Abstract
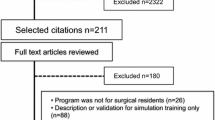
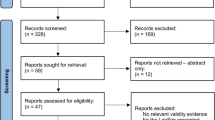
Purpose
The aim of this study was to identify (1) the type of skill evaluation methods and (2) how the effect of training was evaluated in simulation-based training (SBT) in pediatric surgery.
Methods
Databases of PubMed, Cochrane Library, and Web of Science were searched for articles published from January 2000 to January 2017. Search concepts of Medical Subject Heading terms were “surgery,” “pediatrics,” “simulation,” and “training, evaluation.”
Results
Of 5858 publications identified, 43 were included. Twenty papers described simulators as assessment tools used to evaluate technical skills. Reviewers differentiated between experts and trainees using a scoring system (45%) and/or a checklist (25%). Simulators as training tools were described in 23 papers. While the training’s effectiveness was measured using performance assessment scales (52%) and/or surveys (43%), no study investigated the improvement of the clinical outcomes after SBT.
Conclusion
Scoring, time, and motion analysis methods were used for the evaluation of basic techniques of laparoscopic skills. Only a few SBT in pediatric surgery have definite goals with clinical effect. Future research needs to demonstrate the educational effect of simulators as assessment or training tools on SBT in pediatric surgery.

Similar content being viewed by others
References
Dawe SR, Pena GN, Windsor JA, Broeders JAJL, Cregan PC, Hewett PJ et al (2014) Systematic review of skills transfer after surgical simulation-based training. Br J Surg 101:1063–1076. https://doi.org/10.1002/bjs.9482
Cheng A, Lang TR, Starr SR, Pusic M, Cook DA (2014) Technology-enhanced simulation and pediatric education: a meta-analysis. Pediatrics 133:e1313–e1323. https://doi.org/10.1542/peds.2013-2139
Barsness KA (2015) Trends in technical and team simulations: challenging the status Quo of surgical training. Semin Pediatr Surg 24:130–133. https://doi.org/10.1053/j.sempedsurg.2015.02.011
Patel EA, Aydın A, Desai A, Dasgupta P, Ahmed K (2018) Current status of simulation-based training in pediatric surgery: a systematic review. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2018.11.019
Accreditation Council for Graduate Medical Education (2016) ACGME program requirements for graduate medical education in the subspecialties of pediatrics. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/320S_pediatric_subs_2016.pdf. Accessed 11 Feb 2019
The Japanese Society of Pediatric Surgeons Website. https://www.jsps.gr.jp/about/rule_contents/rules. Accessed 11 Feb 2019
Kirkpatrick D (1996) Great ideas revisited. Techniques for evaluating training programs. Revisiting Kirkpatrick’s four-level model. Train Dev 50:54–59
Azzie G, Gerstle JT, Nasr A, Lasko D, Green J, Henao O et al (2011) Development and validation of a pediatric laparoscopic surgery simulator. J Pediatr Surg 46:897–903. https://doi.org/10.1016/j.jpedsurg.2011.02.026
Nasr A, Gerstle JT, Carrillo B, Azzie G (2013) The pediatric laparoscopic surgery (PLS) simulator: methodology and results of further validation. J Pediatr Surg 48:2075–2077. https://doi.org/10.1016/j.jpedsurg.2013.01.039
Hamilton JM, Kahol K, Vankipuram M, Ashby A, Notrica DM, Ferrara JJ (2011) Toward effective pediatric minimally invasive surgical simulation. J Pediatr Surg 46:138–144. https://doi.org/10.1016/j.jpedsurg.2010.09.078
Nasr A, Carrillo B, Gerstle JT, Azzie G (2014) Motion analysis in the pediatric laparoscopic surgery (PLS) simulator: validation and potential use in teaching and assessing surgical skills. J Pediatr Surg 49:791–794. https://doi.org/10.1016/j.jpedsurg.2014.02.063
Harada K, Takazawa S, Tsukuda Y, Ishimaru T, Sugita N, Iwanaka T et al (2014) Quantitative pediatric surgical skill assessment using a rapid-prototyped chest model. Minim Invasive Ther Allied Technol 24:226–232. https://doi.org/10.3109/13645706.2014.996161
