Abstract
Purpose
The possible impact of preload food on insulin sensitivity has yet been reported. This study aimed to investigate the glycemic and insulinemic effect of an apple preload before breakfast, lunch and early supper, based on high glycemic index (GI) rice meals.
Methods
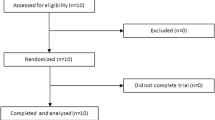
Twenty-three healthy participants in Group 1 and 14 participants in Group 2 were served with the reference meal (white rice containing 50 g of available carbohydrate) or experimental meals (apple preload and rice, each containing 15 and 35 g of available carbohydrate). The meals were either served at 8:00 for breakfast, 12:30 for lunch or 17:00 for early supper to explore the possible effect of time factor. The group 1 assessed the postprandial and subsequent-meal glycemic effect of the test meals by continuous glucose monitoring (CGM), along with subjective appetite; The group 2 further investigated the glycemic and insulin effect by blood collection.
Results
The apple preload lowered the blood glucose peak value by 33.5%, 31.4% and 31.0% in breakfast, lunch and supper, respectively, while increased insulin sensitivity by 40.5% only at breakfast, compared with the rice reference. The early supper resulted significantly milder glycemic response than its breakfast and lunch counterparts did. The result of CGM tests was consistent with that of the fingertip blood tests.
Conclusion
Apple preload performed the best at breakfast in terms of enhancing the insulin sensitivity. The preload treatment could effectively attenuate postprandial GR without increasing the area under insulin response curve in any of the three meals.







Similar content being viewed by others
Data availability
After publication, all data necessary to understand and assess the conclusions of the manuscript are available to any reader of the European Journal of Nutrition.
References
Mone P, Gambardella J, Pansini A, de Donato A, Martinelli G, Boccalone E, Matarese A, Frullone S, Santulli G (2021) Cognitive impairment in frail hypertensive elderly patients: role of hyperglycemia. Cells-Basel 10:2115
Skrha J, Soupal J, Skrha JJ, Prazny M (2016) Glucose variability, HbA1c and microvascular complications. Rev Endocr Metab Disord 17:103–110
Takao T, Suka M, Yanagisawa H, Iwamoto Y (2017) Impact of postprandial hyperglycemia at clinic visits on the incidence of cardiovascular events and all-cause mortality in patients with type 2 diabetes. J Diabetes Investig 8:600–608
Cavalot F, Pagliarino A, Valle M, Di Martino L, Bonomo K, Massucco P, Anfossi G, Trovati M (2011) Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a 14-year follow-up: lessons from the san luigi gonzaga diabetes study. Diabetes Care 34:2237–2243
Loader J, Montero D, Lorenzen C, Watts R, Meziat C, Reboul C, Stewart S, Walther G (2015) Acute hyperglycemia impairs vascular function in healthy and cardiometabolic diseased subjects systematic review and meta-analysis. Arterioscl Throm Vas 35:2060–2072
Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW (2009) Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring) 17:2100–2102
Poggiogalle E, Jamshed H, Peterson CM (2018) Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 84:11–27
Leung G, Huggins CE, Ware RS, Bonham MP (2020) Time of day difference in postprandial glucose and insulin responses: systematic review and meta-analysis of acute postprandial studies. Chronobiol Int 37:311–326
Wee M, Henry CJ (2020) Reducing the glycemic impact of carbohydrates on foods and meals: strategies for the food industry and consumers with special focus on Asia. Compr Rev Food Sci Food Saf 19:670–702
Sun L, Tan K, Han C, Leow MK, Henry CJ (2017) Impact of preloading either dairy or soy milk on postprandial glycemia, insulinemia and gastric emptying in healthy adults. Eur J Nutr 56:77–87
Wu T, Little TJ, Bound MJ, Borg M, Zhang X, Deacon CF, Horowitz M, Jones KL, Rayner CK (2016) A protein preload enhances the glucose-lowering efficacy of vildagliptin in type 2 diabetes. Diabetes Care 39:511–517
Ma J, Stevens JE, Cukier K, Maddox AF, Wishart JM, Jones KL, Clifton PM, Horowitz M, Rayner CK (2009) Effects of a protein preload on gastric emptying, glycemia, and gut hormones after a carbohydrate meal in diet-controlled type 2 diabetes. Diabetes Care 32:1600–1602
Lubransky A, Monro J, Mishra S, Yu H, Haszard JJ, Venn BJ (2018) Postprandial glycaemic, hormonal and satiety responses to rice and kiwifruit preloads in chinese adults: a randomised controlled crossover trial. Nutrients 10:1110
