Abstract
Background
Ventriculoperitoneal shunt infection remains a significant problem. The introduction of antibiotic-impregnated shunt (AIS) systems in the prevention of shunt infection may represent a potential advance; however, there are no randomized controlled trials to establish a robust evidence-based practice. Previously published single-institution cohort studies have provided varying results on the efficacy of AIS systems in the prevention of shunt infection. In this study, we evaluate combined outcomes from three paediatric neurosurgical units in the use of AIS systems for paediatric patients with hydrocephalus.
Methods
The three units established independent databases with data collected from varying time frames. All procedures, where a complete AIS system or part was implanted into patients from 0–16 years in age, were included. The primary outcome measure was shunt infection rate. Shunt procedures were classified as de novo (DNS) and clean revision (CRS). An infant (<1 year) de novo insertion subgroup was also analyzed. AIS shunts were compared to a historical control of non-AIS shunts and results were analysed by centre using an odds ratio with a 95% confidence interval and combined across centres by meta-analysis.
Results
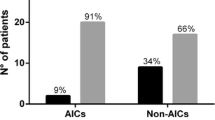
A total of 581 AIS implantation procedures were performed in all three units. The comparative non-AIS historical cohort comprised of 1,963 procedures. The pooled effect estimate indicated a clinical advantage for AIS shunts compared to non-AIS shunts, odds ratio (OR), 0.60 (95% CI 0.38, 0.93). The de novo infant group comprised 153 AIS systems, and 465 de novo shunts in the historical non-AIS cohort. Again the pooled effect estimate indicated a clinical advantage for AIS shunts compared to non-AIS shunts, OR 0.38 (95% CI, 0.17; 0.85); however, there was a large overlap of confidence intervals in the results from the different sites indicating the uncertainty in the treatment effect estimates. Over 80% of organisms were gram positive in the infected AIS cohort with a median time to infection of 19 days. Two rifampicin-resistant organisms and three MRSA organisms were detected.
Conclusion
Data from this exclusively paediatric multi-centre historical control study suggest that AIS may significantly reduce infection rates in de novo and clean revision shunt implants. Although the possibility of bias cannot be excluded due to study design, this is the largest study on an exclusively paediatric cohort comparing standard shunts to AIS implants. Future double-blinded RCTs are needed to confirm AIS efficacy.

Similar content being viewed by others
References
Aryan HE, Meltzer HS, Park MS, Bennett RL, Jandial R, Levy ML (2005) Initial experience with antibiotic-impregnated silicone catheters for shunting of cerebrospinal fluid in children. Childs Nerv Syst 21:56–61
Bayston R (1989) Hydrocephalus shunt infections. Chapman and Hall, London
Bayston R, Grove N, Siegel J, Lawellin D, Barsham S (1989) Prevention of hydrocephalus shunt catheter colonisation in vitro by impregnation with antimicrobials. J Neurol Neurosurg Psychiatry 52:605–609
Bayston R, Lambert E (1997) Duration of protective activity of cerebrospinal fluid shunt catheters impregnated with antimicrobial agents to prevent bacterial catheter-related infection. J Neurosurg 87:247–251
Bayston R, Ashraf W, Bhundia C (2004) Mode of action of an antimicrobial biomaterial for use in hydrocephalus shunts. J Antimicrob Chemother 53:778–782
Belli A, Thompson DNP, Harkness WFJ, Pitt M, Hayward RD (2001) Shunt infection rates: surgical skill or statistical serendipity? Analysis of 1,106 cases. Br J Neurosurg 15:82, Abstract
Borgbjerg BM, Gjerris F, Albeck MJ, Borgesen SE (1995) Risk of infection after cerebrospinal fluid shunt: an analysis of 884 first time shunts. Acta Neurochir (Wien) 136:1–7
Choksey MS, Malik IA (2004) Zero tolerance to shunt infections: can it be achieved? J Neurol Neurosurg Psychiatry 75:87–91
Choux M, Genitori L, Lang D, Lena G (1992) Shunt implantation: reducing the incidence of shunt infection. J Neurosurg 77:875–880
Drake JM, Sainte-Rose C (1995) The shunt book. Blackwell Science, Cambridge, Mass
Enger PO, Svendsen F, Wester K (2003) CSF shunt infections in children: experiences from a population-based study. Acta Neurochir (Wien) 145:243–248