Takazawa S, Ishimaru T, Harada K, Deie K, Fujishiro J, Sugita N et al (2016) Pediatric thoracoscopic surgical simulation using a rapid-prototyped chest model and motion sensors can better identify skilled surgeons than a conventional box trainer. J Laparoendosc Adv Surg Tech 26:740–747. https://doi.org/10.1089/lap.2016.0131
Retrosi G, Cundy T, Haddad M, Clarke S (2015) Motion analysis-based skills training and assessment in pediatric laparoscopy: construct, concurrent, and content validity for the eoSim simulator. J Laparoendosc Adv Surg Tech 25:944–950. https://doi.org/10.1089/lap.2015.0069
Trudeau MO, Carrillo B, Nasr A, Gerstle JT, Azzie G (2017) Educational role for an advanced suturing task in the pediatric laparoscopic surgery simulator. J Laparoendosc Adv Surg Tech 27:441–446. https://doi.org/10.1089/lap.2016.0516
Herbert GL, Cundy TP, Singh P, Retrosi G, Sodergren MH, Azzie G et al (2015) Validation of a pediatric single-port laparoscopic surgery simulator. J Pediatr Surg 50:1762–1766. https://doi.org/10.1016/j.jpedsurg.2015.03.057
Shepherd G, Delft D, Truck J, Kubiak R, Ashour K, Grant H (2015) A simple scoring system to train surgeons in basic laparoscopic skills. Pediatr Surg Int 32:245–252. https://doi.org/10.1007/s00383-015-3841-6
Ieiri S, Ishii H, Souzaki R, Uemura M, Tomikawa M, Matsuoka N et al (2013) Development of an objective endoscopic surgical skill assessment system for pediatric surgeons: suture ligature model of the crura of the diaphragm in infant fundoplication. Pediatr Surg Int 29:501–504. https://doi.org/10.1007/s00383-013-3276-x
Jimbo T, Ieiri S, Obata S, Uemura M, Souzaki R, Matsuoka N et al (2016) A new innovative laparoscopic fundoplication training simulator with a surgical skill validation system. Surg Endosc 31:1688–1696. https://doi.org/10.1007/s00464-016-5159-4
Usón-Casaús J, Pérez-Merino EM, Rivera-Barreno R, Rodríguez-Alarcón CA, Sánchez-Margallo FM (2014) Evaluation of a Bochdalek diaphragmatic hernia rabbit model for pediatric thoracoscopic training. J Laparoendosc Adv Surg Tech 24:280–285. https://doi.org/10.1089/lap.2013.0358
Obata S, Ieiri S, Uemura M, Jimbo T, Souzaki R, Matsuoka N et al (2015) An endoscopic surgical skill validation system for pediatric surgeons using a model of congenital diaphragmatic hernia repair. J Laparoendosc Adv Surg Tech 25:775–781. https://doi.org/10.1089/lap.2014.0259
Barsness KA, Rooney DM, Davis LM, Chin AC (2014) Validation of measures from a thoracoscopic esophageal atresia/tracheoesophageal fistula repair simulator. J Pediatr Surg 49:29–33. https://doi.org/10.1016/j.jpedsurg.2013.09.069
Takazawa S, Ishimaru T, Harada K, Tsukuda Y, Sugita N, Mitsuishi M et al (2015) Video-based skill assessment of endoscopic suturing in a pediatric chest model and a box trainer. J Laparoendosc Adv Surg Tech 25:445–453. https://doi.org/10.1089/lap.2014.0269
Maricic MA, Bailez MM, Rodriguez SP (2016) Validation of an inanimate low cost model for training minimal invasive surgery (MIS) of esophageal atresia with tracheoesophageal fistula (AE/TEF) repair. J Pediatr Surg 51:1429–1435. https://doi.org/10.1016/j.jpedsurg.2016.04.018
Deie K, Ishimaru T, Takazawa S, Harada K, Sugita N, Mitsuishi M et al (2017) Preliminary study of video-based pediatric endoscopic surgical skill assessment using a neonatal esophageal atresia/tracheoesophageal fistula model. J Laparoendosc Adv Surg Tech 27:76–81. https://doi.org/10.1089/lap.2016.0214
Barber SR, Kozin ED, Dedmon M, Lin BM, Lee K, Sinha S et al (2016) 3D-printed pediatric endoscopic ear surgery simulator for surgical training. Int J Pediatr Otorhinolaryngol 90:113–118. https://doi.org/10.1016/j.ijporl.2016.08.027
Weinstock P, Rehder R, Prabhu SP, Forbes PW, Roussin CJ, Cohen AR (2017) Creation of a novel simulator for minimally invasive neurosurgery: fusion of 3D printing and special effects. J Neurosurg Pediatr 20:1–9. https://doi.org/10.3171/2017.1.PEDS16568
Nakajima K, Wasa M, Takiguchi S, Taniguchi E, Soh H, Ohashi S et al (2003) A modular laparoscopic training program for pediatric surgeons. JSLS 7:33–37
Ieiri S, Nakatsuji T, Higashi M, Akiyoshi J, Uemura M, Konishi K et al (2010) Effectiveness of basic endoscopic surgical skill training for pediatric surgeons. Pediatr Surg Int 26:947–954. https://doi.org/10.1007/s00383-010-2665-7
