Abstract
Introduction
The global surgery workforce is in crisis in many low- and middle-income countries (LMICs). The shortage of surgery, obstetrics, and anesthesia providers is an important cause of the unmet need for surgical care in LMICs. The goal of this paper is to summarize the available literature about surgical physicians in LMICs and to describe ongoing initiatives to supplement the existing surgical workforce data.
Methods
We performed a systematic search and literature review of the English-language literature regarding the number of surgeons, obstetrician–gynecologists, and anesthesiologists practicing in LMICs.
Results
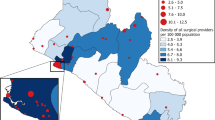
Literature describing the number of surgeons, obstetricians, and anesthesiologists practicing in LMICs represents a small minority of LMICs, and indicates consistently low levels of surgical physicians. Our literature search yielded comprehensive data for only six countries. No national data were found for 23 of the 57 countries considered by the World Health Organization (WHO) to be in health workforce ‘crisis.’ Across LMICs, general surgeon density ranged from 0.13 to 1.57 per 100,000 population, obstetrician density ranged from 0.042 to 12.5 per 100,000, and anesthesiologist density ranged from 0 to 4.9 per 100,000. Total anesthesiologist, obstetrician, and surgeon density was significantly correlated with gross domestic product (GDP) per capita (r 2 = 0.097, p = 0.0002).
Conclusion
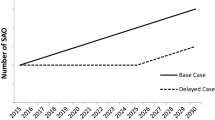
The global surgery workforce is in crisis, yet is poorly characterized by the current English-language literature. There is a critical need for systematically collected, national-level data regarding surgery providers in LMICs to guide improvements in surgery access and care. The Harvard Global Surgery Workforce Initiative and the WHO global surgical workforce database are working to address this need by surveying Ministries of Health and surgical professional organizations around the world.



Similar content being viewed by others
References
Ozgediz D, Kijjambu S, Galukande M et al (2008) Africa’s neglected surgical workforce crisis. Lancet 371:627–628
Ozgediz D, Galukande M, Mabweijano J et al (2008) The neglect of the global surgical workforce: experience and evidence from Uganda. World J Surg 32:1208–1215. doi:10.1007/s00268-008-9473-4
Kruk ME, Wladis A, Mbembati N et al (2010) Human resource and funding constraints for essential surgery in district hospitals in Africa: a retrospective cross-sectional survey. PLoS Med 7:e1000242
Grimes CE, Bowman KG, Dodgion CM et al (2011) Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg 35:941–950. doi:10.1007/s00268-011-1010-1
Dubowitz G, Detlefs S, McQueen KA (2010) Global anesthesia workforce crisis: a preliminary survey revealing shortages contributing to undesirable outcomes and unsafe practices. World J Surg 34:438–444. doi:10.1007/s00268-009-0229-6
Global Health Workforce Alliance (2008) Health workers for all and all for health workers: an agenda for global action. First Global Forum on Human Resources for Health, Kampala, 2–7 March
World Health Organization (2010) WHO global code of practice on the international recruitment of health personnel. WHO, Geneva
Gow J, George G, Mutinta G et al (2011) Health worker shortages in Zambia: an assessment of government responses. J Public Health Policy 32:476–488
Rolfe B, Leshabari S, Rutta F et al (2008) The crisis in human resources for health care and the potential of a ‘retired’ workforce: case study of the independent midwifery sector in Tanzania. Health Policy Plan 23:137–149
Tjoa A, Kapihya M, Libetwa M et al (2010) Meeting human resources for health staffing goals by 2018: a quantitative analysis of policy options in Zambia. Hum Resour Health 8:15
Petroze RT, Nzayisenga A, Rusanganwa V et al (2012) Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. Br J Surg 99:436–443
Iddriss A, Shivute N, Bickler S et al (2011) Emergency, anaesthetic and essential surgical capacity in the Gambia. Bull World Health Organ 89:565–572
OECD Surgeons in OECD and non-OECD Countries (2012) In: OECD editor, OECD
Lebrun DG, Saavedra-Pozo I, Agreda-Flores F et al (2012) Surgical and anesthesia capacity in Bolivian public hospitals: results from a national hospital survey. World J Surg 36(11):2559–2566. doi:10.1007/s00268-012-1722-x
Van Heng Y, Davoung C, Husum H (2008) Non-doctors as trauma surgeons? A controlled study of trauma training for non-graduate surgeons in rural Cambodia. Prehosp Disaster Med 23:483–489 discussion 490–481
