Abstract
Purpose
Assays of salivary biomarkers for diagnosis are gaining popularity in pediatric diseases due to their non-invasive nature. Our pilot project aims to evaluate the utility of salivary leucine-rich-alpha-2-glycoprotein (LRG) in the diagnosis of pediatric acute appendicitis (AA).
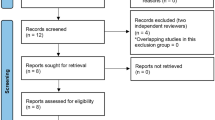
Methods
We prospectively recruited 34 patients, aged between 4 and 16 years, admitted with acute abdominal pain suspicious of appendicitis. The patients’ demography, clinical characteristics, laboratory investigations, imaging examination results, operative findings, and discharge diagnoses were recorded. We compared the diagnostic performance of the patients’ total white counts, neutrophil percentages, C-reactive protein, and saliva LRG levels. Saliva samples were obtained using the SalivaBio Children’s Swab and LRG levels were quantified using a commercially available LRG enzyme-linked immunosorbent assay (ELISA) kit. IRB approval was obtained.
Results
Seventeen patients had a confirmed diagnosis of appendicitis on histology. Another 17 were confirmed not to have appendicitis after a minimum of 24 h of hospitalization, with further verification via telephone interview 2 weeks later. The median levels of saliva LRG were elevated in patients with AA as compared to those without (P = 0.008). At a cutoff of LRG 0.33 ng/μg, we obtained a diagnostic specificity of 100% and sensitivity of 35.3%.
Conclusion
Our proof-of-concept study demonstrated the diagnostic potential of saliva LRG for appendicitis in children. The distinct advantage of saliva LRG assays is that the procedure is simple, pain-free, and requires no specialized skill. Further study with a larger cohort is needed to verify our results.

Similar content being viewed by others
References
Flum DR, Morris A, Koepsell T, Dellinger EP (2001) Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA 286:1748–1753
Bundy DG, Byerley JS, Liles EA, Perrin EM, Katznelson J, Rice HE (2007) Does this child have appendicitis? JAMA 298:438–451
Benabbas R, Hanna M, Shah J, Sinert R (2017) Diagnostic accuracy of history, physical examination, laboratory tests, and point-of-care ultrasound for pediatric acute appendicitis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med 24:523–551
Yu CW, Juan LI, Wu MH, Shen CJ, Wu JY, Lee CC (2013) Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br J Surg 100:322–332
Zhang H, Liao M, Chen J, Zhu D, Byanju S (2017) Ultrasound, computed tomography or magnetic resonance imaging—which is preferred for acute appendicitis in children? A meta-analysis. Pediatr Radiol 47:186–196
Naiditch JA, Lautz TB, Daley S, Pierce MC, Reynolds M (2013) The implications of missed opportunities to diagnose appendicitis in children. Acad Emerg Med 20:592–596
Kentsis A, Lin YY, Kurek K et al (2010) Discovery and validation of urine markers of acute pediatric appendicitis using high accuracy mass spectrometry. Ann Emerg Med 55:62–70
Kentsis A, Ahmed S, Kurek K, Brennan E, Bradwin G, Steen H, Bachur R (2012) Detection and diagnostic value of urine leucine-rich alpha-2-glycoprotein (LRG) in children with suspected acute appendicitis. Ann Emerg Med 60:78–83
Saito K, Tanaka T, Kanda H et al (2002) Gene expression profiling of mucosal addressin cell adhesion molecule-1+high endothelial venule cells (HEV) and identification of a leucine-rich HEV glycoprotein as a HEV marker. J Immunol 168:1050–1059
Kharbanda AB, Rai AJ, Cosme Y, Liu K, Dayan PS (2012) Novel serum and urine markers for pediatric appendicitis. Acad Emerg Med 19:56–62
Kulik DM, Uleryk EM, Maguire JL (2013) Does this child have appendicitis? A systematic review of clinical prediction rules for children with acute abdominal pain. J Clin Epidemiol 66:95–104
Samuel M (2002) Pediatric appendicitis score. J Pediatr Surg 37:877–881
Kelsey JL, Whittemore AS, Evans AS, Thompson WD (1996) Methods in observational epidemiology. Monographs in epidemiology and biostatistics, 2nd edn. Oxford University Press, New York
Fleiss JL, Levin B, Paik MC (2013) Statistical methods for rates and proportions, 3rd edn. Wiley, New Jersey
Castagnola M, Scarano E, Passali GC et al (2017) Salivary biomarkers and proteomics: future diagnostic and clinical utilities. Acta Otorhinolaryngol Ital 37:94–101
Hassaneen M, Maron JL (2017) Salivary diagnostics in pediatrics: applicability, translatability, and limitations. Front Public Health 5:83
Amado EM, Ferreira RP, Vitorino R (2013) One decade of salivary proteomics: current approaches and outstanding challenges. Clin Biochem 46:506–517
Romano-Keeler J, Wynn JL, Maron JL (2014) Great expectorations: the potential of salivary “Omic” approaches in neonatal intensive care. J Perinatol 34:169–173
Campo J, Perea MA, Del Romero J, Cano J, Hernando V, Bascones A (2006) Oral transmission of HIV, reality or fiction? An update. Oral Dis 12:219–228
Spielmann N, Wong DT (2011) Saliva: diagnostics and therapeutic perspectives. Oral Dis 17:345–354
Amado FM, Ferreira RP, Vitorino R (2013) One decade of salivary proteomics: current approaches and outstanding challenges. Clin Biochem 1(46):506–517
Cabras T, Pisano E, Mastinu A et al (2010) Alterations of the salivary secretory peptidome profile in children affected by type 1 diabetes. Mol Cell Proteomics 9:2099–2108
Cabras T, Pisano E, Montaldo C et al (2013) Significant modification of the salivary proteome potentially associated with complications of Down syndrome revealed by top-down proteomics. Mol Cell Proteomics 12:1844–1852
Abrao AL, Falcao DP, de Amorim RF et al (2016) Salivary proteomics: a new adjuvant approach to the early diagnosis of familial juvenile systemic lupus erythematosus. Med Hypothesis 89:97–100
Granger DA, Kivlighan KT, Fortunato C, Harmon AG, Hibel LC, Schwartz EB, Whembolua GL (2007) Integration of salivary biomarkers into developmental and behaviorally-oriented research: problems and solutions for collecting specimens. Physiol Behav 92:583–590
Hart RW, Mauk MG, Liu C et al (2011) Point-of-care oral-based diagnostics. Oral Dis 17:745–752
Salo M, Roth B, Stenstrom P, Arnbjornsson E, Ohlsson B (2016) Urinary biomarkers in pediatric appendicitis. Pediatr Surg Int 32:795–804
Acknowledgements
The authors gratefully acknowledge the support of Dr. Jennie Wong (Research Support Unit, Yong Loo Lin School of Medicine, National University of Singapore) for proof-reading and manuscript editing.
Funding
This research was supported by the SingHealth Foundation Research Grant 2015 (SHF/FG591P/2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no known conflicts of interest associated with this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yap, TL., Fan, J.D., Ho, M.F. et al. Salivary biomarker for acute appendicitis in children: a pilot study. Pediatr Surg Int 36, 621–627 (2020). https://doi.org/10.1007/s00383-020-04645-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04645-9