Abstract
Purpose
To review the outcomes of extremely low birth weight (ELBW, <1000 g) infants with esophageal atresia/tracheoesophageal fistula (EA/TEF).
Methods
Health records of ELBW EA/TEF infants treated at our institution from 2000 to 2014 were reviewed (REB1000046653). Demographics, operative approach and postoperative complications were analyzed. Data are reported as median (range).
Results
Of 268 EA/TEF infants, 8 (3 %, five females) were ELBW (930 g, 540–995). Gestational age was 28 weeks (23–32). Seven had type-C EA/TEF and one type B.
Outcomes
One trisomy 18 infant received no treatment and died; one initially diagnosed as type A had primary repair at 126 days of life (DOL); six underwent TEF ligation (three trans-pleural) with primary repair in one and delayed anastomosis in two (DOL 120 and 178). The remaining three died (gastrostomy dehiscence and peritonitis, liver hemorrhage during peritoneal drain insertion, severe chronic lung disease and brain hemorrhages). At a median follow-up of 3 years (range 15 months–5 years), all survivors are thriving.
Conclusion
ELBW infants with EA/TEF are rare and result in high morbidity and mortality. Mortality is mainly related to complications not associated with EA/TEF repair. Fistula ligation followed by delayed anastomosis seems to achieve a better outcome in ELBW infants.
Similar content being viewed by others
Introduction
Recent advances in the perinatal treatment of preterm infants, including prenatal referral to tertiary care centers, prenatal steroid treatment, and postnatal assisted ventilation and surfactant therapy, have resulted in improved survival rates for very low birth weight (VLBW, <1500 g) and extremely low birth weight (ELBW, <1000 g) neonates [1–5]. Simultaneously, neonatal surgical mortality has steadily fallen over the last decades, thanks to the improvement in pediatric anesthesia, better understanding of neonatal physiology, and advances in intensive care including mechanical ventilation and parenteral nutrition management [6].
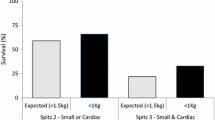
In infants with esophageal atresia/tracheoesophageal fistula (EA/TEF), birth weight has consistently been reported as a significant determinant of overall survival [7]. In 1962, Waterston et al. from Great Ormond Street reported the outcomes of 218 infants born with EA/TEF and proposed a prognostic classification based on birth weight, associated anomalies and pneumonia [8]. In that study, the lowest rates of survival were in infants with birth weights less than 4 lb (1800 g). In 1994, Spitz et al. updated the prognostic classification after reviewing 372 infants with EA/TEF, with the lowest survival rates in infants with major cardiac anomalies and birth weights less than 1500 g [9]. More recently, other groups reviewing smaller series of EA/TEF patients have proposed modifications of these classifications with birth weight becoming a less significant determinant for survival compared to the Waterston and Spitz series [10–13]. Poenaru et al. reported that birth weight was not found to independently influence mortality in their series of 96 patients and proposed a novel “Montreal classification”, based on two other prognostic factors, pre-operative ventilator dependence and associated anomalies [14]. Similarly, Choudhury et al. reported that associated cardiac and chromosomal anomalies were more significant causes of death than birth weight [11]. Conversely, a more recent Japanese study analyzing the outcome of EA/TEF infants treated over 25 years reported a modification of the Spitz classification where birth weight of less than 2000 g and major cardiac anomalies were still considered crucial factors for survival [15]. However, these studies propose new classifications based on relatively small cohorts of patients accrued over a very long period of review during which many facets of neonatal care have changed or improved [11, 14, 15].
Despite these reports, the management of VLBW and ELBW infants with EA/TEF still remains challenging and controversial. The aim of the present study was to review our experience with the surgical management of these infants at our institution over a 15-year period.
Methods
Ethical approval was obtained (REB1000046653). Medical records of ELBW infants with EA/TEF treated at our institution between 2000 and 2014 were reviewed. Demographics, associated anomalies, operative approach and postoperative complications were reported. Data are reported as median (range).
Results
Demographics
Of the 268 infants with EA/TEF managed at our institution during the study period, 8 (3 %) had a median birth weight of 930 g (range 540–995) with a median gestational age of 28 weeks (range 23–32) (Table 1) and a female preponderance (M:F = 3:5). Seven infants had type-C EA/TEF (87.5 %) and one had a type B. Associated anomalies were present in all infants (Table 1).
Surgery
A patient born with dysmorphic features (triangular facies, low set hypoplastic ears, clenched hands, rocker bottom feet, short sternum) had genetic confirmation of trisomy 18 (G-banding analysis), did not undergo any surgery due to severe cardiopulmonary instability and was palliated on day 2 of life (Fig. 1).