Pérez-Duarte FJ, Díaz-Güemes I, Sánchez-Hurtado MA, Cano Novillo I, Berchi García FJ, García Vázquez A et al (2012) Design and validation of a training model on paediatric and neonatal surgery. Cir Pediatr 25:121–125
Jimbo T, Ieiri S, Obata S, Uemura M, Souzaki R, Matsuoka N et al (2015) Effectiveness of short-term endoscopic surgical skill training for young pediatric surgeons: a validation study using the laparoscopic fundoplication simulator. Pediatr Surg Int 31:963–969. https://doi.org/10.1007/s00383-015-3776-y
Deutsh ES (2008) High-fidelity patient simulation mannequins to facilitate aerodigestive endoscopy training. Arch Otolaryngol Head Neck Surg 134:625–629. https://doi.org/10.1001/archotol.134.6.625
Binstadt E, Donner S, Nelson J, Flottemesch T, Hegarty C (2008) Simulator training improves fiber-optic intubation proficiency among emergency medicine residents. Acad Emerg Med 15:1211–1214. https://doi.org/10.1111/j.1553-2712.2008.00199.x
Jabbour N, Reihsen T, Sweet RM, Sidman JD (2011) Psychomotor skills training in pediatric airway endoscopy simulation. Otolaryngol Head Neck Surg 145:43–50. https://doi.org/10.1177/0194599811403379
Griffin GR, Hoesli R, Thorne MC (2017) Validity and efficacy of a pediatric airway foreign body training course in resident education. Ann Otol Rhinol Laryngol 120:635–640. https://doi.org/10.1177/000348941112001002
Deutsch ES, Christenson T, Curry J, Hossain J, PhD Zur K et al (2009) Multimodality education for airway endoscopy skill development. Ann Otol Rhinol Laryngol 118:81–86
Dabbas N, Muktar Z, Ade-Ajayi N (2009) GABBY: an ex vivo model for learning and refining the technique of preformed silo application in the management of gastroschisis. Afr J Paediatr Surg 6:73–76. https://doi.org/10.4103/0189-6725.54766
Tugnoli G, Ribaldi S, Casali M, Calderale SM, Coletti M, Villani S et al (2007) The education of the trauma surgeon: the "trauma surgery course" as advanced didactic tool. Ann Ital Chir 78:39–44
Lehner M, Heimberg E, Hoffmann F, Heinzel O, Kirschner H-J, Heinrich M (2017) Evaluation of a pilot project to introduce simulation-based team training to pediatric surgery trauma room care. Int J Pediatr 2017:1–6. https://doi.org/10.1155/2017/9732316
Nishisaki A Scrattish L Boulet J Kalsi M Maltese M Castner T et al (2008) Effect of recent refresher training on in situ simulated pediatric tracheal intubation psychomotor skill performance. In: Henriksen K Battles JB Keyes MA et al (eds) Advances in patient safety: new directions and alternative approaches (vol. 3: performance and tools). Agency for Healthcare Research and Quality (US), Rockville
Reid J, Stone K, Brown J, Caglar D, Kobayashi A, Lewis-Newby M et al (2012) The Simulation Team Assessment Tool (STAT): development, reliability and validation. Resuscitation 83:879–886. https://doi.org/10.1016/j.resuscitation.2011.12.012
Nishisaki A, Hales R, Biagas K, Cheifetz I, Corriveau C, Garber N et al (2009) A multi-institutional high-fidelity simulation “boot camp” orientation and training program for firstyear pediatric critical care fellows. Pediatr Crit Care Med 10:157–162. https://doi.org/10.1097/PCC.0b013e3181956d29
Cheng A, Goldman RD, Aish MA, Kissoon N (2010) A simulation-based acute care curriculum for pediatric emergency medicine fellowship training programs. Pediatr Emerg Care 26:475–476. https://doi.org/10.1097/PEC.0b013e3181e5841b
Stone K, Reid J, Caglar D, Christensen A, Strelitz B, Zhou L, Quan L (2014) Increasing pediatric resident simulated resuscitation performance: a standardized simulation-based curriculum. Resuscitation 85:1099–1105. https://doi.org/10.1016/j.resuscitation.2014.05.005
Atamanyuk I, Ghez O, Saeed I, Lane M, Hall J, Jackson T et al (2013) Impact of an open-chest extracorporeal membrane oxygenation model for in situ simulated team training: a pilot study. Interact Cardiovasc Thorac Surg 18:17–20. https://doi.org/10.1093/icvts/ivt437
