Abstract
Purpose
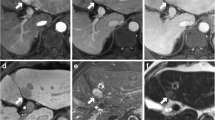
To compare the added values of hepatobiliary phase (HBP) MRI and contrast-enhanced ultrasound (CEUS) in addition to inconclusive extracellular gadolinium-based contrast-enhanced MRI (CE-MRI) to characterize benign hepatocellular tumors (BHT).
Methods
Eighty-three BHT-46 focal nodular hyperplasia (FNH) and 37 hepatocellular adenomas (HCA)-with inconclusive CE-MRI in 54 patients (43 women and 11 men, mean age 42 years old ± 14.8) were retrospectively analyzed. All patients underwent both HBP-MRI and CEUS. Two radiologists independently reviewed 2 sets of images, SET-1: CE-MRI and HBP-MRI; SET-2: CE-MRI and CEUS, and classified lesions as “definite FNH,” “possible FNH,” or “definitely not FNH.” Sensitivity (Se) and specificity (Spe) were compared between the two sets; subgroup analyses according to the lesion’s size were performed.
Results
Regardless of lesion size, the respective Se and Spe of both datasets were not statistically different (95.7 and 100% vs. 76.1 and 94.6% for set-1 and -2 respectively; p = 0.18). For lesions larger than 35 mm, although both sets had similar specificity (100%), sensitivity was higher for SET-1 (100% vs. 40%); p = 0.04. Tumor classifications using SET-1 and SET-2 could have changed patient management in 35/54 (64.8%) and 33/54 (61.1%) of all patients, respectively.
Conclusions
HBP-MRI or CEUS should be performed after an inconclusive CE-MRI. Both can change patient management by avoiding unnecessary biopsy or surveillance. The use of HBP-MRI should be advocated over CEUS in larger (>35 mm) lesions.



Similar content being viewed by others
References
Mathieu D, Rahmouni A, Anglade MC, et al. (1991) Focal nodular hyperplasia of the liver: assessment with contrast-enhanced TurboFLASH MR imaging. Radiology 180:25–30
Nault JC, Bioulac-Sage P, Zucman-Rossi J (2013) Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology 144:888–902
Laumonier H, Bioulac-Sage P, Laurent C, et al. (2008) Hepatocellular adenomas: magnetic resonance imaging features as a function of molecular pathological classification. Hepatology 48:808–818
Navarro AP, Gomez D, Lamb CM, Brooks A, Cameron IC (2014) Focal nodular hyperplasia: a review of current indications for and outcomes of hepatic resection. HPB (Oxford) 16:503–511
De Carlis L, Pirotta V, Rondinara GF, et al. (1997) Hepatic adenoma and focal nodular hyperplasia: diagnosis and criteria for treatment. Liver Transpl Surg 3:160–165
Dokmak S, Paradis V, Vilgrain V, et al. (2009) A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology 137:1698–1705
Cherqui D (2008) Clinical management of benign liver cell tumors. Gastroenterol Clin Biol 32:310–313 (quiz 293, 314)
Bioulac-Sage P, Laumonier H, Couchy G, et al. (2009) Hepatocellular adenoma management and phenotypic classification: the Bordeaux experience. Hepatology 50:481–489
Bieze M, van den Esschert JW, Nio CY, et al. (2012) Diagnostic accuracy of MRI in differentiating hepatocellular adenoma from focal nodular hyperplasia: prospective study of the additional value of gadoxetate disodium. AJR Am J Roentgenol 199:26–34
Ronot M, Vilgrain V (2014) Imaging of benign hepatocellular lesions: Current concepts and recent updates. Clin Res Hepatol Gastroenterol 38:681–688
Ferlicot S, Kobeiter H, Tran Van Nhieu J, et al. (2004) MRI of atypical focal nodular hyperplasia of the liver: radiology-pathology correlation. AJR Am J Roentgenol 182:1227–1231
Grazioli L, Morana G, Federle MP, et al. (2001) Focal nodular hyperplasia: morphologic and functional information from MR imaging with gadobenate dimeglumine. Radiology 221:731–739
Vilgrain V, Flejou JF, Arrive L, et al. (1992) Focal nodular hyperplasia of the liver: MR imaging and pathologic correlation in 37 patients. Radiology 184:699–703
Piccinino F, Sagnelli E, Pasquale G, Giusti G (1986) Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 2:165–173
Wang W, Chen LD, Lu MD, et al. (2013) Contrast-enhanced ultrasound features of histologically proven focal nodular hyperplasia: diagnostic performance compared with contrast-enhanced CT. Eur Radiol 23:2546–2554
Zhu XL, Chen P, Guo H, et al. (2011) Contrast-enhanced ultrasound for the diagnosis of hepatic adenoma. J Int Med Res 39:920–928
Seitz K, Bernatik T, Strobel D, et al. (2010) Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI–a prospective comparison in 269 patients. Ultraschall Med 31:492–499
Kim TK, Jang HJ, Burns PN, Murphy-Lavallee J, Wilson SR (2008) Focal nodular hyperplasia and hepatic adenoma: differentiation with low-mechanical-index contrast-enhanced sonography. AJR Am J Roentgenol 190:58–66