Of the remaining seven patients who underwent surgical repair, six with type-C EA/TEF underwent TEF ligation (trans-pleural in three) on day 1 of life (range 1–5). Primary anastomosis at the time of TEF ligation was performed in only one of those six patients who also underwent a loop colostomy for associated anorectal malformation. Delayed esophageal anastomosis was carried out in two patients at 120 and 178 days of life, respectively. The remaining three patients died. One of those was born with associated duodenal atresia (annular pancreas), omphalomesenteric duct remnant with local volvulus, and anorectal malformation, at the same time of TEF ligation underwent laparotomy with bowel resection, gastrostomy and ileostomy. The postoperative course was complicated by gastrostomy dehiscence and peritonitis, bilateral intraventricular hemorrhage and care was withdrawn on day 21 of life. Another patient died on day 16 of life when during cardiac surgery procedure for truncus arteriosus the infant developed fatal liver hemorrhage caused by the insertion of a peritoneal drain. The third patient, who had undergone TEF ligation on day 1 of life, underwent a second thoracotomy on day 5 due to persistent pneumothorax where a recurrent TEF was excluded and esophageal anastomosis was carried out. Post-operatively, this infant developed recurrent bilateral pneumothoraces requiring multiple drain insertions, severe chronic lung disease requiring maximal ventilator support and oxygen therapy, and multiple cerebellar and brain hemorrhages for which parents opted for comfort care. The child died at 7 weeks of age.
The seventh patient was born at 23 + 2 weeks of gestation with a birth weight of 620 g. He initially underwent bronchoscopy that ruled out the presence of any TEF, was considered as having a pure EA and had an open Stamm gastrostomy on day 61 of life. However, at definitive surgery on day 126 of life, he was found to have a proximal TEF (type B) and underwent TEF ligation and esophageal anastomosis. Moreover, due to severe tracheomalacia, this patient underwent an open aortopexy on day 217 of life.
No patients in this series underwent thoracoscopic TEF ligation or esophageal repair.
Outcome
Overall mortality was 50 %. All four surviving patients experienced postoperative complications. One patient had a thoracic duct injury that was successfully treated conservatively. Two (50 %) patients had anastomotic leak that was successfully managed non-operatively with antibiotic and chest tube drainage. Three patients (75 %) developed esophageal strictures requiring balloon dilatation. One patient had severe tracheomalacia requiring aortopexy after esophageal repair.
All survivors suffered from prematurity-related complications including chronic lung disease and severe pulmonary hypertension (n = 2), retinopathy (n = 2), hyperinsulinemic hypoglycemia attributed to the small size for gestational age (n = 1), osteopenia (n = 1) and sepsis (n = 3).
At a median follow-up of 3 years (range 15 months–5 years), all four survivors are thriving. Three of them are on full oral feeds, whereas one is still dependent on gastrostomy feeds. This latter patient also underwent a Nissen fundoplication at 13 months of age due to severe gastro-esophageal reflux. One patient, who developed congenital disseminated fungal infection with brain lesions during the first admission, suffers from significant neurodevelopmental delay with spastic cerebral palsy.
Discussion
The current series of ELBW infants with EA/TEF is one of the largest reported in the literature. Although the number of ELBW infants who are born with EA/TEF is low, accounting for only 3 % of all newborns with EA/TEF, they experience a very high rate of morbidity and mortality, most of which are secondary to their prematurity in addition to associated congenital anomalies. This reflects the low survival rates reported in the literature for ELBW infants in general without EA/TEF [16–20]. In the present series, infants with ELBW and EA/TEF have a 50 % survival rate. This is much lower than the survival rate recently reported by our institution (91 % at 3 years) [21].
Prenatal ultrasonography in this series of patients was not very informative: scans were normal in two fetuses, showed polyhydramnios in two and were aspecific in the other four. Prenatal diagnosis rate of EA using ultrasonography can be low in the first trimester, but may become more accurate later in the pregnancy when other features, such as a small stomach bubble or a dilated blind-ending esophageal pouch, are visualized [22, 23]. Given the prematurity rate of this series of patients, most had just initial prenatal scans which would explain the low yield of ultrasonography.
All infants in our series had associated anomalies, consistent with previous reports [24, 25]. In particular, cardiac anomalies are the most frequent and found in all patients in our series. Two patients (25 %) had chromosomal anomalies. One was born with trisomy 18. This is a known association with EA/TEF, which has a 1-year survival rate as low as 17–27 % in those receiving surgical repair [26]. This clinical picture poses ethical problems regarding the management of these infants, but given the extremely poor prognosis, once the diagnosis has been confirmed on chromosomal analysis and parents have been counseled, no further surgical treatment may be justified [27]. One patient was born with a mosaic trisomy 14, a very rare chromosome disorder which, to the best of our knowledge, has never been reported in association with EA/TEF. Patients with mosaic trisomy 14 have growth and psychomotor retardation, dysmorphic facial features, congenital heart disease and cryptorchidism [28]. The life expectancy of these patients has not been studied, but about two-thirds of patients with trisomy 14 mosaicism survive relatively free of serious medical problems after infancy [28]. Therefore, an attempt to treat this infant was made, but the eventual outcome was poor.