Allan CK, Pigula F, Bacha EA, Emani S, Fynn-Thompson F, Thiagarajan RR et al (2013) An extracorporeal membrane oxygenation cannulation curriculum featuring a novel integrated skills trainer leads to improved performance among pediatric cardiac surgery trainees. Simul Healthc 8:221–228. https://doi.org/10.1097/SIH.0b013e31828b4179
Brydges R, Farhat WA, El-Hout Y, Dubrowski A (2010) Pediatric urology training: performance-based assessment using the fundamentals of laparoscopic surgery. J Surg Res 161:240–245. https://doi.org/10.1016/j.jss.2008.12.041
Soltani T, Hidas G, Kelly MS, Kaplan A, Selby B, Billimek J et al (2016) Endoscopic correction of vesicoureteral reflux simulator curriculum as an effective teaching tool: pilot study. J Pediatr Urol 12:45.e1–45.e6. https://doi.org/10.1016/j.jpurol.2015.06.017
Peeters SHP, Akkermans J, Slaghekke F, Bustraan J, Lopriore E, Haak MC et al (2015) Simulator training in fetoscopic laser surgery for twin-twin transfusion syndrome: a pilot randomized controlled trial. Ultrasound Obstet Gynecol 46:319–326. https://doi.org/10.1002/uog.14916
Yoo SJY, Spray T, Austion EH, Yun TJ, van Arsdell GS (2017) Hands-on surgical training of congenital heart surgery using 3-dimensional print models. J Thorac Cardiovasc Surg 153:1530–1540. https://doi.org/10.1016/j.jtcvs.2016.12.054
Holmboe ES, Sherbino J, Long DM, Swing SR, Frank JR, For the International CBME Collaborators (2010) The role of assessment in competency-based medical education. Med Teach 32:676–682. https://doi.org/10.3109/0142159X.2010.500704
Fried GM, Feldman LS (2007) Objective assessment of technical performance. World J Surg 32:156–160. https://doi.org/10.1007/s00268-007-9143-y
Jones DB, Schwaitzberg SD (2019) Operative endoscopic and minimally invasive surgery, 1st edn. CRC Press, Boca Raton, pp 184–187
Farcas MA, Trudeau MO, Nasr A, Gerstle JT, Carrillo B, Azzie G (2016) Analysis of motion in laparoscopy: the deconstruction of an intra- corporeal suturing task. Surg Endosc 31:3130–3139. https://doi.org/10.1007/s00464-016-5337-4
Cecilio-Fernandes D, Cnossen F, Jaarsma DADC, Tio RA (2018) Avoiding surgical skill decay a systematic review on the spacing of training sessions. J Surg Educ 75:471–480. https://doi.org/10.1016/j.jsurg.2017.08.002
Cox T, Seymour N, Stefanidis D (2015) Moving the needle: simulation’s impact on patient outcomes. Surg Clin N Am 95:827–838. https://doi.org/10.1016/j.suc.2015.03.005
Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG et al (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair. Ann Surg 254:502–509. https://doi.org/10.1097/SLA.0b013e31822c6994 (discussion 509–11)
Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondré K, Stanbridge D et al (2005) A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg 190:107–113
Kurashima Y, Feldman LS, Al-Sabah S, Kaneva PA, Fried GM, Vassiliou MC (2011) A tool for training and evaluation of laparoscopic inguinal hernia repair: the Global Operative Assessment of Laparoscopic Skills-Groin Hernia (GOALS-GH). Am J Surg 201:54–61. https://doi.org/10.1016/j.amjsurg.2010.09.006
Ghaderi I, Manji F, Park YS, Juul D, Ott M, Harris I et al (2015) Technical skills assessment toolbox. Ann Surg 261:251–262. https://doi.org/10.1097/SLA.0000000000000520
Oue T, Kubota A, Okuyama H, Kawahara H (2005) Laparoscopic percutaneous extraperitoneal closure (LPEC) method for the exploration and treatment of inguinal hernia in girls. Pediatr Surg Int 21:964–968. https://doi.org/10.1007/s00383-005-1556-9
Acknowledgements
This research received no specific grant from any funding agency in the public and commercial sectors.
Funding
This study was not funded by any grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest for this study.
Ethical approval
Not applicable, since the study is a systematic review.
Informed consent
Not applicable, since the study is a systematic review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yokoyama, S., Mizunuma, K., Kurashima, Y. et al. Evaluation methods and impact of simulation-based training in pediatric surgery: a systematic review. Pediatr Surg Int 35, 1085–1094 (2019). https://doi.org/10.1007/s00383-019-04539-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-019-04539-5