Abstract
Purpose
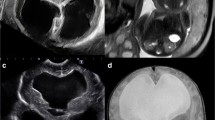
Foetal ventriculomegaly (VM) is one of the most commonly diagnosed brain abnormalities. The aims of this study were to assess cases with isolated VM, describe the prenatal course and assess short- and long-term follow-up at the age of 2 years.
Methods
We performed a retrospective analysis from our prenatal data base and included all children that were prenatally diagnosed with VM in our unit between 2008 and 2013 (n = 250). Prenatal management, postnatal outcome and neurologic development at the age of 2 years were evaluated.
Results
A total of 106 children were born at our institution and were diagnosed prenatally with isolated borderline VM. A total of 1.9% (n = 2/106) was transferred to the neonatal unit. A total of 0.9% (n = 1/106) showed abnormal findings in postnatal brain ultrasound. A total of 1.9% (n = 2/106) showed mild neurologic abnormalities after birth, but none had to be seen by a neuropediatrician. At the follow-up at 2 years, 2.5% (n = 1/40) had an insertion of a shunt.
Conclusion
Based on our analysis, the majority of isolated borderline VM do not show short- or long-term neurological abnormalities. However, all cases of VM should be referred to a detailed prenatal ultrasound exam by a specialist.


Similar content being viewed by others
Abbreviations
- VM:
-
Ventriculomegaly
- TORCH:
-
Toxoplasmosis, rubella, cytomegalovirus, herpes simplex virus 2 and other infections
- MRI:
-
Magnetic resonance imaging
- IUFD:
-
Intrauterine fetal death
- IUGR:
-
Intrauterine growth restriction
- WKS:
-
gestational week
- CMV:
-
Cytomegalovirus
- KIGGS:
-
Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland
References
Cardoza JD, Goldstein RB, Filly RA (1988) Exclusion of fetal ventriculomegaly with a single measurement: the width of the lateral ventricular atrium. Radiology 169(3):711–714
Gaglioti P, Oberto M, Todros T (2009) The significance of fetal ventriculomegaly: etiology, short- and long-term outcomes. Prenat Diagn 29(4):381–388
Kelly EN, Allen VM, Seaward G, Windrim R, Ryan G (2001) Mild ventriculomegaly in the fetus, natural history, associated findings and outcome of isolated mild ventriculomegaly: a literature review. Prenat Diagn 21(8):697–700
Breeze ACG, Alexander PMA, Murdoch EM, Missfelder-Lobos HH, Hackett GA, Lees CC (2007) Obstetric and neonatal outcomes in severe fetal ventriculomegaly. Prenat Diagn 27(2):124–129
Kennelly MM, Cooley SM, McParland PJ (2009) Natural history of apparently isolated severe fetal ventriculomegaly: perinatal survival and neurodevelopmental outcome. Prenat Diagn 29(12):1135–1140
Weichert J, Hartge D, Krapp M, Germer U, Gembruch U, Axt-Fliedner R (2010) Prevalence, characteristics and perinatal outcome of fetal ventriculomegaly in 29,000 pregnancies followed at a single institution. Fetal Diagn Ther 27(3):142–148
Gaglioti P, Danelon D, Bontempo S, Mombrò M, Cardaropoli S, Todros T (2005) Fetal cerebral ventriculomegaly: outcome in 176 cases. Ultrasound Obstet Gynecol 25(4):372–377
Joó JG, Tóth Z, Beke A, Papp C, Tóth-Pál E, Csaba A, Szigeti Z, Rab A, Papp Z (2008) Etiology, prenatal diagnostics and outcome of ventriculomegaly in 230 cases. Fetal Diagn Ther 24(3):254–263
Madazli R, Sal V, Erenel H, Gezer A, Ocak V (2011) Characteristics and outcome of 102 fetuses with fetal cerebral ventriculomegaly: experience of a university hospital in Turkey. Obstet Gynecol 31(2):142–145
Chiu T-H, Haliza G, Lin Y-H, Hung T-H, Hsu J-J, T’sang-T’ang H et al (2014) A retrospective study on the course and outcome of fetal ventriculomegaly. Taiwan J Obstet Gynecol 53(2):170–177
Signorelli M, Tiberti A, Valseriati D, Molin E, Cerri V, Groli C, Bianchi UA (2004) Width of the fetal lateral ventricular atrium between 10 and 12 mm: a simple variation of the norm? Ultrasound Obstet Gynecol 23(1):14–18
Pagani G, Thilaganathan B, Prefumo F (2014) Neurodevelopmental outcome in isolated mild fetal ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet Gynecol44(3):254–260
Larcos G, Gruenewald SM, Lui K (1994) Neonatal subependymal cysts detected by sonography: prevalence, sonographic findings, and clinical significance. AJR Am J Roentgenol 162(4):953–956
Adzick NS, Thom EA, Spong CY, Brock JW, Burrows PK, Johnson MP et al (2011) A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364(11):993–1004
Cavalheiro S, da Costa MDS, Mendonça JN, Dastoli PA, Suriano IC, Barbosa MM, Moron AF (2017) Antenatal management of fetal neurosurgical diseases. Childs Nerv Syst 33(7):1125–1141
Picone O, Simon I, Benachi A, Brunelle F, Sonigo P (2008) Comparison between ultrasound and magnetic resonance imaging in assessment of fetal cytomegalovirus infection. Prenat Diagn 28(8):753–758
