Abstract
Purpose
RALP is rapidly becoming the new gold standard treatment for UPJO in children, who suffer from uretero-pelvic obstruction (UPJO). However, presently there is a lack of data regarding the outcomes of RALP in young infants and smaller children. This study aims to compare the outcomes of RALP in children weighing less than 10 kg and matched with an analogous cohort who underwent open pyeloplasty (OP).
Methods
We prospectively compared patients who underwent RALP to a matched cohort of patients who underwent OP from our retrospectively acquired data registry. Comparative outcomes included: Demographics, success rate, complications, and length of hospital stay, postoperative pain score and failure rate. Failure was defined as the need for a secondary intervention for UPJO, or worsening hydronephrosis during follow-up.
Results
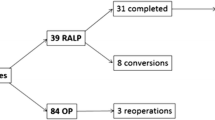
A total of 15 patients with a median age of 8 months (range 5–11 months) and median weight 7 kg (range 5.6–9.8 kg) underwent RALP between 2016 and 2018, a matched cohort of 15 children who underwent OP similar in terms of age, weight, gender and affected side between 2014 and 2016. All children had prenatal diagnosis of hydronephrosis and underwent surgery utilizing combined general and regional (Caudal MO) anesthesia. Intrinsic obstruction was present in 13 of RALP group (86.7%) and in 14 in OP group (93.3%). Mean operative time was 67.8 + 13.4 min in RALP group, while 66.5 + 9.5 min in OP group. (p = 0.76) All but two patients in RALP group had stent inserted and required subsequent anesthesia for stent removal, while all OP children had a Salle Pyeloplasty stent inserted during the procedure and underwent removal in an ambulatory setting without the need for anesthesia. There were no failures recorded in the RALP group, while one patient in OP required a secondary intervention. Mean hospital stay was 1 day (1–2 days) for RALP and 2 days (2–3 days) for OP. There was no difference in FLACC Pain Scale in both groups. Clavien–Dindo grade I–II complications occurred in one patient from each group. Two patients from RALP underwent subsequent ureteral reimplantation due to accompanying uretero-vescical junction obstruction.
Conclusions
Our data suggest that RALP can be performed safely in pediatric patients weighing less than 10 kg. with similar outcomes when compared to patients undergoing an open procedure for the same pathology.



Similar content being viewed by others
References
Tripp BM, Homsy YL (1995) Neonatal hydronephrosis-the controversy and the management. Pediatr Nephrol 9:503–509
Elder JS (1997) Antenatal hydronephrosis. Fetal and neonatal management. Pediatr Clin North Am 44:1299–1321
Chertin B, Pollack A, Koulikov D et al (2006) Conservative treatment of uretero-pelvic junction obstruction in children with antenatal diagnosis of hydronephrosis: lessons learned after 16 years of follow up. Eur Urol 49(4):734–739
Anderson JC, Hynes W (1949) Retrocaval ureter; a case diagnosed pre-operatively and treated successfully by a plastic operation. Br J Urol 21(3):209–214
O’Reilly PH, Brooman PJ, Mak S, Jones M, Pickup C, Atkinson C et al (2001) The long-term results of Anderson-Hynes pyeloplasty. BJU Int 87(4):287–289
Tan BJ, Rastinehad AR, Marcovich R, Smith AD, Lee BR (2005) Trends in ureteropelvic junction obstruction management among urologists in the United States. Urology 65:260–264
Peters CA (2011) Pediatric robot-assisted pyeloplasty. J Endourol Endourol Soc 25(2):179–185
Sorensen MD, Delostrinos C, Johnson MH, Grady RW, Lendvay TS (2011) Comparison of the learning curve and outcomes of robotic assisted pediatric pyeloplasty. J Urol 185(6 Suppl):2517–2522
Freilich DA, Penna FJ, Nelson CP, Retik AB, Nguyen HT (2010) Parental satisfaction after open versus robot assisted laparoscopic pyeloplasty: results from modified Glasgow Children’s Benefit Inventory Survey. J Urol 183(2):704–8040
