Abstract
Introduction
Tumors localized in the proximal tibial meta-diaphysis often lead to osteoarticular resections.
Materials and methods
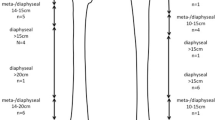
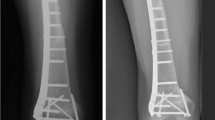
In this study, we retrospectively reviewed four patients who underwent intercalary tumor resection and reconstruction using an ultra-short stem in the proximal tibial epiphysis, a procedure that to our knowledge has not been reported in literature so far.
Results
At the time of operation, the mean patient age was 26.2 years. Three patients were male and one was female. Patients were diagnosed with osteosarcoma in two cases, Ewing’s sarcoma and malignant fibrous histiocytoma of bone in one case each. In all cases, wide tumor resections were achieved (osteotomy 3–3.5 cm below the tibia plateau joint surface, mean resection length of tibial bone 18 cm) at a mean time of operation of 198.8 min. Two superficial wound-healing disorders occurred, leading to one surgical revision in each case. One local tumor recurrence occurred 12 months after operation in a patient who discontinued his adjuvant chemotherapy. This patient died of disease, 31 months after operation. Three patients are alive with no evidence of disease at a mean follow-up of 56 months. Walking is not impaired and light sports activities have been reported in all cases. The mean MSTS score is 28/30.
Conclusions
Therefore, we report this reconstruction technique to be considered for special indications where the functional outcome can be improved by preservation of the knee joint in tumors of the proximal meta-diaphyseal tibial region.





Similar content being viewed by others
References
Aldlyami E, Abudu A, Grimer RJ, Carter SR, Tillman RM (2008) Endoprosthetic replacement of diaphyseal bone defects. Int Orthop 29(1):25–29
Fuchs B, Ossendorf C, Leerapun T, Sim FH (2008) Intercalary segmental reconstruction after bone tumor resection. Eur J Surg Oncol 34(12):1271–1276
Sewell MD, Hanna SA, McGrath A, Aston WJ, Blunn GW, Pollock RC, Skinner JA, Cannon SR, Briggs TW (2011) Intercalary diapyhseal endoprosthetic reconstruction for malignant tibial bone tumours. J Bone Joint Surg Br 93(8):1111–1117
Friedrich MJ, Schmolders J, Lob G, Randau TM, Gravius S, Wirtz DC, Pennekamp PH (2015) Intercalary reconstruction for diaphyseal bone defects with a modular replacement system: Clinical results. Oper Orthop Traumatol 27(5):455–462
Aponte-Tinao L, Farfalli GL, Ritacco LE, Ayerza MA, Muscolo DL (2012) Intercalary femur allografts are an acceptable alternative after tumor resection. Clin Orthop Relat Res 470(3):728–734
Ahlmann ER, Menendez LR (2006) Intercalary endoprosthetic reconstruction for diaphyseal bone tumours. J Bone Joint Surg Br 88(11):1487–1491
Benevenia J, Kirchner R, Patterson F, Beebe K, Wirtz DC, Rivero S, Palma M, Friedrich MJ (2016) Outcomes of a modular intercalary endoprosthesis as treatment for segmental defects of the femur, tibia, and humerus. Clin Orthop Relat Res 474(2):539–548
Hardes J, Henrichs MP, Gosheger G, Gebert C, Höll S, Dieckmann R, Hauschild G, Streitbürger A (2013) Endoprosthetic replacement after extra-articular resection of bone and soft-tissue tumours around the knee. Bone Joint J 95-B(10):1425–1431
Streitbürger A, Gosheger G, Dieckmann R, Nottrott M, Ahrens H, Hardes J (2014) Bone defect reconstruction in bone sarcoma surgery: tumour endoprosthesis versus biological reconstruction. Unfallchirurg 117(7):600–606
Myers GJ, Abudu AT, Carter SR, Tillman RM, Grimer RJ (2007) The long-term results of endoprosthetic replacement of the proximal tibia for bone tumours. J Bone Joint Surg Br 89(12):1632–1637
Capanna R, Scoccianti G, Frenos F, Vilardi A, Beltrami G, Campanacci DA (2015) What was the survival of megaprostheses in lower limb reconstructions after tumor resections? Clin Orthop Relat Res 473(3):820–830
Aponte-Tinao LA, Ayerza MA, Muscolo DL, Farfalli GL (2016) What are the risk factors and management options for infection after reconstruction with massive bone allografts? Clin Orthop Relat Res 474(3):669–673
Campanacci L, Manfrini M, Colangeli M, Alí N, Mercuri M (2010) Long-term results in children with massive bone osteoarticular allografts of the knee for high-grade osteosarcoma. J Pediatr Orthop 30(8):919–927
Aponte-Tinao L, Ayerza MA, Muscolo DL, Farfalli GL (2015) Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin Orthop Relat Res 473(5):1789–1796
Campanacci L, Alì N, Casanova JM, Kreshak J, Manfrini M (2015) Resurfaced allograft-prosthetic composite for proximal tibial reconstruction in children: intermediate-term results of an original technique. J Bone Joint Surg Am 97(3):241–250
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study (retrospective study design), formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Guder, W.K., Hardes, J., Gosheger, G. et al. Ultra-short stem anchorage in the proximal tibial epiphysis after intercalary tumor resections: analysis of reconstruction survival in four patients at a mean follow-up of 56 months. Arch Orthop Trauma Surg 137, 481–488 (2017). https://doi.org/10.1007/s00402-017-2637-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2637-7