4b and 0.05 for 4c. 4c could not be found in the 250 Caucasian women. Consequently, for statistical analysis we subsumed 4c and 4a variants. Despite the clear association of the 4a/4c polymorphism of eNOSI4 with severe vascular disease, studies on the association of the 4a/4b polymorphism with preeclampsia have so far failed to demonstrate increased susceptibility of 4a carriers [11, 41]. Again, ethnic diversity and inhomogeneity of study populations have been made accountable for the conflicting results. In contrast our data clearly show significant association of the 4a polymorphism with a 1.7-fold increased risk to develop preeclampsia in pregnancy.
Epoxide hydrolases (EPHX) catalyze the hydrolysis of potentially genotoxic epoxides to their corresponding vicinal diols by the addition of water. Two mammalian enzymes, microsomal (EPHX1) and soluble epoxide hydrolase (EPHX2), have been described. The hydrolysis of an epoxide results in an increased water solubility of the metabolites and terminates their action. Beyond detoxification of epoxides the microsomal EPHX1 is involved in bioactivation, and thus toxification, of polycyclic aromatic hydrocarbon benzo[a]pyrene [42]. Endogenous epoxides, in particular epoxides derived from unsaturated fatty acids with low chemical reactivity, serve as important signaling molecules. Exemplarily, the epoxyeicosatrienoic acids (EETs) derived from arachidonic acid have evidently been shown to accelerate protective function and prevent myocardial failure in cases of high blood pressure. Consequently, association of genetic polymorphisms accounting for a more active form of EPHX2 with susceptibility to cardiac failure in cases of high blood pressure has been confirmed [43]. Furthermore, epoxides regulate a large variety of physiological functions, ranging from the regulation of vascular tone, to inflammation, angiogenesis and pain. Also, certain steroids like estroxide [44] or androstene oxide involved in reproductive function and development are endogenous substrates for EPHX1. Thus, a role of EPHX1 in a variety of signaling cascades cannot be excluded, particularly in the case of high EPHX1 expression in certain organs, like the liver. Additionally, latest reports connect EPHX1 to neurodegenerative disorders such as Alzheimer’s and Parkinson’s disease [45, 46] and the anticonvulsant valpromide was identified as a potent EPHX1 inhibitor [47], suggesting a function of EPHX1 in central nervous system signaling.
Two prominent genetic polymorphisms (Tyr113His and His139Arg) have been identified in the coding region of EPHX1 [48]. The protein variants resulting from the different haplotypes have been reported to result in different enzyme half lives [49] and have impact on EPHX1 activity in vivo. The Tyr113 to His113 substitution decreases enzyme activity by approximately 40–50 % and the His139 to Arg139 exchange increases the enzymatic activity by 25 % [50]. The association of the EPHX1 polymorphism with preeclampsia has been studied in various populations, so far generating inconsistent results. Zusterzeel et al. [51] investigated the association of EPHX1 polymorphisms with preeclampsia in 167 white women with preeclampsia and 110 controls. The authors demonstrate a significant association of the Tyr113 variant with preeclampsia compared with controls in their population. In a study of 271 preeclamptic and 155 healthy Turkish women these results could not be confirmed [52]. Laasanen et al. [53] studied a group of 133 preeclamptic pregnancies and 115 controls in a Finish population. They failed to show any association of a single polymorphism in the EPHX1 gene with preeclampsia. However, their data demonstrate significant association of the Tyr113/Arg139 with the development of preeclampsia, suggesting the high-activity haplotype of the EPHX1 to predispose to preeclampsia. Furthermore, a study in Colored women in South Africa, comparing 144 preeclamptic patients with 156 controls, did not reveal significant association between EPHX1 polymorphism and preeclampsia [54]. According to the authors the Colored population of South Africa is a homogenous population possessing a blood group pattern constituting of approximately 34 % Western European, 35 % South African and 30 % Asian genes [54]. The diversity of these results again clearly demonstrates the high impact of study