Abstract
Purpose
To evaluate the association between imaging and clinical features and visualization scores, as specified by American College of Radiology (ACR) Ultrasound Liver Imaging Reporting and Data System (LI-RADS), on hepatocellular carcinoma (HCC) screening ultrasound examinations.
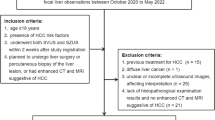
Methods
In this dual-center retrospective study, HCC screening ultrasound reports containing ultrasound elastography measurements (January to September, 2017) were reviewed. Ultrasound point shear wave elastography and 2-dimensional shear wave elastography were used to assess liver stiffness; median shear wave velocity was translated to METAVIR fibrosis scoring, per previously published data. Reports were analyzed for subject age, sex, reason for HCC screening, spleen size, fibrosis scores, and assigned ultrasound visualization scores. Jonckheere–Terpstra trend and Kendall’s tau-b coefficient analyses were performed.
Results
714 subjects (mean age 55; 51% male, 49% female) were included. 308 (43%) subjects had clinically declared cirrhosis; 406 (57%) did not. Majority (535, 75%) of exams were adequate (Visualization Score A), 156 (22%) moderately limited (Visualization Score B), and 23 (3%) severely limited (Visualization Score C). Increasing spleen size and patient age were associated with worsening visualization scores (p < 0.001). Suboptimal visualization was also associated with clinically significant fibrosis (≥ F2) by elastography (Kendall’s tau-b = 0.181, p < 0.001) and clinically declared cirrhosis (Kendall’s tau-b = 0.433, p < 0.001). There was no association with patient sex.
Conclusion
Using ACR Ultrasound LI-RADS visualization score assessment, majority (75%) of HCC screening exams were diagnostically adequate, and only 3% were severely limited. Sonoelastographic diagnosis of clinically significant fibrosis, as well as clinical cirrhosis, increased patient age, and spleen size, were associated with greater diagnostic limitations.
Similar content being viewed by others
References
Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, Allen C, et al. The Burden of Primary Liver Cancer and Underlying Etiologies From 1990 to 2015 at the Global, Regional, and National Level. JAMA Oncol. 2017;98121(12):1683–91.
Tang A, Hallouch O, Chernyak V, Kamaya A, Sirlin CB. Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol. Springer US; 2017;1–13.
Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MAM, et al. Meta-analysis: Surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30(1):37–47.
Morgan TA, Maturen KE, Dahiya N, Sun MRM, Kamaya A. US LI-RADS: ultrasound liver imaging reporting and data system for screening and surveillance of hepatocellular carcinoma. Abdom Radiol. Springer US; 2017;1–15.
Heimbach J, Kulik LM, Finn R, Sirlin CB, Abecassis M, Roberts LR, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–380. https://doi.org/10.1002/hep.29086.
Llovet JM, Ducreux M, Lencioni R, Di Bisceglie AM, Galle PR, Dufour JF, et al. EASL-EORTC Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. European Association for the Study of the Liver; 2012;56(4):908–43.
Barr RG, Ferraioli G, Palmeri ML, Goodman ZD, Garcia-Tsao G, Rubin J, et al. Elastography Assessment of Liver Fibrosis: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2015;276(3).
Simmons O, Fetzer DT, Yokoo T, Marrero JA, Yopp A, Kono Y, et al. Predictors of adequate ultrasound quality for hepatocellular carcinoma surveillance in patients with cirrhosis. Aliment Pharmacol Ther. 2017;45(1):169–77.
Fetzer DT, Rodgers SK, Harris AC, Kono Y, Wasnik AP, Kamaya A, et al. Screening and Surveillance of Hepatocellular Carcinoma: An Introduction to Ultrasound Liver Imaging Reporting and Data System. Radiol Clin North Am. Elsevier Inc; 2017;55(6):1197–209.
American College of Radiology. ACR US LI-RADS Core Document [Internet]. 2017 [cited 2018 May 28]. Available from: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/Ultrasound-LI-RADS-v2017
ACR. ACR – AIUM – SPR – SRU Practice Parameter for the Performance of an Ultrasound Examination of the Abdomen and/or Retroperitoneum [Internet]. [cited 2018 Jul 5]. p. 1–8. Available from: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/us-abd-retro.pdf?la=en
Friedrich-Rust M, Nierhoff J, Lupsor M, Sporea I, Fierbinteanu-Braticevici C, Strobel D, et al. Performance of Acoustic Radiation Force Impulse imaging for the staging of liver fibrosis: A pooled meta-analysis. J Viral Hepat. 2012;19(2):212–9.
Sigrist RMS, Liau J, Kaffas A El, Chammas MC, Willmann JK. Ultrasound elastography: Review of techniques and clinical applications. Theranostics. 2017;7(5):1303–29.
Winkler NS, Raza S, Mackesy M, Birdwell RL. Breast density: clinical implications and assessment methods. Radiographics. 2015;35(2):316–24.
Freer PE. Mammographic Breast Density: Impact on Breast Cancer Risk and Implications for Screening. RadioGraphics. Radiological Society of North America; 2015 Mar 12;35(2):302–15.
Colli A, Fraquelli M, Casazza G, Massironi S, Colucci A, Conte D, et al. Accuracy of Ultrasonography, Spiral CT, Magnetic Resonance, and Alpha-Fetoprotein in Diagnosing Hepatocellular Carcinoma: A Systematic Review. CME. Am J Gastroenterol. 2006 Mar;101(3):513–23.
Lee YJ, Lee JM, Lee JS, Lee HY, Park BH, Kim YH, et al. Hepatocellular Carcinoma: Diagnostic Performance of Multidetector CT and MR Imaging—A Systematic Review and Meta-Analysis. Radiology. Radiological Society of North America; 2015 Apr 5;275(1):97–109.
Tzartzeva K, Obi J, Rich NE, Parikh ND, Marrero JA, Yopp A, et al. Surveillance Imaging and Alpha Fetoprotein for Early Detection of Hepatocellular Carcinoma in Patients With Cirrhosis: A Meta-analysis. Gastroenterology. The American Gastroenterological Association; 2018;
Kennedy P, Wagner M, Castéra L, Hong CW, Johnson CL, Sirlin CB, et al. Quantitative Elastography Methods in Liver Disease: Current Evidence and Future Directions. Radiology. 2018;286(3):738–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
IRB approval was obtained, and the requirement for written consent was waived.
Rights and permissions
About this article
Cite this article
Choi, H.H., Perez, M.G., Millet, J.D. et al. Association of advanced hepatic fibrosis and sonographic visualization score: a dual-center study using ACR US LI-RADS. Abdom Radiol 44, 1415–1422 (2019). https://doi.org/10.1007/s00261-018-1862-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1862-z