The surgical approach to infants with ELBW and EA/TEF is variable and should be individualized. One option is to perform a TEF ligation, possibly combined with a feeding gastrostomy, postponing esophageal repair until the infant is older and of bigger weight. The other option is to carry out an immediate TEF ligation and esophageal anastomosis. In either case, it is crucial to ligate the TEF promptly, because it poses the risk of aspiration and death if left untreated [7]. Preterm infants with severe respiratory distress syndrome will invariably require positive pressure ventilatory support which may initiate a deadly cascade of severe gastric distension, further worsening of ventilation with possible gastric rupture resulting in tension pneumoperitoneum [29]. This risk is even higher in those neonates with associated intestinal atresia or anorectal malformation. For this reason, emergency ligation of the TEF has been advocated for these infants since 1984 [30, 31]. In some of these cases, TEF ligation results in such a dramatic improvement of the infant respiratory status after which primary esophageal repair can safely proceed [7]. This occurred in one of our patients, who was sufficiently stabilized after TEF ligation to undergo esophageal repair.
In non-emergency cases, the timing of esophageal anastomosis in ELBW infants is controversial. Seitz et al. reported a series of four patients, three with ELBW and one with VLBW, where primary repair and TEF closure were achievable and concluded that staged repair should be considered only in patients with associated severe malformations [24]. Conversely, Petrosyan et al. analyzing a larger series of 25 premature infants with VLBW reported that staged esophageal repair results in a lower rate of anastomotic complications and overall morbidity than primary repair [25]. In this series that analyzes the outcomes of “heavier” patients (number of ELBW not reported), infants repaired primarily had higher stricture and leak rates [25].
The strategy we adopted at our institution was to delay the esophageal anastomosis, unless the patient was so stable to sustain it. Of our four survivors, three had a delayed anastomosis and one a primary repair. The three patients who died were all managed with TEF ligation with a plan for delayed anastomosis. However, none of these mortality cases were due to delay in definitive repair or to complications related to the initial esophageal surgery. In two of these patients, the decision for discontinuation of active treatment, in agreement with the family, was based on the very poor neurological outcomes secondary to bilateral intraventricular hemorrhage in one and multiple cerebellar and brain hemorrhage in the other. The surgical complications typical of patients with EA/TEF, including thoracic duct injury and anastomotic leak and/or stricture, were successfully treated. Likewise, tracheomalacia and gastro-esophageal reflux, conditions known to be associated with EA/TEF, were successfully managed. Finally, all survivors but one, who has the shortest follow-up, are on full oral feeds.
It must not be underestimated that, regardless of the surgical approach, these infants suffer from all of the complications of prematurity. In fact, all survivors in this series had severe morbidity related to their early gestational age. Our series stratified according to the international classification of prematurity was composed by three extremely preterm infants (<28 weeks of gestation), 3 very preterm (28 to <32 weeks) and 2 moderate preterm (32 to <33 weeks) [32]. However, also the number and severity of associated anomalies play an important role for survival. In fact, the two patients with the lowest gestational ages (23 and 26 weeks) and birth weights (540 and 750 g) had only a patent ductus arteriosus and survived with good outcome.
In conclusion, the incidence of ELBW infants with EA/TEF is rare (3 %) but these patients have a mortality rate of 50 %. Hence, the association of ELBW and EA/TEF results in high morbidity and mortality. In our series, the causes of death are mainly due to complications not associated with EA/TEF. Early TEF ligation followed by delayed esophageal repair can achieve a good outcome for ELBW infants. Our study confirms that for ELBW neonates with EA/TEF, associated anomalies represent a major risk factor for mortality.