population ethnicity on the results. The allele frequency of the His113 allele varies between 0.19 in African and 0.64 in Dutch Caucasian [54]. In our study the allele frequency of the 113His was 0.15 in the African women and 0.31 in the Caucasian. Thus, the identification of polymorphisms associated with, or predisposing for the development of preeclampsia necessarily demands statistical analysis accounting for ethnicity. Therefore, our results demonstrating an association of the risk to develop severe preeclampsia with decreased frequency of the 113His allele in the Caucasian as well as in the African study group clearly hints to the fast EPHX1 being a susceptibility factor for the severe course of the disease. Consequently, the performed multivariate regression analysis accounting for ethnicity revealed a 3.6-fold elevated risk to suffer the severe course of preeclampsia in the presence of the 113Tyr allele. In consideration of the potential signaling function of EPHX1 in the central nervous system and its organ specific distribution, accumulating EPHX1 in the liver, susceptibility to the liver dominated HELLP syndrome and the central nervous system dominated eclampsia may well be explained by altered EPHX1 reactivity. Additionally, although the enzymatic pathways of EPHX1 are far less well described compared with those of EPHX2, it might be reasonable to assume a similar role in influencing the amount of EETs being available in endothelial cells. In endothelial cells EETs have been shown to ensure vasodilatative function, especially if NO is less available [55, 56]. EETs have been shown to be substrate to EPHX1 [42]. Thus, enhanced EPHX activity would, in cases of preeclampsia, when NO-mediated vasodilatation is impaired, explain the additional impact on severity of the disease by diminishing EETs acting as vasodilators in the absence of NO.
There are three potential limitations of the presented study. Due to the hospital-based study taking place in referral centers for preeclamptic patients in Germany as well as in Ghana the prevalence of preeclampsia was especially high, potentially tampering the results. Second, data analysis did not account for late- and early-onset preeclampsia and the time point of onset of preeclampsia was not included into the definition of severe preeclampsia in either study group. In the Caucasian study group onset of the disease was before 28 weeks of gestation in 13 of 74 patients. Of these 13 patients seven have been categorized as severe because of the development of a HELLP syndrome. Exact data accounting for the onset of pregnancy have not been available for most patients in the African study group. Third, the occurrence of intrauterine growth restriction (IUGR) was not included into the data analysis. In the Caucasian study group percentage of IUGR was similar in all groups (control, mild and severe preeclampsia). In the African study group exact estimation of the delivery date was usually impossible. Thus, definition of IUGR was not reliable. However, there were no growth-restricted(?) babies born in the African preeclamptic study group, except of five dead born. In consideration of these limitations our data primarily reflects the maternal part of the disease. Consequently, following the concept of preeclampsia being a two stage disease [7, 8], the presented results relate to maternal susceptibility to react to placental signals and to develop preeclampsia. In accordance, our data supports the concept of the mother’s genetic background determining the individual course of the disease rather than predisposing to develop preeclampsia.
Perspectives
In conclusion, eNOSI4 polymorphisms VNTR 4a revealed to be predisposing to preeclampsia independently of ethnicity, age and parity, increasing the risk to develop preeclampsia by 1.7-fold. This finding supports the old concept of NO being a key player in the endothelial disorder preeclampsia. Furthermore, the EPHX1 polymorphism 113Tyr significantly increases the risk to develop a HELLP syndrome or eclampsia in cases of preeclampsia by 3.6-fold. Since EPHX1 is highly expressed in the liver, can interact with various signaling pathways and has been shown to be involved in central nervous system disorders, this enzyme suggests it to be worthwhile to further elucidate its role in the maternal disease of preeclampsia.
