Abstract
Introduction
Benign lytic lesions of bone encompass a group of neoplastic or developmental disorders of human skeleton. They may involve different sites with varied clinical presentation and pattern of aggressiveness for which the treatment strategy needs to be tailored accordingly. Planning a treatment protocol for a lytic lesion in the femoral neck is a matter of concern for the operating surgeon with due consideration to the risks involved.
Patients and method
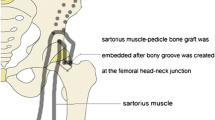
This prospective study comprised of 16 patients (9 females and 7 males) with an average age of 23.37 years (range 14 to 35) who presented with lytic lesion in the neck of femur. Only those lesions which were involving the anterior or the inferior aspect of the femoral neck in which the destruction was more than 50 % of the cortex in a single view or there was a pathological fracture were included in this study. There were six cases of giant cell tumour, five cases of fibrous dysplasia, four cases of aneurysmal bone cyst and one case of benign fibrous histiocytoma. All the lesions were operated using anterior approach, and after extended curettage, the cavity was packed with bone chips and sartorius-based muscle pedicle bone grafting (MPBG) was done. Four patients presented with pathological fracture in which the fibula strut grafting was done in addition to MPBG. The patients were assessed using Musculoskeletal Tumour Society (MSTS) score. The mean follow-up period was 32 months (range 26–74 months).
Results
The average time to clinical healing was 8 weeks (range 6–12 weeks) in patients without pathological fracture at the presentation. At final follow-up, the average MSTS score was 28.2 and full radiological consolidation had occurred in all but one patient who developed recurrence. There was no evidence of avascular necrosis or pathological fracture in any of the cases.
Conclusions
Sartorius muscle pedicle bone grafting using anterior approach is a good and reliable option in patients presenting with benign lytic lesion in the neck of femur.




Similar content being viewed by others
References
Eyesan SU, Idowu OK, Obalum DC, Nnodu OE, Abdulkareem FB (2011) Surgical consideration for benign bone tumors. Niger J Clin Pract 14(2):146–150
Aston W, Briggs T, Solomon L (2010) Tumours. In: Solomon L, Warwick D, Nayagam S (eds) Apley’s system of Orthopaedics and Fractures, 9th edn. Hooder Arnold, London, pp 187–223
Jeys LM, Suneja R, Chami G, Grimer RJ, Carter SR, Tillman RM (2006) Impending fractures in giant cell tumours of the distal femur: incidence and outcome. Int Orthop 30(2):135–138
Mirels H (1989) Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 249:256–264
Enneking WF (1986) A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res 204:9–24
Smith-peterson MN (1917) A new supra-articular subperiosteal approach to hip joint. Am J Orthop Surg 15:592
Smith-peterson MN (1949) Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am 31(1):40–46
Puri A, Agarwal M (2007) Treatment of giant cell tumor of bone: current concepts. Indian J Orthop 41(2):101–108
Baksi DP (1983) Treatment of post-traumatic avascular necrosis of the femoral head by multiple drilling and muscle pedicle bone grafting preliminary report. J Bone Joint Surg Br 65(3):268–273
Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 286:241–246
Hirn M, de Silva U, Sidharthan S, Grimer RJ, Abudu A, Tillman RM, Carter SR (2009) Bone defects following curettage do not necessarily need augmentation. Acta Orthop 80(1):4–8
Kreicbergs A, Lönnqvist PA, Nilsson B (1985) Curettage of benign lesions of bone Factors related to recurrence. Int Orthop 8(4):287–294
Tomford WW (1995) Transmission of disease through transplantation of musculoskeletal allografts. J Bone Joint Surg Am 77(11):1742–1754
Reppenhagen S, Reichert JC, Rackwitz L, Rudert M, Raab P, Daculsi G, Nöth U (2012) Biphasic bone substitute and fibrin sealant for treatment of benign bone tumours and tumour-like lesions. Int Orthop 36(1):139–148
Bucholz RW (2002) Nonallograft osteoconductive bone graft substitutes. Clin Orthop Relat Res 395:44–52
Bauer TW, Muschler GF (2000) Bone graft materials. An overview of the basic science. Clin Orthop Relat Res 371:10–27
Dinopoulos H, Dimitriou R, Giannoudis PV (2012) Bone graft substitutes: what are the options? Surgeon 10(4):230–239
Trueta J, Harrison MH (1953) The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br 35(3):442–461
Baksi DP (1991) Treatment of osteonecrosis of the femoral head by drilling and muscle pedicle bone grafting. J Bone Joint Surg Br 73(2):241–245
Baksi DP, Pal AK, Baksi DD (2009) Long-term results of decompression and muscle-pedicle bone grafting for osteonecrosis of the femoral head. Int Orthop 33(1):41–47
Merle D’Aubigné R, Postel M, Mazabraud A, Massias P, Gueguen J, France P (1965) Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br 47(4):612–633
Saito S, Ohzono K, Ono K (1988) Joint-preserving operations for idiopathic avascular necrosis of the femoral head. Results of core decompression, grafting and osteotomy. J Bone Joint Surg Br 70(1):78–84
Liu GP, Kang B, Zeng H, Tang YK, Tang XY, Xiong A, Xie XC, Huang W (2003) Treatment of femoral neck fracture with muscle-bone flap of both tensor fasciae latae and sartorius. Chin J Traumatol 6(4):238–241
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kundu, Z.S., Gogna, P., Sangwan, S.S. et al. Benign lytic lesions of the femoral neck: mid-term results of extended curettage and sartorius muscle pedicle bone grafting. Arch Orthop Trauma Surg 133, 457–462 (2013). https://doi.org/10.1007/s00402-013-1687-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1687-8