Abstract
Introduction
Studies have shown that the use of nonlocking (reconstruction) plates in fixing distal humerus fractures may not yield stable fixation which therefore requires long immobilization and suboptimal functional results. There are reports showing that locking plates are biomechanically superior to nonlocking plates. The aim of this study was to compare elbow functional outcomes between locking and nonlocking plates in fixation of distal humerus fractures.
Methods
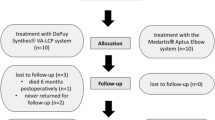
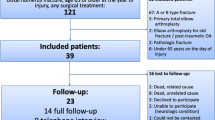
A single-centre, randomized control study was conducted at an academic level 1 trauma centre. A total of 60 patients with type 13-A fracture (AO/OTA classification) were randomized into two equal groups, locking plates group, and nonlocking plates group. The primary outcome measure was the Mayo elbow performance score (MEPS) at one year. Secondary outcomes measures were elbow flexion/extension arc, union, operative time, and complications (e.g., infection, heterotrophic ossification).
Results
The Mayo Elbow Performance Score (MEPS) at one year was 88 ± 10.1 in locking plates group and 75.8 ± 12.8 in nonlocking plates group. The difference was found to be statically significant (P value = 0.01). Elbow flexion/extension arc of motion at one year was 116° ± 15° in locking plates group and 113° ± 28° in nonlocking plates. The difference was not found to be statistically significant (P value = 0.17).
Conclusion
Both implants yield similar results, with locking plates showing slightly better clinical scores.



Similar content being viewed by others
References
Huang TL, Chiu FY, Chuang TY, Chen TH (2005) The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus. J Trauma 58(1):62–69
Sodergard J, Sandelin J, Bostman O (1992) Postoperative complications of distal humeral fractures. 27/96 adults followed up for 6 (2-10) years. Acta Orthop Scand 63(1):85–89
Jacobson SR, Glisson RR, Urbaniak JR (1997) Comparison of distal humerus fracture fixation: a biomechanical study. J South Orthop Assoc 6(4):241–249
Self J, Viegas SF, Buford WL Jr, Patterson RM (1995) A comparison of double-plate fixation methods for complex distal humerus fractures. J Shoulder Elbow Surg 4(1 Pt 1):10–16
Schuster I, Korner J, Arzdorf M, Schwieger K, Diederichs G, Linke B (2008) Mechanical comparison in cadaver specimens of three different 90-degree double-plate osteosyntheses for simulated C2-type distal humerus fractures with varying bone densities. J Orthop Trauma 22(2):113–120
Reising K, Hauschild O, Strohm PC, Suedkamp NP (2009) Stabilisation of articular fractures of the distal humerus: early experience with a novel perpendicular plate system. Injury 40(6):611–617
Caravaggi P, Laratta JL, Yoon RS, De Biasio J, Ingargiola M, Frank MA, Capo JT, Liporace FA (2014) Internal fixation of the distal humerus: a comprehensive biomechanical study evaluating current fixation techniques. J Orthop Trauma 28(4):222–226
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF (2018) Fracture and dislocation classification compendium. J Orthop Trauma 32(Supplement 1):S1–S170
Schildhauer TA, Nork SE, Mills WJ, Henley MB (2003) Extensor mechanism-sparing paratricipital posterior approach to the distal humerus. J Orthop Trauma 17(5):374–378
Cusick MC, Bonnaig NS, Azar FM, Mauck BM, Smith RA, Throckmorton TW (2014) Accuracy and reliability of the Mayo Elbow Performance Score. J Hand Surg Am 9(6):1146–1150
Greiner S, Haas NP, Bail HJ (2008) Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Arch Orthop Trauma Surg 128(7):723–729
Valone LC, Waites C, Tartarilla AB et al (2019) Functional elbow range of motion in children and adolescents [published online ahead of print]. J Pediatr Orthop. https://doi.org/10.1097/BPO.0000000000001467
O’Driscoll SW (2005) Optimizing stability in distal humeral fracture fixation. J Shoulder Elbow Surg 14(1 Suppl S):186–194
Horne G (1980) Supracondylar fractures of the humerus in adults. J Trauma 20(1):71–74
Aslam N, Willett K (2004) Functional outcome following internal fixation of intraarticular fractures of the distal humerus (AO type C). Acta Orthop Belg 70(2):118–122
Pajarinen J, Bjorkenheim JM (2002) Operative treatment of type C inter-condylar fractures of the distal humerus: results after a mean follow- up of 2 years in a series of 18 patients. J Shoulder Elbow Surg 11(1):48–52
Patela J, Motwania G, Shaha H, Daveshwar R (2017) Outcome after internal fixation of intraarticular distal humerus (AO type B & C) fractures: preliminary results with anatomical distal humerus LCP system. J Clin Orthop Trauma 8(1):63–67
Lee JK, Choi YS, Sim YS, Choi DC, Han SH (2017) Dual plate fixation on distal third diaphyseal fracture of the humerus. Int Orthop 41(8):1655–1661
Kaiser T, Brunner A, Hohendorff B, Ulmar B, Babst R (2011) Treatment of supra- and intra-articular fractures of the distal humerus with the LCP distal humerus plate: a 2-year follow-up. J Shoulder Elbow Surg 20(2):206–212
Zdravkovic V, Jost B (2018) Rounded data have a high potential for false comparative statistical results as shown with elbow arc of motion. J Shoulder Elbow Surg 27(2):276–228
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: Level I, Therapeutic study
Rights and permissions
About this article
Cite this article
Galal, S., Mattar, Y., Solyman, A.M.E. et al. Locking versus non-locking plates in fixation of extra-articular distal humerus fracture: a randomized controlled study. International Orthopaedics (SICOT) 44, 2761–2767 (2020). https://doi.org/10.1007/s00264-020-04770-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04770-z