Eymann R, Chehab S, Strowitzki M, Steudel W-I, Keifer M (2008) Clinical and economic consequences of antibiotic-impregnated cerebrospinal fluid shunt catheters. J Neurosurg Pediatrics 1:444–450
Fan-Havard P, Nahata MC (1987) Treatment and prevention of infections of cerebrospinal fluid shunts. Clin Pharm 6:866–880
Govender ST, Nathoo N, van Dellen JR (2003) Evaluation of an antibiotic-impregnated shunt system for the treatment of hydrocephalus. J Neurosurg 99:831–839
Hayhurst C, Cooke R, Williams D, Kandasamy J, O'Brien DF, Mallucci CL (2008) The impact of antibiotic-impregnated catheters on shunt infection in children and neonates. Childs Nerv Syst 24(5):557–562, Epub 2007 Oct 26
Kan P, Kestle J (2007) Lack of efficacy of antibiotic-impregnated shunt systems in preventing shunt infections in children. Childs Nerv Syst 23:773–777
Kulkarni AV, Drake JM, Lamberti-Pasculli M (2001) Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg 94:195–201
Pattavilakom A, Kotasnas D, Korman TM, Xenos C, Danks A (2006) Duration of in vivo antimicrobial activity of antibiotic-impregnated cerebrospinal fluid catheters. Neurosurgery 58:930–935
Pattavilakom A, Xenos C, Bradfield O, Danks RA (2007) Reduction in shunt infection using antibiotic impregnated CSF shunt catheters: an Australian prospective study. J Clin Neurosci 14(6):526–531
Pople IK, Bayston R, Hayward RD (1992) Infection of cerebrospinal fluid shunts in infants: a study of etiological factors. J Neurosurg 77:29–36
Ratilal B, Costa J, Sampaio C (2008) Antibiotic prophylaxis for surgical introduction of intracranial ventricular shunts: a systematic review. J Neurosurg Pediatrics 1:48–56
Ritz R, Roser F, Morgalla M, Dietz K, Tatagiba M, Will BE (2007) Do antibiotic-impregnated shunts in hydrocephalus therapy reduce the risk of infection? An observational study in 258 patients. BMC Infect Dis 8(7):38
Richards HK, Seeley HM, Pickard JD (2009) Efficacy of antibiotic-impregnated shunt catheters in reducing shunt infection: data from the United Kingdom Shunt Registry. J Neurosurg Pediatr 4(4):389–393
Ronan A, Hogg GG, Klug GL (1995) Cerebrospinal fluid shunt infections in children. Pediatr Infect Dis J 14:782–786
Schiff SJ, Oakes WJ (1989) Delayed cerebrospinal-fluid shunt infection in children. Pediatr Neurosci 15:131–135
Sciubba DM, Stuart RM, McGirt MJ, Woodworth GF, Samdani A, Carson B, Jallo GI (2005) Effect of antibiotic-impregnated shunt catheters in decreasing the incidence of shunt infection in the treatment of hydrocephalus. J Neurosurg 103:131–136
Sciubba DM, Lin LM, Woodworth GF, McGirt MJ, Carson B, Jallo GI (2007) Factors contributing to the medical costs of cerebrospinal fluid shunt infection treatment in pediatric patients with standard shunt components compared with those in patients with antibiotic impregnated components. Neurosurg Focus 22(4):E9
Sciubba DM, McGirt MJ, Woodworth GF, Carson B, Jallo GI (2007) Prolonged exposure to antibiotic-impregnated shunt catheters does not increase incidence of late shunt infections. Childs Nerv Syst 23:867–871
Shapiro S, Boaz J, Kleiman M, Kalsbeck J, Mealey J (1988) Origin of organisms infecting ventricular shunts. Neurosurgery 22:868–872
Taggart DP, D'Amico R, Altman DG (2001) Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet 358(9285):870–875
Thompson DN, Hartley JC, Hayward RD (2007) Shunt infection: is there a near-miss scenario? J Neurosurg 106(1 Suppl):15–19
Walters BC, Hoffman HJ, Hendrick EB, Humphreys RP (1984) Cerebrospinal fluid shunt infection. Influences on initial management and subsequent outcome. J Neurosurg 60:1014–1021
Wang KW, Chang WN, Shih TY, Huang CR, Tsai NW, Chang CS, Chuang YC, Liliang PC, Su TM, Rau CS, Tsai YD, Cheng BC, Hung PL, Chang CJ, Lu CH (2004) Infection of cerebrospinal fluid shunts: causative pathogens, clinical features, and outcomes. Jpn J Infect Dis 57:44–48
Conflict of interest
None.
Disclosure
The authors confirm that no financial support has been received for the inception or preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kandasamy, J., Dwan, K., Hartley, J.C. et al. Antibiotic-impregnated ventriculoperitoneal shunts—a multi-centre British paediatric neurosurgery group (BPNG) study using historical controls. Childs Nerv Syst 27, 575–581 (2011). https://doi.org/10.1007/s00381-010-1290-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1290-z