Poggetti RS (2008) Acute care surgeon South American model. World J Surg 32:1626–1629. doi:10.1007/s00268-008-9659-9
Kassum DA, Valji A, Gulyazov S (2003) General surgery in a district hospital in Tajikistan: clinical impact of a partnership between visiting volunteers and host specialists. Can J Surg 46:335–339
Ahmed SM, Hossain MA, Rajachowdhury AM et al (2011) The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health 9:3
Lebrun DG, Dhar D, Sarkar MI et al (2012) Measuring global surgical disparities: a survey of surgical and anesthesia infrastructure in Bangladesh. World J Surg 37(1):24–31. doi:10.1007/s00268-012-1806-7
Essential Surgery Group (2007) Conference on increasing access to surgical services in resource-constrained settings in Sub-Saharan Africa, Bellagio, Bellagio Report, Lake Como, 4–8 June
Bickler S, Ozgediz D, Gosselin R et al (2010) Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World J Surg 34:374–380. doi:10.1007/s00268-009-0261-6
Grimes CE, Law RS, Borgstein ES et al (2012) Systematic review of met and unmet need of surgical disease in rural sub-Saharan Africa. World J Surg 36:8–23. doi:10.1007/s00268-011-1330-1
Prytherch H, Massawe S, Kuelker R et al (2007) The unmet need for emergency obstetric care in Tanga Region, Tanzania. BMC Pregnancy Childbirth 7:16
Godal T, Quam L (2012) Accelerating the global response to reduce maternal mortality. Lancet 379:2025–2026
Pearson L, Shoo R (2005) Availability and use of emergency obstetric services: Kenya, Rwanda, Southern Sudan, and Uganda. Int J Gynaecol Obstet 88:208–215
Murray CJ, Vos T, Lozano R et al (2013) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2197–2223
World Bank Dataset (2012) Population, total. The World Bank, Washington, DC
World Bank Dataset (2013) GDP per capita (current US$). The World Bank, Washington, DC
World Health Organization (2006) World health report 2006: working together for health. WHO, Geneva
Fletcher P, McDonald A, McCartney T et al (2003) Surgery in Jamaica. Arch Surg 138:1150–1153
Gnassingbe K, Tekou H, da Silva-Anoma S et al (2011) The paediatric surgeon and his working conditions in Francophone sub-Saharan Africa. Afr J Paediatr Surg 8:298–300
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32:533–536. doi:10.1007/s00268-008-9525-9
Ozgediz D, Riviello R, Rogers SO (2008) The surgical workforce crisis in Africa: a call to action. Bull Am Coll Surg 93:10–16
Debas HT, Gosselin R, McCord C et al (2006) Surgery. In: Jamison DT, Breman JG, Measham AR et al (eds) Disease control priorities in developing countries. The International Bank for Reconstruction and Development/The World Bank Group, Washington, DC
Groen RS, Samai M, Kamara TB et al (2012) The unmet surgical disease burden in the developing world. Lancet 379:616
Galukande M, von Schreeb J, Wladis A et al (2010) Essential surgery at the district hospital: a retrospective descriptive analysis in three African countries. PLoS Med 7:e1000243
Reshamwalla S, Gobeze AA, Ghosh S et al (2012) Snapshot of surgical activity in rural Ethiopia: is enough being done? World J Surg 36:1049–1055. doi:10.1007/s00268-012-1511-6
Bowman KG, Berry WR, Gawande A (2012) Pediatric emergency and essential care in Zambian hospitals: a nationwide study. American Academy of Pediatrics 2012 National Conference & Exhibition, Ernest N. Morial Convention Center, New Orleans, 20–23 October 2012
Choo S, Perry H, Hesse AA et al (2010) Assessment of capacity for surgery, obstetrics and anaesthesia in 17 Ghanaian hospitals using a WHO assessment tool. Trop Med Int Health 15(9):1109–1115
Contini S, Taqdeer A, Cherian M et al (2010) Emergency and essential surgical services in Afghanistan: still a missing challenge. World J Surg 34:473–479. doi:10.1007/s00268-010-0406-7
Osen H, Chang D, Choo S et al (2011) Validation of the World Health Organization tool for situational analysis to assess emergency and essential surgical care at district hospitals in Ghana. World J Surg 35:500–504. doi:10.1007/s00268-010-0918-1
Penoyar T, Cohen H, Kibatala P et al (2012) Emergency and surgery services of primary hospitals in the United Republic of Tanzania. BMJ Open 2:e000369
Sherman L, Clement PT, Cherian MN et al (2011) Implementing Liberia’s poverty reduction strategy: an assessment of emergency and essential surgical care. Arch Surg 146:35–39
