Abstract
Objective
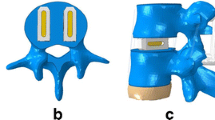
In this study, we aimed to design a movable artificial lumbar complex (MALC) prosthesis for non-fusion reconstruction after lumbar subtotal corpectomy and to establish an in vitro anterolateral lumbar corpectomy non-fusion model for evaluating the biomechanical stability, preservation of segment movements and influence on adjacent inter-vertebral movements of this prosthesis.
Methods
Imaging was performed on a total of 26 fresh goat lumbar spine specimens to determine which of the specimens did not meet the requirements (free of deformity and fractures); the residual specimens were randomly divided into an intact group, a fusion group and a non-fusion group. Bone mineral density (BMD) was tested and compared among the three groups. Biomechanical testing was conducted to obtain the range of motion (ROM) in flexion–extension, lateral bending at L2–3, L3–4 and L4–5 and axial rotation at L2–5 in the three groups.
Results
Two specimens were excluded due to vertebral fractures. BMD showed no statistical significance among three groups (P > 0.05). The stability of the prosthesis did not differ significantly during flexion, extension, and lateral bending at L2–3, L3–4, and L4–5 and axial torsion at L2–5 between the intact group and the non-fusion group (P > 0.05). Segment movements of the specimens in the non-fusion group revealed significantly decreased L2–3 ROM and significantly increased L3–4 and L4–5 ROM in flexion and lateral bending compared with the fusion group (P < 0.05).
Conclusions
Reconstruction with a MALC prosthesis after lumbar subtotal corpectomy not only produced instant stability but also effectively preserved segment movements, without any abnormal gain of mobility in adjacent inter-vertebral spaces. However, additional studies, including in vivo animal experiments as well as biocompatibility and biomechanical tests of human body specimens are needed.









Similar content being viewed by others
References
Liu P, Sun MW, Li SJ et al (2015) A retrospective controlled study of three different operative approaches for the treatment of thoracic and lumbar spinal tuberculosis: three years of follow-up. Clin Neurol Neurosurg 128(3):25–34
Wang JF, Liu P (2015) Analysis of surgical approaches for unstable thoracolumbar burst fracture: minimum of five year follow-up. J Pak Med Assoc 65(2):201–205
Denaro V, Denaro L, Albo E et al (2016) Surgical management of spinal fractures and neurological involvement in patients with myeloma. Injury 47(Suppl 4):S49–S53
Serak J, Vanni S, Levi AD (2015) The extreme lateral approach for treatment of thoracic and lumbar vertebral body metastases. J Neurosurg Sci (Epub ahead of print)
Sung SH, Chang UK (2014) Clinical significance of radiological stability in reconstructed thoracic and lumbar spine following vertebral body resection. J Korean Neurosurg Soc 56(4):323–329
Pan AX, Hai Y, Yang JC et al (2016) Adjacent segment degeneration after lumbar spinal fusion compared with motion-preservation procedures: a meta-analysis. Eur Spine J 25(5):1522–1532
Zhang C, Berven SH, Fortin M et al (2016) Adjacent segment degeneration versus disease after lumbar spine fusion for degenerative pathology: a systematic review with meta-analysis of the literature. Clin Spine Surg 1(29):21–29
Kim HJ, Kang KT, Chun HJ et al (2015) The influence of intrinsic disc degeneration of the adjacent segments on its stress distribution after one-level lumbar fusion. Eur Spine J 24(4):827–837
Rao MJ, Cao SS (2014) Artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 134(2):149–158
Wilke HJ, Kettle A, Claes LE (1997) Are sheep spines a valid biomechanical model for human spines?. Spine 22(20):2365–2374
Sheng SR, Wang XY, Xu HZ et al (2010) Anatomy of large animal spines and its comparison to the human spine: a systematic review. Euro Spine J 19(1):46–56
Smit TH (2002) The use of a quadruped as an in vivo model for the study of the spine-biomechanical considerations. Eur Spine J 11(2):137–144
Ren LX, Jiao SG, Yin J et al (2009) Effect of percutaneous laser disc decompression on normal goat lumbar biomechanical stability. Chin J Spine Spinal Cord 19(9):689–692
Zhou Z, Wang X, Wu Z et al (2017) Epidemiological characteristics of primary spinal osseous tumors in Eastern China. World J Surg Oncol 15(1):73
Grivna M, Eid HO, Abu-Zidan FM (2015) Epidemiology of spinal injuries in the United Arab Emirates. World J Emerg Surg 10:20
Hamdi FA (1969) Prosthesis for an excised lumbar vertebra: a preliminary report. Can Med Assoc J 100(12):576–580
Paulzak AN, Rusyniak WG, Gonzalez RP et al (2015) Lumbar corpectomy via retroperitoneal approach: a case series of 42 patients with traumatic lumbar fracture. J Am Coll Surg 221(4Suppl2):e143
Wang W, Liu S, He G et al (2016) Application of laparoscopic lumbar discectomy and artificial disc replacement: at least two years of follow-up. Spine 41(Suppl 19):B38–B43
Qin J, He XJ, Wang D et al (2012) Artificial cervical vertebra and intervertebral complex replacement through the anterior approach in animal model: a biomechanical and in vivo evaluation of a successful goat model. PLoS One 7(12):1–13
Dong J, Lu M, He XJ et al (2015) Artificial disc and vertebra system: a novel motion preservation device for cervical spinal disease after vertebral corpectomy. Clinics 70(7):493–499
Yu J, Liu LT, Zhao JN (2013) Design and preliminary biomechanical analysis of artificial cervical joint complex. Arch Orthop Trauma Surg 133(6):735–743
Xiao J, Huang Y-C, Lam SKL, Luk KDK (2015) Surgical technique for lumbar intervertebral disc transplantation in a goat model. Eur Spine J 24(9):1951–1958
Huang Y-C, Xiao J, Lu WW, Leung VYL, Hu Y, Luk KDK (2017) Lumbar intervertebral disc allograft transplantation: long-term mobility and impact on the adjacent segments. Eur Spine J 26(3):799–805
Weber MH, Fortin M, Shen J et al. (2016) Graft subsidence and revision rates following anterior cervical corpectomy: a clinical study comparing different interbody cages. Clin Spine Surg. doi:10.1097/BSD.0000000000000428
Acknowledgements
I would like to express my gratitude to Lu Teng, Wen Zhijing, Wang Yibin and Liang Hui. They gave us a lot of support and help during the study. I also owe a special debt of gratitude to the fund “Design and basic research of artificial atlanto-odontoid joint” (No. xjtc2014 001). In the financial support of it, we finally successfully completed this experiment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has potential conflict of interest and the manuscript has been approved by all authors for publication.
Rights and permissions
About this article
Cite this article
Liu, J., Zhang, F., Gao, Z. et al. Lumbar subtotal corpectomy non-fusion model produced using a novel prosthesis. Arch Orthop Trauma Surg 137, 1467–1476 (2017). https://doi.org/10.1007/s00402-017-2753-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2753-4