Kagan KO, Hamprecht K (2017) Cytomegalovirus infection in pregnancy. Arch Gynecol Obstet 296(1):15–26
Pasquini L, Masini G, Gaini C, Franchi C, Trotta M, Dani C, di Tommaso M (2014) The utility of infection screening in isolated mild ventriculomegaly: an observational retrospective study on 141 fetuses. Prenat Diagn 34(13):1295–1300
Abdel-Fattah SA, Bhat A, Illanes S, Bartha JL, Carrington D (2005) TORCH test for fetal medicine indications: only CMV is necessary in the United Kingdom. Prenat Diagn 25(11):1028–1031
WHO | Preterm birth [Internet]. WHO. [cited 2017 Jan 8]. Available from: http://www.who.int/mediacentre/factsheets/fs363/en/. Accessed 8 Jan 2017
Ouahba J, Luton D, Vuillard E, Garel C, Gressens P, Blanc N, Elmaleh M, Evrard P, Oury JF (2006) Prenatal isolated mild ventriculomegaly: outcome in 167 cases. BJOG Int J Obstet Gynaecol 113(9):1072–1079
Baffero GM, Crovetto F, Fabietti I, Boito S, Fogliani R, Fumagalli M, Triulzi F, Mosca F, Fedele L, Persico N (2015) Prenatal ultrasound predictors of postnatal major cerebral abnormalities in fetuses with apparently isolated mild ventriculomegaly. Prenat Diagn 35(8):783–788
Nicolaides KH, Berry SB, Snijders RJM, Thorpe-Beeston JG, Gosden C (1990) Fetal lateral cerebral Ventriculomegaly: associated malformations and chromosomal defects. Fetal Diagn Ther 5(1):5–14
Benacerraf BR, Shipp TD, Bromley B, Levine D (2007) What does magnetic resonance imaging add to the prenatal sonographic diagnosis of ventriculomegaly? J Ultrasound Med 26(11):1513–1522
Salomon LJ, Ouahba J, Delezoide A-L, Vuillard E, Oury J-F, Sebag G, Garel C (2006) Third-trimester fetal MRI in isolated 10- to 12-mm ventriculomegaly: is it worth it? BJOG Int J Obstet Gynaecol 113(8):942–947
Yin S, Na Q, Chen J, Li-Ling J, Liu C (2010) Contribution of MRI to detect further anomalies in fetal Ventriculomegaly. Fetal Diagn Ther 27(1):20–24
Malinger G, Ben-Sira L, Lev D, Ben-Aroya Z, Kidron D, Lerman-Sagie T (2004) Fetal brain imaging: a comparison between magnetic resonance imaging and dedicated neurosonography. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 23(4):333–340
Paladini D, Quarantelli M, Sglavo G, Pastore G, Cavallaro A, D’Armiento MR et al (2014) Accuracy of neurosonography and MRI in clinical management of fetuses referred with central nervous system abnormalities. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 44(2):188–196
Parazzini C, Righini A, Doneda C, Arrigoni F, Rustico M, Lanna M, Triulzi F (2012) Is fetal magnetic resonance imaging indicated when ultrasound isolated mild ventriculomegaly is present in pregnancies with no risk factors? Prenat Diagn 32(8):752–757
Kutuk MS, Ozgun MT, Uludag S, Dolanbay M, Poyrazoglu HG, Tas M (2013) Postnatal outcome of isolated, nonprogressive, mild borderline fetal ventriculomegaly. Childs Nerv Syst 29(5):803–808
Chu N, Zhang Y, Yan Y, Ren Y, Wang L, Zhang B (2016) Fetal ventriculomegaly: pregnancy outcomes and follow-ups in ten years. Biosci Trends 10(2):125–132
Hölling H, Erhart M, Ravens-Sieberer U, Schlack R (2007) Verhaltensauffälligkeiten bei Kindern und Jugendlichen. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz 50(5–6):784–793
Hölling H, Schlack R, Petermann F, Ravens-Sieberer U, Mauz E, Group KS (2014) Psychische Auffälligkeiten und psychosoziale Beeinträchtigungen bei Kindern und Jugendlichen im Alter von 3 bis 17 Jahren in Deutschland – Prävalenz und zeitliche Trends zu 2 Erhebungszeitpunkten (2003–2006 und 2009–2012). Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz 57(7):807–819
Ihle W, Esser G (2002) Epidemiologie psychischer Störungen im Kindes- und Jugendalter. Psychol Rundsch 53(4):159–169
Richman N (1982) Pre-school to school: a behavioural study / N. Richman, J Stevenson, PJ Graham. Behavioural development: Children, 3-8 years Behaviour Development; Child psychology. London, New York: Academic Press, p 211-216
Weyerer S, Castell R, Biener A, Artner K, Dilling H (1988) Prevalence and treatment of psychiatric disorders in 3 to 14-year-old children: results of a representative field study in the small town rural region of Traunstein, upper Bavaria. Acta Psychiatr Scand 77(3):290–296
Kadesjö B, Gillberg C (1998) Attention deficits and clumsiness in Swedish 7-year-old children. Dev Med Child Neurol 40(12):796–804
Schott N, Roncesvalles N (2004) Motorische Ungeschicklichkeit. Z Sportpsychol 11(4):147–162
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Informed consent
There was no informed consent required for this retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tomic, K., Schönberger, H., Weber, P. et al. Significance of isolated borderline ventriculomegaly. Childs Nerv Syst 36, 393–399 (2020). https://doi.org/10.1007/s00381-019-04189-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04189-x