Lu J, Zhao W, Wang L, Fan Z, Zhu R, Wu Y, Zhou Y (2019) Apple preload halved the postprandial glycaemic response of rice meal on in healthy subjects. Nutrients 11:2912
Lu X, Lu J, Fan Z, Liu A, Zhao W, Wu Y, Zhu R (2021) Both isocarbohydrate and hypercarbohydrate fruit preloads curbed postprandial glycemic excursion in healthy subjects. Nutrients 13:2470
Zhao W, Zhou Y, Yuan Y, Fan Z, Wu Y, Liu A, Lu X (2020) Potato preload mitigated postprandial glycemic excursion in healthy subjects: an acute randomized trial. Nutrients 12:2759
Zhao W, Ye T, Fan Z, Wu Y, Liu A, Lu X (2021) Yam paste in glycemic preloads curbs peak glycemia of rice meals in apparent healthy subjects. Asia Pac J Clin Nutr 30:436–445
Saito Y, Nitta A, Imai S, Kajiyama S, Miyawaki T, Ozasa N, Kajiyama S, Hashimoto Y, Fukui M (2020) Tomato juice preload has a significant impact on postprandial glucose concentration in healthy women: a randomized cross-over trial. Asia Pac J Clin Nutr 29:491–497
Zhao W, Wang L, Fan Z, Lu J, Zhu R, Wu Y, Lu X (2020) Co-ingested vinegar-soaked or preloaded dried apple mitigated acute postprandial glycemia of rice meal in healthy subjects under equicarbohydrate conditions. Nutr Res 83:108–118
Lopez-Minguez J, Saxena R, Bandin C, Scheer FA, Garaulet M (2018) Late dinner impairs glucose tolerance in MTNR1B risk allele carriers: a randomized, cross-over study. Clin Nutr 37:1133–1140
Nakamura K, Tajiri E, Hatamoto Y, Ando T, Shimoda S, Yoshimura E (2021) Eating dinner early improves 24-h blood glucose levels and boosts lipid metabolism after breakfast the next day: a randomized cross-over trial. Nutrients 13:2424
Shea SA, Hilton MF, Orlova C, Ayers RT, Mantzoros CS (2005) Independent circadian and sleep/wake regulation of adipokines and glucose in humans. J Clin Endocrinol Metab 90:2537–2544
Saad A, Dalla MC, Nandy DK, Levine JA, Bharucha AE, Rizza RA, Basu R, Carter RE, Cobelli C, Kudva YC, Basu A (2012) Diurnal pattern to insulin secretion and insulin action in healthy individuals. Diabetes 61:2691–2700
Jamshed H, Beyl RA, Della MD, Yang ES, Ravussin E, Peterson CM (2019) Early time-restricted feeding improves 24-hour glucose levels and affects markers of the circadian clock, aging, and autophagy in humans. Nutrients 11:1234
Flint A, Raben A, Blundell JE, Astrup A (2000) Reproducibility, power and validity of visual analogue scares in assessment of appetite sensations in single test meal studies. Int J Obesity 24:38–48
Blundell J, de Graaf C, Hulshof T, Jebb S, Livingstone B, Lluch A, Mela D, Salah S, Schuring E, van der Knaap H, Westerterp M (2010) Appetite control: methodological aspects of the evaluation of foods. Obes Rev 11:251–270
Service FJ, Nelson RL (1980) Characteristics of glycemic stability. Diabetes Care 3:58–62
McDonnell CM, Donath SM, Vidmar SI, Werther GA, Cameron FJ (2005) A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol Ther 7:253–263
Wolever TM (2004) Effect of blood sampling schedule and method of calculating the area under the curve on validity and precision of glycaemic index values. Br J Nutr 91:295–301
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470
Mishra S, Edwards H, Hedderley D, Podd J, Monro J (2017) Kiwifruit non-sugar components reduce glycaemic response to co-ingested cereal in humans. Nutrients 9:1195
Wu T, Zhao BR, Bound MJ, Checklin HL, Bellon M, Little TJ, Young RL, Jones KL, Horowitz M, Rayner CK (2012) Effects of different sweet preloads on incretin hormone secretion, gastric emptying, and postprandial glycemia in healthy humans. Am J Clin Nutr 95:78–83
Akhavan T, Luhovyy BL, Panahi S, Kubant R, Brown PH, Anderson GH (2014) Mechanism of action of pre-meal consumption of whey protein on glycemic control in young adults. J Nutr Biochem 25:36–43
Wiedemann SJ, Rachid L, Illigens B, Böni-Schnetzler M, Donath MY (2020) Evidence for cephalic phase insulin release in humans: a systematic review and meta-analysis. Appetite 155:104792
Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A (2019) Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol 234:8152–8161
de Oliveira RC, Dos SPE, Camargo TM, Vinholes J, Rombaldi CV, Vizzotto M, Nora L (2019) Apple phenolic extracts strongly inhibit alpha-glucosidase activity. Plant Foods Hum Nutr 74:430–435
Hanhineva K, Torronen R, Bondia-Pons I, Pekkinen J, Kolehmainen M, Mykkanen H, Poutanen K (2010) Impact of dietary polyphenols on carbohydrate metabolism. Int J Mol Sci 11:1365–1402
Yu K, Ke MY, Li WH, Zhang SQ, Fang XC (2014) The impact of soluble dietary fibre on gastric emptying, postprandial blood glucose and insulin in patients with type 2 diabetes. Asia Pac J Clin Nutr 23:210–218
