Abstract
Background
The use of fluoroscopy is necessary during proximal femoral fracture (PFF) osteosynthesis. The frequency of these procedures justifies a description of radiation exposure and comparisons between different techniques and between the different surgical team members.
Methods
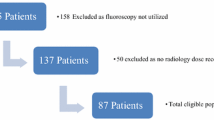
This observational prospective and comparative study includes a series of 68 patients with PFF receiving osteosynthesis. Radiation exposure was assessed for all members of the operating team. The radiation dose measurements for the different members of the surgical team during PFF osteosynthesis were compared. The factors affecting the radiation dose were investigated.
Results
The mean active dosimeter readings for each operation were 7.39 µSv for the primary surgeon, 3.93 µSv for the assistant surgeon, 1.92 µSv for the instrument nurse, 1.25 µSv for the circulating nurse, and 0.64 µSv for the anaesthesiologist, respectively. Doses decreased significantly between these different members of the medical team (all p < 0.001). The dose also varied with patient age and BMI, as well as with fluoroscopy time and operating time, but not with type of fracture or type of osteosynthesis.
Conclusion
Medical staff receives significantly different doses depending on their position in relation to the radiation source. Operating time and fluoroscopy time are the modifiable factors that affect the radiation dose. The radiation doses received by the different members of the medical teams involved in proximal femur osteosynthesis procedures all fall below the doses recommended by the International Commission on Radiation Units and Measurements.



Similar content being viewed by others
References
Müller LP, Suffner J, Wenda K et al (1998) Radiation exposure to the hands and the thyroid of the surgeon during intramedullary nailing. Injury 29:461–468
Seagger R, Howell J, David H, Gregg-Smith S (2004) Prevention of secondary osteoporotic fractures–why are we ignoring the evidence? Injury 35:986–988
Benetos IS, Babis GC, Zoubos AB et al (2007) Factors affecting the risk of hip fractures. Injury 38:735–744
Kannus P, Parkkari J, Sievänen H et al (1996) Epidemiology of hip fractures. Bone 18:57S–63S
International Commission on Radiological Protection (2010) Radiological protection in fluoroscopically guided procedures outside the imaging department. ICRP Publication 117. Ann ICRP 40
Alonso JA, Shaw DL, Maxwell A et al (2001) Scattered radiation during fixation of hip fractures. Is distance alone enough protection? J Bone Jt Surg Br 83:815–818
Plourde G, Pancholy SB, Nolan J et al (2015) Radiation exposure in relation to the arterial access site used for diagnostic coronary angiography and percutaneous coronary intervention: a systematic review and meta-analysis. Lancet 386:2192–2203
Sciahbasi A, Rigattieri S, Sarandrea A et al (2015) Operator radiation exposure during right or left transradial coronary angiography: a phantom study. Cardiovasc Revascularization Med 16:386–390
Marsh JL, Slongo TF, Agel J et al (2007) Fracture and dislocation classification compendium—2007: orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 21:S1–S133
Sulieman A, Alzimami K, Habeeballa B et al (2014) Evaluation of occupational and patient radiation doses in orthopedic surgery. Appl Radiat Isot, Med
Ramisetty NM, Pynsent PB, Abudu A (2005) Fracture of the femoral neck, the risk of serious underlying pathology. Injury 36:622–626
Cooper C, Campion G, Melton LJ (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Kesavachandran CN, Haamann F, Nienhaus A (2012) Radiation exposure of eyes, thyroid gland and hands in orthopaedic staff: a systematic review. Eur J Med Res 17:28
Johnell O, Kanis JA (2004) An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 15:897–902
Palácio EP, Ribeiro AA, Gavassi BM et al (2014) Exposure of the surgical team to ionizing radiation during orthopedic surgical procedures. Rev Bras Ortop 49:227–232
Elffors L (1998) Are osteoporotic fractures due to osteoporosis? Impacts of a frailty pandemic in an aging world. Aging Milan Italy 10:191–204