References
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R (2010) Pre-eclampsia. Lancet 376(9741):631–644. doi:10.1016/S0140-6736(10)60279-6
Haram K, Svendsen E, Abildgaard U (2009) The HELLP syndrome: clinical issues and management. A review. BMC Pregnancy Childbirth 9:8. doi:10.1186/1471-2393-9-8
Hladunewich MA, Myers BD, Derby GC, Blouch KL, Druzin ML, Deen WM, Naimark DM, Lafayette RA (2008) Course of preeclamptic glomerular injury after delivery. Am J Physiol Ren Physiol 294(3):F614–F620. doi:10.1152/ajprenal.00470.2007
Bellamy L, Casas JP, Hingorani AD, Williams DJ (2007) Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 335(7627):974. doi:10.1136/bmj.39335.385301.BE
McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ (2008) Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J 156(5):918–930. doi:10.1016/j.ahj.2008.06.042
Bushnell C, Chireau M (2011) Preeclampsia and stroke: risks during and after pregnancy. Stroke Res Treat 2011:858134. doi:10.4061/2011/858134
Roberts JM, Hubel CA (2009) The two stage model of preeclampsia: variations on the theme. Placenta 30(Suppl A):S32–S37. doi:10.1016/j.placenta.2008.11.009
Huppertz B (2008) Placental origins of preeclampsia: challenging the current hypothesis. Hypertension 51(4):970–975. doi:10.1161/HYPERTENSIONAHA.107.107607
Mutze S, Rudnik-Schoneborn S, Zerres K, Rath W (2008) Genes and the preeclampsia syndrome. J Perinat Med 36(1):38–58. doi:10.1515/JPM.2008.004
Schroeder BM (2002) ACOG practice bulletin on diagnosing and managing preeclampsia and eclampsia. American college of obstetricians and gynecologists. Am Fam Physician 66(2):330–331
Tempfer CB, Dorman K, Deter RL, O’Brien WE, Gregg AR (2001) An endothelial nitric oxide synthase gene polymorphism is associated with preeclampsia. Hypertens Pregnancy 20(1):107–118. doi:10.1081/PRG-100104177
Tempfer CB, Jirecek S, Riener EK, Zeisler H, Denschlag D, Hefler L, Husslein PW (2004) Polymorphisms of thrombophilic and vasoactive genes and severe preeclampsia: a pilot study. J Soc Gynecol Investig 11(4):227–231. doi:10.1016/j.jsgi.2003.12.002
Medica I, Kastrin A, Peterlin B (2007) Genetic polymorphisms in vasoactive genes and preeclampsia: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 131(2):115–126. doi:10.1016/j.ejogrb.2006.10.005
Ward K, Hata A, Jeunemaitre X, Helin C, Nelson L, Namikawa C, Farrington PF, Ogasawara M, Suzumori K, Tomoda S et al (1993) A molecular variant of angiotensinogen associated with preeclampsia. Nat Genet 4(1):59–61. doi:10.1038/ng0593-59
Motawi T, Shaker O, Taha M, Sedrak H, Nabil M (2011) Endothelial nitric oxide synthase and angiotensinogen gene polymorphism in coronary artery diseases in Egypt. Angiology 62(2):191–197. doi:10.1177/0003319710373094
Morgan T, Ward K (1999) New insights into the genetics of preeclampsia. Semin Perinatol 23(1):14–23
Groten T, Pierce AA, Huen AC, Schnaper HW (2005) 17 beta-estradiol transiently disrupts adherens junctions in endothelial cells. FASEB J 19(10):1368–1370. doi:10.1096/fj.04-2558fje
Ellis JA, Infantino T, Harrap SB (2004) Sex-dependent association of blood pressure with oestrogen receptor genes ERalpha and ERbeta. J Hypertens 22(6):1127–1131 (pii: 00004872-200406000-00013)
Schuit SC, Oei HH, Witteman JC, Geurts van Kessel CH, van Meurs JB, Nijhuis RL, van Leeuwen JP, de Jong FH, Zillikens MC, Hofman A, Pols HA, Uitterlinden AG (2004) Estrogen receptor alpha gene polymorphisms and risk of myocardial infarction. JAMA 291(24):2969–2977. doi:10.1001/jama.291.24.2969
