Abstract
Background
Outpatient, non-emergent upper gastrointestinal (GI) series are frequently requested in children with no surgical history who have nonspecific symptoms such as abdominal pain, failure to thrive and vomiting. The positive yield of an upper GI series in these patients, and, thus, its utility, has not been studied.
Objectives
We evaluated the incidence of positive upper GI findings in children without a history of GI pathology or abdominal surgery in order to identify clinical indications associated with a greater diagnostic yield.
Materials and methods
Findings of upper GI series performed between October 2015 and October 2017 in three institutions in children younger than 18 years of age were retrospectively reviewed. The upper GI series protocol for each institution was also reviewed. Children with a medical or surgical GI history, children with insufficient history in the chart and those with an incomplete upper GI series were excluded from the study. Exam indications, patient demographics and clinical history were obtained from the electronic medical records.
Results
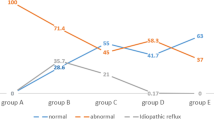
Of 1,267 children who underwent outpatient upper GI series, 720 (median age: 2 years) had no GI history and were included in the study. The most common indications were non-bilious vomiting (62%), reflux symptoms (28%) and abdominal pain (20%). Upper GI series were normal in 605/720 cases (84%), including 25/26 children with reported bilious emesis. Of the 115 positive studies, 78 (68%) showed only gastroesophageal reflux (GER) (median age: 11 months). Of the remaining 37 studies, 19 demonstrated esophageal findings. One case of malrotation without midgut volvulus was identified in a patient who presented with dysphagia and reflux symptoms. Using a multinomial logistic regression model and adjusting for other variables, reflux symptoms and younger patient age were independent predictors of GER on upper GI series (relative risk ratios of 2.2 and 0.9, respectively). Dysphagia and/or foreign body sensation and older patient age were independent predictors of the presence of esophageal findings (relative risk ratios of 3.3 and 1.1, respectively).
Conclusion
The yield of routine upper GI series in children with nonspecific symptoms, such as abdominal pain and vomiting, and no surgical history is low. Diagnostic yield was improved in older children and in those complaining of dysphagia and/or foreign body sensation. Routine upper GI series should be avoided in clinically well children with symptoms only of uncomplicated GER and no significant GI history. In children with a history of dysphagia and/or foreign body sensation, an esophagram/barium swallow can suffice.
Similar content being viewed by others
References
Stanescu AL, Liszewski MC, Lee EY, Phillips GS (2017) Neonatal gastrointestinal e0mergencies: step-by-step approach. Radiol Clin N Am 55:717–739
Cuenca AG, Reddy SV, Dickie B et al (2011) The usefulness of the upper gastrointestinal series in the pediatric patient before anti-reflux procedure or gastrostomy tube placement. J Surg Res 170:247–252
Graziano K, Islam S, Dasgupta R et al (2015) Asymptomatic malrotation: diagnosis and surgical management: an American pediatric surgical association outcomes and evidence based practice committee systematic review. J Pediatr Surg 50:1783–1790
Kumar D, Brereton RJ, Spitz L, Hall CM (1988) Gastro-oesophageal reflux and intestinal malrotation in children. Br J Surg 75:533–535
Leonidas JC (1984) Gastroesophageal reflux in infants: role of the upper gastrointestinal series. AJR Am J Roentgenol 143:1350–1351
Macharia EW (2012) Comparison of upper gastrointestinal contrast studies and pH/impedance tests for the diagnosis of childhood gastro-oesophageal reflux. Pediatr Radiol 42:946–951
Ruigomez A, Wallander MA, Lundborg P et al (2010) Gastroesophageal reflux disease in children and adolescents in primary care. Scand J Gastroenterol 45:139–146
Applegate KE, Anderson JM, Klatte EC (2006) Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics 26:1485–1500
Sizemore AW, Rabbani KZ, Ladd A, Applegate KE (2008) Diagnostic performance of the upper gastrointestinal series in the evaluation of children with clinically suspected malrotation. Pediatr Radiol 38:518–528
Simanovsky N, Buonomo C, Nurko S (2002) The infant with chronic vomiting: the value of the upper GI series. Pediatr Radiol 32:549–550
Acker SN, Trinh BB, Partrick DA et al (2016) Is routine upper gastrointestinal contrast study necessary prior to laparoscopic gastrostomy tube placement in children? Eur J Pediatr Surg 26:29–33
Abbas PI, Naik-Mathuria BJ, Akinkuotu AC, Pimpalwar AP (2015) Routine gastrostomy tube placement in children: does preoperative screening upper gastrointestinal contrast study alter the operative plan? J Pediatr Surg 50:715–717
Gonzalez KW, Dalton BG, Boda S et al (2015) Utility of preoperative upper gastrointestinal series in laparoscopic gastrostomy tube placement. J Laparoendosc Adv Surg Tech A 25:1040–1043
Larson-Nath CM, Wagner AJ, Goday PS (2014) Use of upper gastrointestinal series before gastrostomy tube placement. J Pediatr Gastroenterol Nutr 58:613–615
Atkin KL, Chowdhury MM, Bartlett M (2014) Incidence of clinically silent malrotation detected on barium swallow examination in children. J Med Imaging Radiat Oncol 58:298–302
Kapfer SA, Rappold JF (2004) Intestinal malrotation-not just the pediatric surgeon's problem. J Am Coll Surg 199:628–635
Emigh B, Gordon CL, Connolly BL et al (2013) Effective dose estimation for pediatric upper gastrointestinal examinations using an anthropomorphic phantom set and metal oxide semiconductor field-effect transistor (MOSFET) technology. Pediatr Radiol 43:1108–1116
Walker MM, Powell N, Talley NJ (2014) Atopy and the gastrointestinal tract--a review of a common association in unexplained gastrointestinal disease. Expert Rev Gastroenterol Hepatol 8:289–299
Czinn SJ, Blanchard S (2013) Gastroesophageal reflux disease in neonates and infants : when and how to treat. Paediatr Drugs 15:19–27
Raske ME, Dempsey ME, Dillman JR et al (2015) ACR appropriateness criteria vomiting in infants up to 3 months of age. J Am Coll Radiol 12:915–922
Lampl B, Levin TL, Berdon WE, Cowles RA (2009) Malrotation and midgut volvulus: a historical review and current controversies in diagnosis and management. Pediatr Radiol 39:359–366
Levitt B, Richter JE (2007) Dysphagia lusoria: a comprehensive review. Dis Esophagus 20:455–460
Menchise AN, Mezoff EA, Lin TK et al (2016) Medical management of duodenum inversum presenting with partial proximal intestinal obstruction in a pediatric patient. J Pediatr Gastroenterol Nutr 62:e64–e65
Acknowledgements
We would like to thank Dr. Kenny Ye for statistical consultation and Oleg Kaplun for assistance with computer searches.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Goldman-Yassen, A.E., Gross, J., Novak, I. et al. Identification of clinical parameters to increase the diagnostic yield of the non-emergent upper gastrointestinal series in pediatric outpatients. Pediatr Radiol 49, 162–167 (2019). https://doi.org/10.1007/s00247-018-4286-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4286-6