Grazioli L, Morana G, Kirchin MA, Schneider G (2005) Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study. Radiology 236:166–177
Suh CH, Kim KW, Kim GY, et al. (2015) The diagnostic value of Gd-EOB-DTPA-MRI for the diagnosis of focal nodular hyperplasia: a systematic review and meta-analysis. Eur Radiol 25:950–960
McInnes MD, Hibbert RM, Inacio JR, Schieda N (2015) Focal nodular hyperplasia and hepatocellular adenoma: accuracy of gadoxetic acid-enhanced MR imaging-a systematic review. Radiology. doi:10.1148/radiol.2015142986:142986
Grazioli L, Bondioni MP, Faccioli N, et al. (2010) Solid focal liver lesions: dynamic and late enhancement patterns with the dual phase contrast agent gadobenate dimeglumine. J Gastrointest Cancer 41:221–232
Kim HJ, Kim BS, Kim MJ, et al. (2013) Enhancement of the liver and pancreas in the hepatic arterial dominant phase: comparison of hepatocyte-specific MRI contrast agents, gadoxetic acid and gadobenate dimeglumine, on 3 and 1.5 Tesla MRI in the same patient. J Magn Reson Imaging 37:903–908
Yoneda N, Matsui O, Kitao A, et al. (2012) Hepatocyte transporter expression in FNH and FNH-like nodule: correlation with signal intensity on gadoxetic acid enhanced magnetic resonance images. Jpn J Radiol 30:499–508
Roche V, Pigneur F, Tselikas L, et al. (2015) Differentiation of focal nodular hyperplasia from hepatocellular adenomas with low-mechanical-index contrast-enhanced sonography (CEUS): effect of size on diagnostic confidence. Eur Radiol 25:186–195
Fabre A, Audet P, Vilgrain V, et al. (2002) Histologic scoring of liver biopsy in focal nodular hyperplasia with atypical presentation. Hepatology 35:414–420
Roux M, Pigneur F, Calderaro J, et al. (2015) Differentiation of focal nodular hyperplasia from hepatocellular adenoma: Role of the quantitative analysis of gadobenate dimeglumine-enhanced hepatobiliary phase MRI. J Magn Reson Imaging. doi:10.1002/jmri.24897
Cherqui D, Rahmouni A, Charlotte F, et al. (1995) Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology 22:1674–1681
Vilgrain V (2006) Focal nodular hyperplasia. Eur J Radiol 58:236–245
Fleiss JL, Levin B, Paik MC (2013) Statistical methods for rates and proportions. New York: Wiley
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Kim S, Lee W (2014) Does McNemar’s test compare the sensitivities and specificities of two diagnostic tests? Stat Methods Med Res. doi:10.1177/0962280214541852
Bertin C, Egels S, Wagner M, et al. (2014) Contrast-enhanced ultrasound of focal nodular hyperplasia: a matter of size. Eur Radiol 24:2561–2571
Westwood M, Joore M, Grutters J, et al. (2013) Contrast-enhanced ultrasound using SonoVue(R) (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Assess 17:1–243
Gupta RT, Iseman CM, Leyendecker JR, et al. (2012) Diagnosis of focal nodular hyperplasia with MRI: multicenter retrospective study comparing gadobenate dimeglumine to gadoxetate disodium. AJR Am J Roentgenol 199:35–43
Dahlqvist Leinhard O, Dahlstrom N, Kihlberg J, et al. (2012) Quantifying differences in hepatic uptake of the liver specific contrast agents Gd-EOB-DTPA and Gd-BOPTA: a pilot study. Eur Radiol 22:642–653
Zech CJ, Bartolozzi C, Bioulac-Sage P, et al. (2013) Consensus report of the Fifth International Forum for Liver MRI. AJR Am J Roentgenol 201:97–107
D’Onofrio M, Crosara S, De Robertis R, et al. (2014) Malignant focal liver lesions at contrast-enhanced ultrasonography and magnetic resonance with hepatospecific contrast agent. Ultrasound 22:91–98
Agarwal S, Fuentes-Orrego JM, Arnason T, et al. (2014) Inflammatory hepatocellular adenomas can mimic focal nodular hyperplasia on gadoxetic acid-enhanced MRI. AJR Am J Roentgenol 203:W408–W414
Ramalho J, Castillo M, AlObaidy M, et al. (2015) High Signal Intensity in Globus Pallidus and Dentate Nucleus on Unenhanced T1-weighted MR Images: Evaluation of Two Linear Gadolinium-based Contrast Agents. Radiology 276:836–844
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Research involving Human Participants (adults) was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards (IRB approved).
Informed consent
For this type of study formal consent is not required and was waived by IRB.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tselikas, L., Pigneur, F., Roux, M. et al. Impact of hepatobiliary phase liver MRI versus Contrast-Enhanced Ultrasound after an inconclusive extracellular gadolinium-based contrast-enhanced MRI for the diagnosis of benign hepatocellular tumors. Abdom Radiol 42, 825–832 (2017). https://doi.org/10.1007/s00261-016-0921-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0921-6