Herrington DM, Howard TD, Brosnihan KB, McDonnell DP, Li X, Hawkins GA, Reboussin DM, Xu J, Zheng SL, Meyers DA, Bleecker ER (2002) Common estrogen receptor polymorphism augments effects of hormone replacement therapy on E-selectin but not C-reactive protein. Circulation 105(16):1879–1882
Molvarec A, Ver A, Fekete A, Rosta K, Derzbach L, Derzsy Z, Karadi I, Rigo J Jr (2007) Association between estrogen receptor alpha (ESR1) gene polymorphisms and severe preeclampsia. Hypertens Res 30(3):205–211. doi:10.1291/hypres.30.205
Zhang J, Bai H, Liu X, Fan P, Liu R, Huang Y, Wang X, He G, Liu Y, Liu B (2009) Genotype distribution of estrogen receptor alpha polymorphisms in pregnant women from healthy and preeclampsia populations and its relation to blood pressure levels. Clin Chem Lab Med 47(4):391–397. doi:10.1515/CCLM.2009.096
Rush JW, Denniss SG, Graham DA (2005) Vascular nitric oxide and oxidative stress: determinants of endothelial adaptations to cardiovascular disease and to physical activity. Can J Appl Physiol 30(4):442–474
Fisher AB, Chien S, Barakat AI, Nerem RM (2001) Endothelial cellular response to altered shear stress. Am J Physiol Lung Cell Mol Physiol 281(3):L529–L533
Webb A, Bond R, McLean P, Uppal R, Benjamin N, Ahluwalia A (2004) Reduction of nitrite to nitric oxide during ischemia protects against myocardial ischemia-reperfusion damage. Proc Natl Acad Sci USA 101(37):13683–13688. doi:10.1073/pnas.0402927101
Morris NH, Eaton BM, Dekker G (1996) Nitric oxide, the endothelium, pregnancy and pre-eclampsia. Br J Obstet Gynaecol 103(1):4–15
Nakayama M, Yoshimura M, Sakamoto T, Abe K, Yamamuro M, Shono M, Suzuki S, Nishijima T, Miyamoto Y, Saito Y, Nakao K, Yasue H, Ogawa H (2006) A -786T > C polymorphism in the endothelial nitric oxide synthase gene reduces serum nitrite/nitrate levels from the heart due to an intracoronary injection of acetylcholine. Pharmacogenet Genomics 16(5):339–345. doi:10.1097/01.fpc.0000199499.08725.d5
Casas JP, Cavalleri GL, Bautista LE, Smeeth L, Humphries SE, Hingorani AD (2006) Endothelial nitric oxide synthase gene polymorphisms and cardiovascular disease: a HuGE review. Am J Epidemiol 164(10):921–935. doi:10.1093/aje/kwj302
Veldman BA, Spiering W, Doevendans PA, Vervoort G, Kroon AA, de Leeuw PW, Smits P (2002) The Glu298Asp polymorphism of the NOS 3 gene as a determinant of the baseline production of nitric oxide. J Hypertens 20(10):2023–2027
Hingorani AD, Liang CF, Fatibene J, Lyon A, Monteith S, Parsons A, Haydock S, Hopper RV, Stephens NG, O’Shaughnessy KM, Brown MJ (1999) A common variant of the endothelial nitric oxide synthase (Glu298– > Asp) is a major risk factor for coronary artery disease in the UK. Circulation 100(14):1515–1520
Kim IJ, Bae J, Lim SW, Cha DH, Cho HJ, Kim S, Yang DH, Hwang SG, Oh D, Kim NK (2007) Influence of endothelial nitric oxide synthase gene polymorphisms (-786T > C, 4a4b, 894G > T) in Korean patients with coronary artery disease. Thromb Res 119(5):579–585. doi:10.1016/j.thromres.2006.06.005
Tang W, Yang Y, Wang B, Xiao C (2008) Association between a G894T polymorphism of eNOS gene and essential hypertension in Hani and Yi minority groups of China. Arch Med Res 39(2):222–225. doi:10.1016/j.arcmed.2007.08.002