Chertin B, Zeldin A, Kocherov S, Ioscovich A, Ostrovsky IA, Gozal Y (2016) Use of caudal analgesia supplemented with low dose of morphine in children who undergo renal surgery. Curr Urol 9(3):132–137
Minnillo BJ, Cruz JAS, Sayao RH et al (2011) Long-term experience and outcomes of robotic assisted laparoscopic pyeloplasty in children and young adults. J Urol 185:1455–1460
Dangle PP, Kearns J, Anderson B, Gundeti MS (2013) Outcomes of infants undergoing robot-assisted laparoscopic pyeloplasty compared to open repair. J Urol 190(6):2221–2224
Valla JS, Breaud J, Griffin SJ, Sautot-Vial N, Beretta F, Guana R et al (2009) Retroperitoneoscopic vs open dismembered pyeloplasty for ureteropelvic junction obstruction in children. J Pediatr Urol 5(5):368–373
Van der Toorn F, van den Hoek J, Wolffenbuttel KP, Scheepe JR (2013) Laparoscopic transperitoneal pyeloplasty in children from age of 3 years: our clinical outcomes compared with open surgery. J Pediatr Urol 9(2):161–168
Cundy TP, Shetty K, Clark J, Chang TP, Sriskandarajah K, Gattas NE et al (2013) The first decade of robotic surgery in children. J Pediatr Surg 48(4):858–865
Lee RS, Retik AB, Borer JG, Peters CA (2006) Pediatric robot assisted laparoscopic dismembered pyeloplasty: comparison with a cohort of open surgery. J Urol 175(2):683–687
Avery DI, Herbst KW, Lendvay TS et al (2015) Robot-assisted laparoscopic pyeloplasty: multi-institutional experience in infants. J Pediatr Urol 11(139):e1–e139.e5
Lucas SM, Sundaram CP, Wolf JS Jr, Leveillee RJ, Bird VG, Aziz M et al (2012) Factors that impact the outcome of minimally invasive pyeloplasty: results of the multi-institutional laparoscopic and robotic pyeloplasty collaborative group. J Urol 187(2):522–527
Richter S, Ringel A, Shalev M, Nissenkorn I (2000) The indwelling ureteric stent: a “friendly” procedure with unfriendly high morbidity. BJU Int 85:408–411
Joshi HB, Stainthrope A, MacDonagh RP, Keeley FX Jr, Timoney AG, Barry MJ (2003) Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol 169:1065–1069
Silva MV, Levy AC, Finkelstein JB et al (2015) Is peri-operative urethral catheter drainage enough? The case for stentless pediatric robotic pyeloplasty. J Pediatr Urol 11(175):e1–e5
Rodriguez AR, Rich MA, Swana HS (2012) Stentless pediatric robotic pyeloplasty. Adv Urol 4(2):57–60
Smith KE, Holmes N, Lieb JI et al (2002) Stented versus nonstented pediatric pyeloplasty: a modern series and review of the literature. J Urol 168:1127–1130
Elmalik K, Chowdhury MM, Capps SN (2008) Ureteric stents in pyeloplasty: a help or a hindrance? J Pediatr Urol 4:275–279
Lee LC, Kanaroglou N, Gleason JM et al (2015) Impact of drainage technique on pediatric pyeloplasty: comparative analysis of externalized uretero-pyelostomy versus double-J internal stents. Can Urol Assoc J 9:453–457
Barbosa JABA, Barayan G, Gridley CM et al (2013) Parent and patient perceptions of robotic vs open urological surgery scars in children. J Urol 190:244–250
Boysen WR, Gundeti MS (2017) Robot-assisted laparoscopic pyeloplasty in the pediatric population: a review of technique, outcomes, complications, and special considerations in infants. Pediatr Surg Int 33(9):925–935
Funding
This study did not receive any financial funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent regarding the surgical procedure was obtained from the parents of all individual participants included in the study.
Conflict of interest
The authors have no conflict of the interest with the discussion in the paper and we have nothing to disclose concerning this manuscript.
Rights and permissions
About this article
Cite this article
Kafka, I.Z., Kocherov, S., Jaber, J. et al. Pediatric robotic-assisted laparoscopic pyeloplasty (RALP): does weight matter?. Pediatr Surg Int 35, 391–396 (2019). https://doi.org/10.1007/s00383-019-04435-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-019-04435-y