Abstract
Purpose
Increased blood glucose level (BGL) has been reported to cause alterations of FDG uptake in the brain that mimic Alzheimer’s disease (AD), even within the "acceptable" range ≤ 160 mg/dl. The aim of this study was (i) to confirm this in a large sample of well-characterized normal control (NC) subjects, and (ii) to analyze its impact on the prediction of AD dementia (ADD) in mild cognitive impairment (MCI).
Methods
The study included NCs from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) that were cognitively stable for ≥36 months after PET (n = 87, 74.2 ± 5.3 y), and ADNI MCIs with ≥36 months follow-up if not progressed to ADD earlier (n = 323, 71.1 ± 7.1 y). Seventy-three of the MCIs had progressed to ADD within 36 months. In the NCs, parenchyma-scaled FDG uptake was tested for clusters of correlation with BGL on the family-wise, error-corrected 5% level. In the MCIs, ROC analysis was used to assess the power of FDG uptake in a predefined AD-typical region for prediction of ADD. ROC analysis was repeated after correcting mean FDG uptake in the AD-typical region for BGL based on linear regression in the NCs.
Results
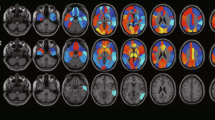
In the NCs, BGL (59–149 mg/dl) was negatively correlated with FDG uptake in a cluster comprising the occipital cortex and precuneus but sparing the posterior cingulate, independent of amyloid-β and ApoE4 status. In the MCIs, FDG uptake in the AD-typical region provided an area of 0.804 under the ROC curve for prediction of ADD. Correcting FDG uptake in the AD-typical region for BGL (55–189 mg/dl) did not change predictive performance (area = 0.808, p = 0.311).
Conclusions
Increasing BGL is associated with relative reduction of FDG uptake in the posterior cortex even in the "acceptable" range ≤ 160 mg/dl. The BGL-associated pattern is similar to the typical AD pattern, but not identical. BGL-associated variability of regional FDG uptake has no relevant impact on the power of FDG PET for prediction of MCI-to-ADD progression.



Similar content being viewed by others
References
Garibotto V, Herholz K, Boccardi M, Picco A, Varrone A, Nordberg A, et al. Clinical validity of brain fluorodeoxyglucose positron emission tomography as a biomarker for Alzheimer's disease in the context of a structured 5-phase development framework. Neurobiol Aging. 2017;52:183–95. https://doi.org/10.1016/j.neurobiolaging.2016.03.033.
Minoshima S, Giordani B, Berent S, Frey KA, Foster NL, Kuhl DE. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer's disease. Ann Neurol. 1997;42:85–94. https://doi.org/10.1002/ana.410420114.
Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R, et al. Physical basis of cognitive alterations in Alzheimer's disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol. 1991;30:572–80. https://doi.org/10.1002/ana.410300410.
Kljajevic V, Grothe MJ, Ewers M, Teipel S. Alzheimer's disease neuroimaging I. Distinct pattern of hypometabolism and atrophy in preclinical and predementia Alzheimer's disease. Neurobiol Aging. 2014;35:1973–81. https://doi.org/10.1016/j.neurobiolaging.2014.04.006.
Varrone A, Asenbaum S, Vander Borght T, Booij J, Nobili F, Nagren K, et al. EANM procedure guidelines for PET brain imaging using [18F]FDG, version 2. Eur J Nucl Med Mol Imaging. 2009;36:2103–10. https://doi.org/10.1007/s00259-009-1264-0.
Ishibashi K, Kawasaki K, Ishiwata K, Ishii K. Reduced uptake of 18F-FDG and 15O-H2O in Alzheimer's disease-related regions after glucose loading. J Cereb Blood Flow Metab. 2015;35:1380–5. https://doi.org/10.1038/jcbfm.2015.127.