Hakli T, Romppanen EL, Hiltunen M, Helisalmi S, Punnonen K, Heinonen S (2003) Endothelial nitric oxide synthase polymorphism in preeclampsia. J Soc Gynecol Investig 10(3):154–157 (pii:S1071557603000030)
Serrano NC, Casas JP, Diaz LA, Paez C, Mesa CM, Cifuentes R, Monterrosa A, Bautista A, Hawe E, Hingorani AD, Vallance P, Lopez-Jaramillo P (2004) Endothelial NO synthase genotype and risk of preeclampsia: a multicenter case-control study. Hypertension 44(5):702–707. doi:10.1161/01.HYP.0000143483.66701.ec
Tanus-Santos JE, Desai M, Flockhart DA (2001) Effects of ethnicity on the distribution of clinically relevant endothelial nitric oxide variants. Pharmacogenetics 11(8):719–725
Tsukada T, Yokoyama K, Arai T, Takemoto F, Hara S, Yamada A, Kawaguchi Y, Hosoya T, Igari J (1998) Evidence of association of the ecNOS gene polymorphism with plasma NO metabolite levels in humans. Biochem Biophys Res Commun 245(1):190–193. doi:10.1006/bbrc.1998.8267
Sandrim VC, Palei AC, Sertorio JT, Cavalli RC, Duarte G, Tanus-Santos JE (2010) Effects of eNOS polymorphisms on nitric oxide formation in healthy pregnancy and in pre-eclampsia. Mol Hum Reprod 16(7):506–510. doi:10.1093/molehr/gaq030
Wang XL, Wang J (2000) Endothelial nitric oxide synthase gene sequence variations and vascular disease. Mol Genet Metab 70(4):241–251. doi:10.1006/mgme.2000.3033
Howard TD, Giles WH, Xu J, Wozniak MA, Malarcher AM, Lange LA, Macko RF, Basehore MJ, Meyers DA, Cole JW, Kittner SJ (2005) Promoter polymorphisms in the nitric oxide synthase 3 gene are associated with ischemic stroke susceptibility in young black women. Stroke 36(9):1848–1851. doi:10.1161/01.STR.0000177978.97428.53
Sigusch HH, Surber R, Lehmann MH, Surber S, Weber J, Henke A, Reinhardt D, Hoffmann A, Figulla HR (2000) Lack of association between 27-bp repeat polymorphism in intron 4 of the endothelial nitric oxide synthase gene and the risk of coronary artery disease. Scand J Clin Lab Invest 60(3):229–235
Aggarwal PK, Jain V, Jha V (2010) Endothelial nitric oxide synthase, angiotensin-converting enzyme and angiotensinogen gene polymorphisms in hypertensive disorders of pregnancy. Hypertens Res 33(5):473–477. doi:10.1038/hr.2010.23
Decker M, Arand M, Cronin A (2009) Mammalian epoxide hydrolases in xenobiotic metabolism and signalling. Arch Toxicol 83(4):297–318. doi:10.1007/s00204-009-0416-0
Monti J, Fischer J, Paskas S, Heinig M, Schulz H, Gosele C, Heuser A, Fischer R, Schmidt C, Schirdewan A, Gross V, Hummel O, Maatz H, Patone G, Saar K, Vingron M, Weldon SM, Lindpaintner K, Hammock BD, Rohde K, Dietz R, Cook SA, Schunck WH, Luft FC, Hubner N (2008) Soluble epoxide hydrolase is a susceptibility factor for heart failure in a rat model of human disease. Nat Genet 40(5):529–537. doi:10.1038/ng.129
Fandrich F, Degiuli B, Vogel-Bindel U, Arand M, Oesch F (1995) Induction of rat liver microsomal epoxide hydrolase by its endogenous substrate 16 alpha, 17 alpha-epoxyestra-1,3,5-trien-3-ol. Xenobiotica 25(3):239–244. doi:10.3109/00498259509061848
Liu M, Sun A, Shin EJ, Liu X, Kim SG, Runyons CR, Markesbery W, Kim HC, Bing G (2006) Expression of microsomal epoxide hydrolase is elevated in Alzheimer’s hippocampus and induced by exogenous beta-amyloid and trimethyl-tin. Eur J Neurosci 23(8):2027–2034. doi:10.1111/j.1460-9568.2006.04724.x
Farin FM, Janssen P, Quigley S, Abbott D, Hassett C, Smith-Weller T, Franklin GM, Swanson PD, Longstreth WT Jr, Omiecinski CJ, Checkoway H (2001) Genetic polymorphisms of microsomal and soluble epoxide hydrolase and the risk of Parkinson’s disease. Pharmacogenetics 11(8):703–708