References
Hack M, Fanaroff AA (1999) Outcomes of children of extremely low birth weight and gestational age in the 1990’s. Early Hum Dev 53:193–218
Mathews TJ, MacDorman MF, Menacker F (2002) Infant mortality statistics from the 1999 period linked birth/infant death data set. Natl Vital Stat Rep 50:1–28
Goldenberg RL, Culhane JF (2007) Low birth weight in the United States. Am J Clin Nutr 85:584S–590S
Itabashi K, Horiuchi T, Kusuda S et al (2009) Mortality rates for extremely low birth weight infants born in Japan in 2005. Pediatrics 123:445–450
Irvine B, Dzakpasu S, León JA (2015) Perinatal health indicators 2013: a surveillance report by the Public Health Agency of Canada’s perinatal surveillance system. Health Promot Chronic Dis Prev Can 35:23–24
Rowe MI, Rowe SA (2000) The last fifty years of neonatal surgical management. Am J Surg 180:345–352
Spitz L (2007) Oesophageal atresia. Orphanet J Rare Dis 2:24
Waterston DJ, Carter RE, Aberdeen E (1962) Oesophageal atresia: tracheo-oesophageal fistula. A study of survival in 218 infants. Lancet 1:819–822
Spitz L, Kiely EM, Morecroft JA et al (1994) Oesophageal atresia: at-risk groups for the 1990s. J Pediatr Surg 29:723–725
Engum SA, Grosfeld JL, West KW et al (1995) Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over 2 decades. Arch Surg 130:502–508
Choudhury SR, Ashcraft KW, Sharp RJ et al (1999) Survival of patients with esophageal atresia: influence of birth weight, cardiac anomaly, and late respiratory complications. J Pediatr Surg 34:70–73
Deurloo JA, Ekkelkamp S, Schoorl M et al (2002) Esophageal atresia: historical evolution of management and results in 371 patients. Ann Thorac Surg 73:267–272
Calisti A, Oriolo L, Nanni L et al (2004) Mortality and long term morbidity in esophageal atresia: the reduced impact of low birth weight and maturity on surgical outcome. J Perinat Med 32:171–175
Poenaru D, Laberge JM, Neilson IR et al (1993) A new prognostic classification for esophageal atresia. Surgery 113:426–432
Okamoto T, Takamizawa S, Arai H et al (2009) Esophageal atresia: prognostic classification revisited. Surgery 145:675–681
Narayan S, Aggarwal R, Upadhyay A et al (2003) Survival and morbidity in extremely low birth weight (ELBW) infants. Indian Pediatr 40:130–135
Doyle LW (2006) Evaluation of neonatal intensive care for extremely-low-birth-weight infants. Semin Fetal Neonatal Med 11:139–145
Fanaroff AA, Stoll BJ, Wright LL et al (2007) Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 196:147.e1–147.e8
Sritipsukho S, Suarod T, Sritipsukho P (2007) Survival and outcome of very low birth weight infants born in a university hospital with level II NICU. J Med Assoc Thai 90:1323–1329
Tagare A, Chaudhari S, Kadam S et al (2013) Mortality and morbidity in extremely low birth weight (ELBW) infants in a neonatal intensive care unit. Indian J Pediatr 80:16–20
Zamiara P, Thomas KE, Connolly BL et al. (2015) Long-term burden of care and radiation exposure in survivors of esophageal atresia. J Pediatr Surg 50:1686–1690
Kalache KD, Chaoui R, Mau H (1998) The upper neck pouch sign: a prenatal sonographic marker for esophageal atresia. Ultrasound Obstet Gynecol 11:138–140
Kalache KD, Wauer R, Mau H (2000) Prognostic significance of the pouch sign in fetuses with prenatally diagnosed esophageal atresia. Am J Obstet Gynecol 182:978–981
Seitz G, Warmann SW, Schaefer J et al (2006) Primary repair of esophageal atresia in extremely low birth weight infants: a single-center experience and review of the literature. Biol Neonate 90:247–251
Petrosyan M, Estrada J, Hunter C et al (2009) Esophageal atresia/tracheoesophageal fistula in very low-birth-weight neonates: improved outcomes with staged repair. J Pediatr Surg 44:2278–2281
Nishi E, Takamizawa S, Iio K et al (2014) Surgical intervention for esophageal atresia in patients with trisomy 18. Am J Med Genet A 164A:324–330
Beasley SW, Allen M, Myers N (1997) The effects of Down syndrome and other chromosomal abnormalities on survival and management in oesophageal atresia. Pediatr Surg Int 12:550–551
Fujimoto A, Allanson J, Crowe CA (1992) Natural history of mosaic trisomy 14 syndrome. Am J Med Genet 44:189–196
Jones TB, Kirchner SG, Lee FA et al (1980) Stomach rupture associated with esophageal atresia, tracheoesophageal fistula, and ventilatory assistance. AJR Am J Roentgenol 134:675–677
Holmes SJK, Kiely EM, Spitz L (1987) Tracheo-oesophageal fistula and the respiratory distress syndrome. Pediatr Surg Int 2:16–18
Malone PS, Kiely EM, Brain AJ (1990) Tracheo-oesophageal fistula and pre-operative mechanical ventilation. Aust N Z J Surg 60:525–527
Moutquin JM (2003) Classification and heterogeneity of preterm birth. BJOG 110:30–33
Acknowledgments
This work was supported by the endowment of the Robert M Filler Chair of Surgery, The Hospital for Sick Children.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zani, A., Wolinska, J., Cobellis, G. et al. Outcome of esophageal atresia/tracheoesophageal fistula in extremely low birth weight neonates (<1000 grams). Pediatr Surg Int 32, 83–88 (2016). https://doi.org/10.1007/s00383-015-3816-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3816-7