Harrison JD, Balonov M, Martin CJ et al (2016) Use of effective dose. Ann ICRP 45:215–224
Jablon S, Bailar JC (1980) The contribution of ionizing radiation to cancer mortality in the United States. Prev Med 9:219–226
Khan IA, Kamalasekaran S, Fazal MA (2012) Risk of ionising radiation to trainee orthopaedic surgeons. Acta Orthop Belg 78:106–110
Mastrangelo G, Fedeli U, Fadda E et al (2005) Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med Oxf Engl 55:498–500
Moore C, Heeckt P (2011) Reducing radiation risk in orthopaedic trauma surgery. Bone Jt Sci 2:1–6
Abas AA, Rahman RA, Yahya N et al (2014) Occupational radiation exposure to anesthetists from fluoroscopic projections during orthopedic operative procedures. Clin Ter 165:e253–e257
Dalgleish S, Hince A, Finlayson DF (2015) Peri-operative radiation exposure: are overweight patients at increased risks? Injury 46:2448–2451
Blattert TR, Fill UA, Kunz E et al (2004) Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: a clinical study. Arch Orthop Trauma Surg 124:659–664
Mehlman CT, DiPasquale TG (1997) Radiation exposure to the orthopaedic surgical team during fluoroscopy: “how far away is far enough?”. J Orthop Trauma 11:392–398
Fuchs M, Schmid A, Eiteljörge T et al (1998) Exposure of the surgeon to radiation during surgery. Int Orthop 22:153–156
Tasbas BA, Yagmurlu MF, Bayrakci K et al (2003) Which one is at risk in intraoperative fluoroscopy? Assistant surgeon or orthopaedic surgeon? Arch Orthop Trauma Surg 123:242–244. doi:10.1007/s00402-003-0516-x
Baumgartner R, Libuit K, Ren D et al (2016) Reduction of radiation exposure from C-arm fluoroscopy during orthopaedic trauma operations with introduction of real-time dosimetry. J Orthop Trauma 30:e53–e58. doi:10.1097/BOT.0000000000000442
Richter P, Dehner C, Scheiderer B et al (2013) Emission of radiation in the orthopaedic operation room: a comprehensive review. OA Musculoskeletal Medicine 1:1–11
Burns S, Thornton R, Dauer LT et al (2013) Leaded eyeglasses substantially reduce radiation exposure of the surgeon’s eyes during acquisition of typical fluoroscopic views of the hip and pelvis. J Bone Jt Surg Am 95:1307–1311
Roux A, Bronsard N, Blanchet N, de Peretti F (2011) Can fluoroscopy radiation exposure be measured in minimally invasive trauma surgery? Orthop Traumatol Surg Res OTSR 97:662–667
Botchu R, Ravikumar K (2008) Radiation exposure from fluoroscopy during fixation of hip fracture and fracture of ankle: effect of surgical experience. Indian J Orthop 42:471–473
Riley SA (1989) Radiation exposure from fluoroscopy during orthopedic surgical procedures. Clin Orthop 248:257–260
Kuon E, Weitmann K, Hoffmann W et al (2015) Multicenter long-term validation of a minicourse in radiation-reducing techniques in the catheterization laboratory. Am J Cardiol 115:367–373
Richter PH, Steinbrener J, Schicho A, Gebhard F (2016) Does the choice of mobile C-arms lead to a reduction of the intraoperative radiation dose? Injury 47:1608–1612. doi:10.1016/j.injury.2016.04.031
Lee T, Shin SW, Choi D et al (1987) Risk factors of radiation dose in patients undergoing peripherally-inserted central catheter procedure using conventional angiography equipment and flat panel detector-based mobile C-arm fluoroscopy. Acta Radiol Stockh Swed 55:1234–1238. doi:10.1177/0284185113514221
Esfandiari H, Amiri S, Lichti DD, Anglin C (2016) A fast, accurate and closed-form method for pose recognition of an intramedullary nail using a tracked C-arm. Int J Comput Assist Radiol Surg 11:621–633. doi:10.1007/s11548-015-1294-y
Khoury A, Liebergall M, Weil Y, Mosheiff R (2007) Computerized fluoroscopic-based navigation-assisted intramedullary nailing. Am J Orthop Belle Mead NJ 36:582–585
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Siedlecki, C., Gauthé, R., Gillibert, A. et al. Exposure of medical staff to radiation during osteosynthesis of proximal femoral fracture: descriptive analysis and comparison of different devices. Arch Orthop Trauma Surg 137, 1391–1397 (2017). https://doi.org/10.1007/s00402-017-2761-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2761-4