Robbins DK, Wedlund PJ, Elsberg S, Oesch F, Thomas H (1992) Interaction of valproic acid and some analogues with microsomal epoxide hydrolase. Biochem Pharmacol 43(4):775–783
Omiecinski CJ, Hassett C, Hosagrahara V (2000) Epoxide hydrolase-polymorphism and role in toxicology. Toxicol Lett 112–113:365–370 (pii: S0378427499002350)
Hassett C, Lin J, Carty CL, Laurenzana EM, Omiecinski CJ (1997) Human hepatic microsomal epoxide hydrolase: comparative analysis of polymorphic expression. Arch Biochem Biophys 337(2):275–283. doi:10.1006/abbi.1996.9794
Rosenberger A, Illig T, Korb K, Klopp N, Zietemann V, Wolke G, Meese E, Sybrecht G, Kronenberg F, Cebulla M, Degen M, Drings P, Groschel A, Konietzko N, Kreymborg KG, Haussinger K, Hoffken G, Jilge B, Ko YD, Morr H, Schmidt C, Schmidt EW, Tauscher D, Bickeboller H, Wichmann HE (2008) Do genetic factors protect for early onset lung cancer? A case control study before the age of 50 years. BMC Cancer 8:60. doi:10.1186/1471-2407-8-60
Zusterzeel PL, Peters WH, Visser W, Hermsen KJ, Roelofs HM, Steegers EA (2001) A polymorphism in the gene for microsomal epoxide hydrolase is associated with pre-eclampsia. J Med Genet 38(4):234–237
Pinarbasi E, Percin FE, Yilmaz M, Akgun E, Cetin M, Cetin A (2007) Association of microsomal epoxide hydrolase gene polymorphism and pre-eclampsia in Turkish women. J Obstet Gynaecol Res 33(1):32–37. doi:10.1111/j.1447-0756.2007.00473.x
Laasanen J, Romppanen EL, Hiltunen M, Helisalmi S, Mannermaa A, Punnonen K, Heinonen S (2002) Two exonic single nucleotide polymorphisms in the microsomal epoxide hydrolase gene are jointly associated with preeclampsia. Eur J Hum Genet 10(9):569–573. doi:10.1038/sj.ejhg.5200849
Gebhardt GS, Peters WH, Hillermann R, Odendaal HJ, Carelse-Tofa K, Raijmakers MT, Steegers EA (2004) Maternal and fetal single nucleotide polymorphisms in the epoxide hydrolase and gluthatione S-transferase P1 genes are not associated with pre-eclampsia in the Coloured population of the Western Cape. South Africa. J Obstet Gynaecol 24(8):866–872. doi:10.1080/01443610400018841
Yousif MH, Benter IF (2010) Role of 20-hydroxyeicosatetraenoic and epoxyeicosatrienoic acids in the regulation of vascular function in a model of hypertension and endothelial dysfunction. Pharmacology 86(3):149–156. doi:10.1159/000317521
Zhang LN, Vincelette J, Chen D, Gless RD, Anandan SK, Rubanyi GM, Webb HK, MacIntyre DE, Wang YX (2011) Inhibition of soluble epoxide hydrolase attenuates endothelial dysfunction in animal models of diabetes, obesity and hypertension. Eur J Pharmacol 654(1):68–74. doi:10.1016/j.ejphar.2010.12.016
Acknowledgments
The authors thank Yasmin Windisch and Sonja Wolfarth for their excellent technical assistance and the midwife staff in Ulm and Kumasi for their help in patient recruitment and care.
Conflict of interest
The authors confirm that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Groten, T., Schleussner, E., Lehmann, T. et al. eNOSI4 and EPHX1 polymorphisms affect maternal susceptibility to preeclampsia: analysis of five polymorphisms predisposing to cardiovascular disease in 279 Caucasian and 241 African women. Arch Gynecol Obstet 289, 581–593 (2014). https://doi.org/10.1007/s00404-013-2991-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-2991-9