Abstract
Background
Gallstones remain a common clinical problem requiring skilled operative and nonoperative management. The aim of the present population-based study was to investigate causes of gallstone-related mortality in Scotland.
Methods
Surgical deaths were peer reviewed between 1997 and 2006 through the Scottish Audit of Surgical Mortality (SASM); data were analyzed for patients in whom the principal diagnosis on admission was gallstone disease.
Results
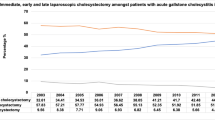
Gallstone disease was responsible for 790/43,271 (1.83%) of the surgical deaths recorded, with an overall mortality for cholecystectomy of 0.307% (176/57,352), endoscopic retrograde cholangiopancreatography (ERCP) of 0.313% (117/37,345), and cholecystostomy of 2.1% (12/578) across the decade. However, the majority of patients who died were elderly (47.6% ≥80 years or older) and were managed conservatively. Deaths following cholecystectomy usually followed emergency admission (76%) and were more likely to have been associated with postoperative medical complications (n = 189) than surgical complications (n = 36).
Discussion
Although cholecystectomy is a relatively safe procedure, patients who die as a result of gallstone disease tend to be elderly, to have been admitted as emergency cases, and to have had co-morbidities. Future combined medical and surgical perioperative management may reduce the mortality rate associated with gallstones.

Similar content being viewed by others
References
Gurusamy KS, Samraj K, Fusai G et al (2008) Early versus delayed laparoscopic cholecystectomy for biliary colic. Cochrane Database Syst Rev 4:CD007196
Nilsson E, Fored CM, Granath F et al (2005) Cholecystectomy in Sweden 1987–99: a nationwide study of mortality and preoperative admissions. Scand J Gastroenterol 40:1478–1485
Rosenmuller M, Haapamaki MM, Nordin P et al (2007) Cholecystectomy in Sweden 2000–2003: a nationwide study on procedures, patient characteristics, and mortality. BMC Gastroenterol 7:35–43
McMahon AJ, Fischbacher CM, Frame SH et al (2000) Impact of laparoscopic cholecystectomy: a population-based study. Lancet 356:1632–1637
Maxwell JG, Tyler BA, Rutledge R et al (1998) Cholecystectomy in patients aged 80 and older. Am J Surg 176:627–631
Winbladh A, Gullstrand P, Svanvik J et al (2009) Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford) 11:183–193
Knudson K, Raeburn CD, McIntyre RC Jr et al (2008) Management of duodenal and pancreaticobiliary perforations associated with periampullary endoscopic procedures. Am J Surg 196:975–981
Andriulli A, Loperfido S, Napolitano G et al (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102:1781–1788
Stonebridge PA, Thompson AM, Nixon SJ (1999) Completion of the journey of care: Scottish Audit of Surgical Mortality (SASM). J R Coll Surg Edinb 44:185–186
Thompson AM, Stonebridge PA (2005) Building a framework for trust: critical event analysis of deaths in surgical care. Br Med J 330:1139–1142
Parks RW, Bettschart V, Frame S et al (2004) Benefits of specialisation in the management of pancreatic cancer: results of a Scottish population-based study. Br J Cancer 91:459–465
Tekkis PP, Poloniecki JD, Thompson MR et al (2003) Operative mortality in colorectal cancer: prospective national study. Br Med J 327:1196–1201
McCulloch P, Ward J, Tekkis PP (2003) Mortality and morbidity in gastro-oesophageal cancer surgery: initial results of ASCOT multicentre prospective cohort study. Br Med J 327:1192–1197
Thompson AM, Ashraf Z, Burton H et al (2005) Mapping changes in surgical mortality over 9 years by peer review audit. Br J Surg 92:1449–1452
Vascular Society of Great Britain and Ireland. Fourth National Vascular Database Report 2004
National Confidential Enquiry into Perioperative Death (2005) Annual Report. Abdominal aortic aneurysm: a service in need of surgery?
Keogh B, Spiegelhalter D, Bailey A et al (2004) The legacy of Bristol: public disclosure of individual surgeons’ results. Br Med J 329:450–454
Lam CM, Murray FE, Cuschieri A (1996) Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy in Scotland. Gut 38:282–284
Campbell EJ, Montgomery DA, Mackay CJ (2008) A national survey of current surgical treatment of acute gallstone disease. Surg Laparosc Endosc Percutan Tech 18:242–247
David GG, Al-Sarira AA, Willmott S et al (2008) Management of acute gallbladder disease in England. Br J Surg 95:472–476
Cameron IC, Chadwick C, Phillips J et al (2004) Management of acute cholecystitis in UK hospitals: time for a change. Postgrad Med J 80:292–294
Cameron IC, Chadwick C, Phillips J et al (2000) Current practice in the management of acute cholecystitis. Br J Surg 87:362–373
Hadad SM, Vaidya JS, Baker L et al (2007) Delay from symptom onset increases the conversion rate in laparoscopic cholecystectomy for acute cholecystitis. World J Surg 31:1201–1298
Griniatsos J, Petrou A, Pappas P et al (2008) Percutaneous cholecystostomy without interval cholecystectomy as definitive treatment of acute cholecystitis in elderly and critically ill patients. South Med J 101:586–590
Schreurs WH, Vles WJ, Stuifbergen WH et al (2004) Endoscopic management of common bile duct stones leaving the gallbladder in situ. A cohort study with long-term follow-up. Dig Surg 21:60–64
Boytchev I, Pelletier G, Prat F et al (2000) Late biliary complications after endoscopic sphincterotomy for common bile duct stones in patients older than 65 years of age with gallbladder in situ. Gastroenterol Clin Biol 24:995–1000
McAlister VC, Davenport E, Renouf E (2007) Cholecystectomy deferral in patients with endoscopic sphincterotomy. Cochrane Database Syst Rev 4:CD006233
Dawson J, Vig S, Choke E et al (2007) Medical optimisation can reduce morbidity and mortality associated with elective aortic aneurysm repair. Eur J Vasc Endovasc Surg 33:100–104
Cuthbertson BH, Campbell M, Stott SA et al (2010) A pragmatic multi-centre randomised controlled trial of fluid loading and level of dependency in high-risk surgical patients undergoing major elective surgery: trial protocol. Trials 11:41 (Epub ahead of print, Apr 16, 2010)
Acknowledgments
The authors thank Dave Stobie, David Readhead, Christine Torrance, and Lynsey Kerr from the Information Services Division of the National Health Service (NHS), National Services Scotland, for assistance with this research. They also acknowledge the assistance of Mr. Jamie Young, Department of Surgery, Ninewells Hospital, for help with statistical analysis.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scollay, J.M., Mullen, R., McPhillips, G. et al. Mortality Associated with the Treatment of Gallstone Disease: A 10-Year Contemporary National Experience. World J Surg 35, 643–647 (2011). https://doi.org/10.1007/s00268-010-0908-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0908-3