Choo VL, Viguiliouk E, Blanco MS, Cozma AI, Khan TA, Ha V, Wolever T, Leiter LA, Vuksan V, Kendall C, de Souza RJ, Jenkins D, Sievenpiper JL (2018) Food sources of fructose-containing sugars and glycaemic control: systematic review and meta-analysis of controlled intervention studies. BMJ 363:k4644
Petersen KF, Laurent D, Yu C, Cline GW, Shulman GI (2001) Stimulating effects of low-dose fructose on insulin-stimulated hepatic glycogen synthesis in humans. Diabetes 50:1263–1268
Geidl-Flueck B, Gerber PA (2017) Insights into the hexose liver metabolism-glucose versus fructose. Nutrients 9:1206
Cozma AI, Sievenpiper JL, de Souza RJ, Chiavaroli L, Ha V, Wang DD, Mirrahimi A, Yu ME, Carleton AJ, Di Buono M, Jenkins AL, Leiter LA, Wolever TM, Beyene J, Kendall CW, Jenkins DJ (2012) Effect of fructose on glycemic control in diabetes: a systematic review and meta-analysis of controlled feeding trials. Diabetes Care 35:1611–1620
Yajima T, Takahashi H, Yasuda K (2020) Comparison of interstitial fluid glucose levels obtained by continuous glucose monitoring and flash glucose monitoring in patients with type 2 diabetes mellitus undergoing hemodialysis. J Diabetes Sci Technol 14:1088–1094
Chlup R, Jelenova D, Kudlova P, Chlupova K, Bartek J, Zapletalova J, Langova K, Chlupova L (2006) Continuous glucose monitoring a novel approach to the determination of the glycaemic index of foods (DEGIF 1)—determination of the glycaemic index of foods by means of the CGMS. Exp Clin Endocr Diab 114:68–74
Morgan LM, Aspostolakou F, Wright J, Gama R (1999) Diurnal variations in peripheral insulin resistance and plasma non-esterified fatty acid concentrations: a possible link? Ann Clin Biochem 36(Pt 4):447–450
Malherbe C, Gasparo MD, Hertogh RD, Hoet JJ (1969) Circadian variations of blood sugar and plasma insulinlevels in man. Diabetologia 5:397
Nitta A, Imai S, Kajiyama S, Miyawaki T, Matsumoto S, Ozasa N, Kajiyama S, Hashimoto Y, Tanaka M, Fukui M (2019) Impact of different timing of consuming sweet snack on postprandial glucose excursions in healthy women. Diabetes Metab 45:369–374
Leung G, Huggins CE, Bonham MP (2019) Effect of meal timing on postprandial glucose responses to a low glycemic index meal: a crossover trial in healthy volunteers. Clin Nutr 38:465–471
Gu C, Brereton N, Schweitzer A, Cotter M, Duan D, Borsheim E, Wolfe RR, Pham LV, Polotsky VY, Jun JC (2020) Metabolic effects of late dinner in healthy volunteers-a randomized crossover clinical trial. J Clin Endocrinol Metab 105:2789
Pellegrini M, Cioffi I, Evangelista A, Ponzo V, Goitre I, Ciccone G, Ghigo E, Bo S (2020) Effects of time-restricted feeding on body weight and metabolism. A systematic review and meta-analysis. Rev Endocr Metab Disord 21:17–33
Xie Z, Sun Y, Ye Y, Hu D, Zhang H, He Z, Zhao H, Yang H, Mao Y (2022) Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nat Commun 13:1003
Bornet FR, Jardy-Gennetier AE, Jacquet N, Stowell J (2007) Glycaemic response to foods: impact on satiety and long-term weight regulation. Appetite 49:535–553
Clark MJ, Slavin JL (2013) The effect of fiber on satiety and food intake: a systematic review. J Am Coll Nutr 32:200–211
Scheer FA, Morris CJ, Shea SA (2013) The internal circadian clock increases hunger and appetite in the evening independent of food intake and other behaviors. Obesity (Silver Spring) 21:421–423
Sargent C, Zhou X, Matthews RW, Darwent D, Roach GD (2016) Daily rhythms of hunger and satiety in healthy men during one week of sleep restriction and circadian misalignment. Int J Environ Res Public Health 13:170
Acknowledgements
We sincerely thank all the volunteers who participated for their time and corporation.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
ZF and WZ formulated the research question. ZF, WZ and ZL designed the study. WZ, ZL, YW, AL, XL and XL carried out the research. WZ and ZL analyzed the data. WZ wrote the original draft and ZF revised the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of China Agricultural University (ethics number CAUHR-2021011) and registered on the Chinese Clinical Trial Registry (ChiCTR2100050541) on August 28th.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, W., Liu, Z., Fan, Z. et al. Apple preload increased postprandial insulin sensitivity of a high glycemic rice meal only at breakfast. Eur J Nutr 62, 1427–1439 (2023). https://doi.org/10.1007/s00394-022-03079-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-03079-4