Taira BR, Cherian MN, Yakandawala H et al (2010) Survey of emergency and surgical capacity in the conflict-affected regions of Sri Lanka. World J Surg 34:428–432. doi:10.1007/s00268-009-0254-5
Kingham TP, Kamara TB, Cherian MN et al (2009) Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Arch Surg 144:122–127; discussion 128
World Health Organization (2012) Emergency and essential surgical care: WHO EESC Global Database. WHO, Geneva
Kushner AL, Groen RS, Kamara TB et al (2012) Assessment of pediatric surgery capacity at government hospitals in Sierra Leone. World J Surg 36(11):2554–2558. doi:10.1007/s00268-012-1737-3
Groen RS, Kamara TB, Dixon-Cole R et al (2012) A tool and index to assess surgical capacity in low income countries: an initial implementation in Sierra Leone. World J Surg 36:1970–1977. doi:10.1007/s00268-012-1591-3
Henry JA, Windapo O, Kushner AL et al (2012) A survey of surgical capacity in rural southern Nigeria: opportunities for change. World J Surg 36:2811–2818. doi:10.1007/s00268-012-1764-0
Chao TE, Burdic M, Ganjawalla K et al (2012) Survey of surgery and anesthesia infrastructure in Ethiopia. World J Surg 36(11):2545–2553. doi:10.1007/s00268-012-1729-3
Linden AF, Sekidde FS, Galukande M et al (2012) Challenges of surgery in developing countries: a survey of surgical and anesthesia capacity in Uganda’s public hospitals. World J Surg 36:1056–1065. doi:10.1007/s00268-012-1482-7
Notrica MR, Evans FM, Knowlton LM et al (2011) Rwandan surgical and anesthesia infrastructure: a survey of district hospitals. World J Surg 35:1770–1780. doi:10.1007/s00268-011-1125-4
Chu K, Rosseel P, Gielis P et al (2009) Surgical task shifting in Sub-Saharan Africa. PLoS Med 6:e1000078
Chu KM, Ford NP, Trelles M (2011) Providing surgical care in Somalia: a model of task shifting. Confl Health 5:12
Cherian M, Choo S, Wilson I et al (2010) Building and retaining the neglected anaesthesia health workforce: is it crucial for health systems strengthening through primary health care? Bull World Health Organ 88:637–639
World Health Organization (2012) WHO global health observatory data repository. WHO, Geneva
Transparency International. Corruption perceptions index. http://www.transparency.org/. Accessed 21 May 2013
Mullan F, Frehywot S (2007) Non-physician clinicians in 47 sub-Saharan African countries. Lancet 370:2158–2163
Mullan F, Frehywot S, Omaswa F et al (2011) Medical schools in sub-Saharan Africa. Lancet 377:1113–1121
Sherr K, Mussa A, Chilundo B et al (2012) Brain drain and health workforce distortions in Mozambique. PLoS One 7:e35840
Hagander LE, Hughes CD, Nash K et al (2013) Surgeon migration between developing countries and the United States: train, retain, and gain from brain drain. World J Surg 37(1):14–23. doi:10.1007/s00268-012-1795-6
Terhune KP, Zaydfudim V, Abumrad NN (2010) International medical graduates in general surgery: increasing needs, decreasing numbers. J Am Coll Surg 210:990–996
Itani KM, Hoballah J, Kaafarani H et al (2011) Could international medical graduates offer a solution to the surgical workforce crisis? Balancing national interest and global responsibility. Surgery 149:597–600
Debas HT (2006) The problem of heavy reliance on international medical graduates to supply the surgical workforce in the United States. Surgery 140:359–361
Mullan F (2005) The metrics of the physician brain drain. N Engl J Med 353:1810–1818
Clemens MA, Pettersson G (2008) New data on African health professionals abroad. Hum Resour Health 6:1
MacDonagh R, Jiddawi M, Parry V (2002) Twinning: the future for sustainable collaboration. BJU Int 89(Suppl 1):13–17
Gemici G (2006) The metrics of the physician brain drain. N Engl J Med 354:528–530;author reply 528–530
Chandra A (2006) The metrics of the physician brain drain. N Engl J Med 354:528–530;author reply 528–530
Weiser TG, Makary MA, Haynes AB et al (2009) Standardised metrics for global surgical surveillance. Lancet 374:1113–1117
Thompson MJ, Lynge DC, Larson EH et al (2005) Characterizing the general surgery workforce in rural America. Arch Surg 140:74–79
Chang DC, Eastman B, Talamini MA et al (2011) Density of surgeons is significantly associated with reduced risk of deaths from motor vehicle crashes in US counties. J Am Coll Surg 212:862–866
Hagander L, Hoyler M, Finlayson SR et al (2013) National density of surgeons and anesthesiologists is significantly correlated with maternal mortality. Bethune Round Table, Vancouver (BC), 2013
Adegoke AA, van den Broek N (2009) Skilled birth attendance: lessons learnt. BJOG 116(Suppl 1):33–40
