Abstract
Purpose
Findings from few studies that investigated the relation between dietary behaviors and obesity are inconsistent. We aimed to assess the relation between patterns of dietary habits, identified by latent class analysis (LCA), and obesity in a large sample of Iranian adults.
Methods
In a cross-sectional study on 7958 adults, dietary behaviors were assessed in five domains (meal patterns, eating rate, intra-meal fluid intake, meal-to-sleep interval, and fatty foods intake) using a pretested questionnaire. LCA was applied to identify classes of diet-related practices. Anthropometric measures were assessed through the use of a validated self-reported questionnaire. General and abdominal obesity were defined as a body mass index ≥30 kg/m2, and a waist circumference ≥88 cm for women and ≥102 cm for men.
Results
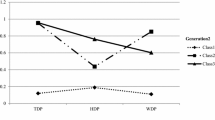
General and abdominal obesity were prevalent in 9.7 and 27.7 % of the study population, respectively. We identified three distinct classes of eating rates (moderate, moderate to slow, and moderate to fast), two classes of meal patterns (regular and irregular), two classes of intra-meal fluid intake (moderate and more intra-meal drinking), three classes of meal-to-sleep interval (short, moderate, and long meal-to-sleep interval), and three classes of fatty food intake (low to moderate, moderate to high, and low intake of fatty foods). After adjustment for potential confounders, individuals with ‘irregular meal pattern’ were 21, 24, and 22 % more likely to be overweight/obese, abdominally overweight/obese, and abdominally obese, compared with those who had a ‘regular meal pattern.’ Individuals with ‘more intra-meal drinking’ had greater odds of overweight (OR 1.37; 1.19–1.458) and obesity (OR 1.51; 1.16–1.97) than those with ‘moderate intra-meal drinking.’ Moderate-to-high intake of fatty foods was inversely associated with abdominally overweight/obese (OR 0.85; 0.73–1.00) and abdominally obesity (OR 0.80; 0.68–0.96) compared with ‘low-to-moderate intake of fatty foods.’ No significant association was observed between eating rate, meal-to-sleep interval, and general or abdominal obesity, after controlling for confounders.
Conclusion
Irregular meal pattern and more intra-meal drinking were associated with increased odds of general and abdominal obesity, whereas moderate-to-high intake of fatty foods was related to the decreased odds of central obesity among Iranian adults.

Similar content being viewed by others
References
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:1–253
Kolotkin RL, Meter K, Williams GR (2001) Quality of life and obesity. Obes Rev 2:219–229
Janghorbani M, Amini M, Willett WC et al (2007) First nationwide survey of prevalence of overweight, underweight, and abdominal obesity in Iranian adults. Obesity (Silver Spring) 15:2797–2808
Keller KL, Pietrobelli A, Faith MS (2003) Genetics of food intake and body composition: lessons from twin studies. Acta Diabetol 40:S95–S100
Popkin BM, Adair LS, Ng SW (2012) Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 70:3–21
Summerbell CD, Douthwaite W, Whittaker V et al (2009) The association between diet and physical activity and subsequent excess weight gain and obesity assessed at 5 years of age or older: a systematic review of the epidemiological evidence. Int J Obes (Lond) 33:S1–S92
Tanihara S, Imatoh T, Miyazaki M et al (2011) Retrospective longitudinal study on the relationship between 8-year weight change and current eating speed. Appetite 57:179–183
Galhardo J, Hunt LP, Lightman SL et al (2012) Normalizing eating behavior reduces body weight and improves gastrointestinal hormonal secretion in obese adolescents. J Clin Endocrinol Metab 97:E193–E201
Ohkuma T, Fujii H, Iwase M et al (2013) Impact of eating rate on obesity and cardiovascular risk factors according to glucose tolerance status: the Fukuoka Diabetes Registry and the Hisayama Study. Diabetologia 56:70–77
Ford AL, Bergh C, Sodersten P et al (2010) Treatment of childhood obesity by retraining eating behaviour: randomised controlled trial. BMJ 340:b5388
Ebbeling CB, Garcia-Lago E, Leidig MM, Seger-Shippee LG, Feldman HA, Ludwig DS (2007) Altering portion sizes and eating rate to attenuate gorging during a fast food meal: effects on energy intake. Pediatrics 119:869–875
Cleator J, Abbott J, Judd P, Sutton C, Wilding JP (2012) Night eating syndrome: implications for severe obesity. Nutr Diabetes 2:e44
Brewer EA, Kolotkin RL, Baird DD (2003) The relationship between eating behaviors and obesity in African American and Caucasian women. Eat Behav 4:159–171
Norton GN, Anderson AS, Hetherington MM (2006) Volume and variety: relative effects on food intake. Physiol Behav 87:714–722