Ishibashi K, Onishi A, Fujiwara Y, Ishiwata K, Ishii K. Relationship between Alzheimer disease-like pattern of 18F-FDG and fasting plasma glucose levels in cognitively normal volunteers. J Nucl Med. 2015;56:229–33. https://doi.org/10.2967/jnumed.114.150045.
Ishibashi K, Onishi A, Fujiwara Y, Ishiwata K, Ishii K. Plasma glucose levels affect cerebral 18F-FDG distribution in cognitively normal subjects with diabetes. Clin Nucl Med. 2016;41:e274–80. https://doi.org/10.1097/RLU.0000000000001147.
Ishibashi K, Wagatsuma K, Ishiwata K, Ishii K. Alteration of the regional cerebral glucose metabolism in healthy subjects by glucose loading. Hum Brain Mapp. 2016;37:2823–32. https://doi.org/10.1002/hbm.23210.
Kawasaki K, Ishii K, Saito Y, Oda K, Kimura Y, Ishiwata K. Influence of mild hyperglycemia on cerebral FDG distribution patterns calculated by statistical parametric mapping. Ann Nucl Med. 2008;22:191–200. https://doi.org/10.1007/s12149-007-0099-7.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Clark CM, Aisen PS, Petersen RC, et al. Cerebrospinal fluid biomarker signature in Alzheimer's disease neuroimaging initiative subjects. Ann Neurol. 2009;65:403–13. https://doi.org/10.1002/ana.21610.
Landau SM, Lu M, Joshi AD, Pontecorvo M, Mintun MA, Trojanowski JQ, et al. Comparing positron emission tomography imaging and cerebrospinal fluid measurements of beta-amyloid. Ann Neurol. 2013;74:826–36. https://doi.org/10.1002/ana.23908.
Lange C, Suppa P, Frings L, Brenner W, Spies L, Buchert R. Optimization of statistical single subject analysis of brain FDG PET for the prognosis of mild cognitive impairment-to-Alzheimer's disease conversion. J Alzheimers Dis. 2016;49:945–59. https://doi.org/10.3233/JAD-150814.
Reiman EM, Chen K, Alexander GE, Caselli RJ, Bandy D, Osborne D, et al. Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer's dementia. Proc Natl Acad Sci U S A. 2004;101:284–9. https://doi.org/10.1073/pnas.2635903100.
Joshi A, Koeppe RA, Fessler JA. Reducing between scanner differences in multi-center PET studies. NeuroImage. 2009;46:154–9. https://doi.org/10.1016/j.neuroimage.2009.01.057.
Jagust WJ, Bandy D, Chen K, Foster NL, Landau SM, Mathis CA, et al. The Alzheimer's disease neuroimaging initiative positron emission tomography core. Alzheimers Dement. 2010;6:221–9. https://doi.org/10.1016/j.jalz.2010.03.003.
Hogstrom LJ, Westlye LT, Walhovd KB, Fjell AM. The structure of the cerebral cortex across adult life: age-related patterns of surface area, thickness, and gyrification. Cereb Cortex. 2013;23:2521–30. https://doi.org/10.1093/cercor/bhs231.
Acknowledgements
Data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI; National Institutes of Health grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC; Johnson & Johnson Pharmaceutical Research & Development LLC; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Funding
There was no funding of this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
P.S. and L.S. are employees of jung diagnostics GmbH, Hamburg, Germany. This did not bias their work, as they have no financial interest in the results of this study. All other authors declare that they do not have any potential conflict of interest concerning this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
As the present study was retrospective in nature, formal consent was not required.
Additional information
Data were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI; adni.loni.usc.edu). The investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in the analysis/writing of this report. A complete list of ADNI investigators can be found at http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf
Rights and permissions
About this article
Cite this article
Apostolova, I., Lange, C., Suppa, P. et al. Impact of plasma glucose level on the pattern of brain FDG uptake and the predictive power of FDG PET in mild cognitive impairment. Eur J Nucl Med Mol Imaging 45, 1417–1422 (2018). https://doi.org/10.1007/s00259-018-3985-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3985-4