Adegoke A, Utz B, Msuya SE et al (2012) Skilled birth attendants: who is who? A descriptive study of definitions and roles from nine Sub Saharan African countries. PLoS One 7:e40220
Harvey SA, Blandon YC, McCaw-Binns A et al (2007) Are skilled birth attendants really skilled? A measurement method, some disturbing results and a potential way forward. Bull World Health Organ 85:783–790
World Health Organization (2008) Spotlight on health workforce statistics. WHO, Geneva
World Health Organization. Technical notes: global health workforce statistics database. WHO, Geneva
OECD (2012) OECD health data: health care resources. OECD Health Statistics (database). http://www.oecd-ilibrary.org/content/data/data-00541-en. Accessed 19 Feb 2013
Mavalankar D, Sriram V (2009) Provision of anaesthesia services for emergency obstetric care through task shifting in South Asia. Reprod Health Matters 17:21–31
de Jesus LE, Aguiar AS, de Campos Mdo S et al (2009) Needs and specialization for pediatric surgeons in Brazil [article in Portuguese]. Rev Col Bras Cir 36:356–361
Dewan PA (1995) Paediatric surgery in Cambodia. Med J Aust 163:640–642
Chirdan LB, Ameh EA, Abantanga FA et al (2010) Challenges of training and delivery of pediatric surgical services in Africa. J Pediatr Surg 45:610–618
Gaym A (2010) Audit of obstetrician-gynecologists in Ethiopia, 1950s–2007: implications for specialty level reproductive health care provision. Ethiop Med J 48:137–148
Edwin F, Tettey M, Aniteye E et al (2011) The development of cardiac surgery in West Africa—the case of Ghana. Pan Afr Med J 9:15
Cameron BH, Rambaran M, Sharma DP et al (2010) International surgery: the development of postgraduate surgical training in Guyana. Can J Surg 53:11–16
Smith SR (1984) How might we improve surgical services for rural populations in developing countries? Br Med J (Clin Res Ed) 289:494–495
Lavy C, Tindall A, Steinlechner C et al (2007) Surgery in Malawi: a national survey of activity in rural and urban hospitals. Ann R Coll Surg Engl 89:722–724
Spiegel DA, Choo S, Cherian M et al (2011) Quantifying surgical and anesthetic availability at primary health facilities in Mongolia. World J Surg 35:272–279. doi:10.1007/s00268-010-0904-7
Adepoju FG, Ayanniyi AA, Pam V et al (2011) Human resource development for Vision 2020 in developing countries: a change from absolute numbers. Eur J Ophthalmol 21:820–825
Ameh EA, Adejuyigbe O, Nmadu PT (2006) Pediatric surgery in Nigeria. J Pediatr Surg 41:542–546
Blanchard RJ, Blanchard ME, Toussignant P et al (1987) The epidemiology and spectrum of surgical care in district hospitals of Pakistan. Am J Public Health 77:1439–1445
Natuzzi ES, Kushner A, Jagilly R et al (20011) Surgical care in the Solomon Islands: a road map for universal surgical care delivery. World J Surg 35:1183–1193. doi:10.1007/s00268-011-1097-4
Abdool-Carrim AT, Veller MG (2010) Vascular surgical education in a medium-income country. Eur J Vasc Endovasc Surg 39(Suppl 1):S22–S24
Bornman PC, Krige JE (2005) Perspectives on surgery in the new South Africa. World J Surg 29:949–952. doi:10.1007/s00268-005-0141-7
Hodges S, Wilson J, Hodges A (2009) Plastic and reconstructive surgery in Uganda: 10 years experience. Paediatr Anaesth 19:12–18
Walker IA, Obua AD, Mouton F et al (2010) Paediatric surgery and anaesthesia in south-western Uganda: a cross-sectional survey. Bull World Health Organ 88:897–906
Al Serouri AW, Al Rukeimi A, Bin Afif M et al (2012) Findings from a needs assessment of public sector emergency obstetric and neonatal care in four governorates in Yemen: a human resources crisis. Reprod Health Matters 20:122–128
World Health Organization (2012) Global initiative for emergency and essential surgical care. WHO, Geneva
World Health Organization (2011) Mental health atlas. WHO, Geneva
Acknowledgments
The authors wish to acknowledge the collaboration of Dr. Meena Nathan Cherian of the WHO Department of Health Systems Policies and Workforce, and Dr. Amani Siyam of Human Resources for Health and the WHO Department of Health Systems Policies and Workforce.
Conflict of interest
The authors report no potential or real conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoyler, M., Finlayson, S.R.G., McClain, C.D. et al. Shortage of Doctors, Shortage of Data: A Review of the Global Surgery, Obstetrics, and Anesthesia Workforce Literature. World J Surg 38, 269–280 (2014). https://doi.org/10.1007/s00268-013-2324-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2324-y