Atkinson RL (1996) Role of nutrition planning in the treatment for obesity. Endocrinol Metab Clin North Am 25:955–964
Collins LM, Lanza ST (2010) Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. Wiley, Hoboken
Adibi P, Esmaillzadeh A, Hassanzadeh A et al (2012) The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): overview of methodology. J Res Med Sci 17:S292–S298
Third Report of the National Cholesterol Education Program (NCEP) (2002) Expert panel on detection, evaluation, and treatment of high blood cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106:3143–3421
Keshteli A, Esmaillzadeh A, Rajaie S, Askari G, Feinle-Bisset C, Adibi P (2014) A dish-based semi-quantitative food frequency questionnaire for assessment of dietary intakes in epidemiologic studies in Iran: design and development. Int J Prev Med 5:29–36
NICE (2006) Promoting and creating built or natural environments that encourage and support physcial activity: scope. National Institute for Health and Clinical Excellence, London
Hagenaars JAMAHJ, Mccutcheon AL (2002) Applied latent class analysis models. Cambridge University Press, Cambridge
Berg C, Lappas G, Wolk A et al (2009) Eating patterns and portion size associated with obesity in a Swedish population. Appetite 52:21–26
Marin-Guerrero AC, Gutierrez-Fisac JL, Guallar-Castillon P, Banegas JR, Rodriguez-Artalejo F (2008) Eating behaviours and obesity in the adult population of Spain. Br J Nutr 100:1142–1148
Nikpartow N, Danyliw AD, Whiting SJ, Lim H, Vatanparast H (2012) Fruit drink consumption is associated with overweight and obesity in Canadian women. Can J Public Health 103:178–182
Raat H, Struijk MK, Remmers T et al (2013) Primary prevention of overweight in preschool children, the BeeBOFT study (breastfeeding, breakfast daily, outside playing, few sweet drinks, less TV viewing): design of a cluster randomized controlled trial. BMC Public Health 13:974
Muckelbauer R, Sarganas G, Gruneis A, Muller-Nordhorn J (2013) Association between water consumption and body weight outcomes: a systematic review. Am J Clin Nutr 98:282–299
Pan A, Malik VS, Hao T, Willett WC, Mozaffarian D, Hu FB (2013) Changes in water and beverage intake and long-term weight changes: results from three prospective cohort studies. Int J Obes (Lond) 37:1378–1385
Hooper L, Abdelhamid A, Moore HJ, Douthwaite W, Skeaff CM, Summerbell CD (2012) Effect of reducing total fat intake on body weight: systematic review and meta-analysis of randomised controlled trials and cohort studies. BMJ 345:e7666
Labayen I, Ruiz JR, Ortega FB et al (2014) High fat diets are associated with higher abdominal adiposity regardless of physical activity in adolescents; the HELENA study. Clin Nutr 33:859–866
Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Bacskai K, Ross R (2008) Association between dietary fat intake, liver fat, and insulin sensitivity in sedentary, abdominally obese, older men. Appl Physiol Nutr Metab 33:239–245
Esmaillzadeh A, Mirmiran P, Azizi F (2005) Whole-grain consumption and the metabolic syndrome: a favorable association in Tehranian adults. Eur J Clin Nutr 59:353–362
Rajaie S, Azadbakht L, Khazaei M, Sherbafchi M, Esmaillzadeh A (2014) Moderate replacement of carbohydrates by dietary fats affects features of metabolic syndrome: a randomized crossover clinical trial. Nutrition 30:61–68
Blundell JE, MacDiarmid JI (1997) Fat as a risk factor for overconsumption: satiation, satiety, and patterns of eating. J Am Diet Assoc 97:S63–S69
Esmaillzadeh A, Keshteli AH, Feizi A, Zaribaf F, Feinle-Bisset C, Adibi P (2013) Patterns of diet-related practices and prevalence of gastro-esophageal reflux disease. Neurogastroenterol Motil 25:831-e638
Sasaki S, Katagiri A, Tsuji T, Shimoda T, Amano K (2003) Self-reported rate of eating correlates with body mass index in 18-y-old Japanese women. Int J Obes Relat Metab Disord 27:1405–1410
Acknowledgments
We wish to thank all staff of Isfahan University of Medical Sciences who kindly participated in our study and staff of Public Relations Unit, and other authorities of IUMS for their excellent cooperation. This study was supported by a grant from the Vice Chancellery for Research and Technology, Isfahan University of Medical Sciences, University of Medical Sciences, Islamic Republic of Iran. The financial support for conception, design, data analysis, and manuscript drafting comes from Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflict of interest
None of the authors had any personal or financial conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saneei, P., Esmaillzadeh, A., Keshteli, A.H. et al. Patterns of dietary habits in relation to obesity in Iranian adults. Eur J Nutr 55, 713–728 (2016). https://doi.org/10.1007/s00394-015-0891-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-0891-4