Abstract
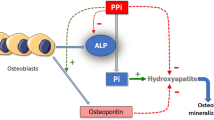
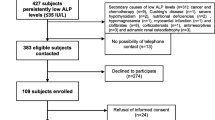
Low serum alkaline phosphatase (sALP)—hypophosphatasemia—is a characteristic of hypophosphatasia (HPP), but related to several clinical conditions. Here, we evaluated the frequency, persistency and the etiology of hypophosphatasemia in children. In retrospective analyses of sALP measurements from children, evaluated according to in-house constructed age- and sex-specific reference ranges, patients with no normal sALP measurement (Unresolved hypophosphatasemia) were invited for reanalysis. Prospectively, ALP substrates, pyridoxal-5-phosphate (PLP), and phosphoethanolamine (PEA) were measured in patients with persistent hypophosphatasemia. Radiographs and ALPL gene sequencing for HPP were performed to the cases with elevated PEA and/or PLP. From 130,340 sALP measurements of 93,162 patients, hypophosphatasemia was detected in 1404 samples from 867 patients (0.9%). Among them, 745 had at least one normal sALP values in laboratory records, grouped as transient hypophosphatasemia. 75 out of 122 patients with unresolved hypophosphatasemia could be reanalyzed for sALP, of whom PLP and PEA measurements were required in 37 due to persistent hypophosphatasemia. Both PEA and PLP were elevated in 4 patients, and ALPL gene analysis showed heterozygous mutations in 3 patients and homozygous in 1 patient. Elevated PEA with normal PLP were detected in 3 patients, and one had a heterozygous ALPL mutation. Anemia was the most common diagnosis, and upper respiratory tract infections and chronic diseases were more common in transient and unresolved hypophosphatasemia, respectively. In conclusion, reflected persistent hypophosphatasemia frequency was 1/1552 (0.06%) in this large pediatric cohort and, ALPL gene mutations were detected in 13.5% (5/37) of the studied cases. Although biochemical hypophosphatasemia is not uncommon, clinically significant HPP is rare.


Similar content being viewed by others
Abbreviations
- ALP:
-
Alkaline phosphatase
- TNSALP:
-
Tissue-nonspecific ALP, ALPL gene
- HPP:
-
Hypophosphatasia
- PPi:
-
Inorganic pyrophosphate
- PLP:
-
Pyridoxal-5-phosphate
- PEA:
-
Phosphoethanolamine
- Ca:
-
Calcium
- PO4 :
-
Phosphate
- PTH:
-
Parathyroid hormone
- Cre:
-
Creatinine
- S:
-
Serum
- U:
-
Urine
References
Millán JL (2006) Mammalian alkaline phosphatases: from biology to applications in medicine and biotechnology. Wiley, Weinheim, pp 1–322
Turan S, Topcu B, Gökçe İ, Güran T, Atay Z, Omar Aİ et al (2011) Serum alkaline phosphatase levels in healthy children and evaluation of alkaline phosphatase z-scores in different types of rickets. J Clin Res Pediatr Endocrinol 3:7–11
McKiernan FE, Shrestha LK, Berg RL, Fuehrer J (2014) Acute hypophosphatasemia. Osteoporos Int 25:519–523
Lum G (1995) Significance of low serum alkaline phosphatase activity in a predominantly adult male population. Clin Chem 41:515–518
Whyte MP (1994) Hypophosphatasia and the role of alkaline phosphatase in skeletal mineralization. Endocr Rev 15:439–461
Mornet E (2007) Hypophosphatasia. Orphanet J Rare Dis 2:40
Whyte MP, Zhang F, Wenkert D, McAlister WH, Mack KE, Benigno MC et al (2015) Hypophosphatasia: validation and expansion of the clinical nosology for children from 25 years experience with 173 pediatric patients. Bone 75:229–239
Baumgartner-Sigl S, Haberlandt E, Mumm S, Scholl-Beurgi S, Sergi C, Ryan L, et al (2007) Pyridoxine-responsive seizures as the first symptom of infantile hypophosphatasia caused by two novel missense mutations (c.677T%3eC, p.M226T; c.1112C%3eT, p.T371I) of the tissue-nonspecific alkaline phosphatase gene. Bone 40:1655–1661.
Leung EC, Mhanni AA, Reed M, Whyte MP, Landy H, Greenberg CR (2013) Outcome of perinatal hypophosphatasia in Manitoba Mennonites: a retrospective cohort analysis. JIMD Rep 11:73–78
Fauvert D, Brun-Heath I, Lia-Baldini AS, Bellazi L, Taillandier A, Serre JL et al (2009) Mild forms of hypophosphatasia mostly result from dominant negative effect of severe alleles or from compound heterozygosity for severe and moderate alleles. BMC Med Genet 10:51
Fallon MD, Teitelbaum SL, Weinstein RS, Goldfischer S, Brown DM, Whyte MP (1984) Hypophosphatasia: clinicopathologic comparison of the infantile, childhood, and adult forms. Medicine 63:12–24
Whyte MP (2013) In: Thakker RV, Whyte MP, Eisman J, Igarashi T (eds) Genetics of bone biology and skeletal disease, 1st edn. Academic Press, New York, pp 337–360
Chodirker BN, Evans JA, Seargeant LE, Cheang MS, Greenberg CR (1990) Hyperphosphatemia in infantile hypophosphatasia: implications forcarrier diagnosis and screening. Am J Hum Genet 46:280–285
Whyte MP, Greenberg CR, Salman NJ, Bober MB, McAlister WH, Wenkert D et al (2012) Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med 366:904–913
Silvent J, Gasse B, Mornet E, Sire JY (2014) Molecular evolution of the tissue-nonspecific alkaline phosphatase allows prediction and validation of missense mutations responsible for hypophosphatasia. J Biol Chem 289:24168–24179
Haliloglu B, Guran T, Atay Z, Abali S, Mornet E, Bereket A et al (2013) Infantile loss of teeth: odontohypophosphatasia or childhood hypophosphatasia. Eur J Pediatr 172:851–853
McKiernan FE, Berg RL, Fuehrer J (2014) Clinical and radiographic findings in adults with persistent hypophosphatasemia. J Bone Miner Res 29:1651–1660
Deeb A, Elfatih A (2018) Could alerting physicians for low alkaline phosphatase levels be helpful in early diagnosis of hypophosphatasia? J Clin Res Pediatr Endocrinol 10:19–24
Saraff V, Narayanan VK, Lawson AJ, Shaw NJ, Preece MA, Högler W (2016) A Diagnostic algorithm for children with low alkaline phosphatase activities: lessons learned from laboratory screening for hypophosphatasia. J Pediatr 172(181–186):e1
McKiernan FE, Dong J, Berg RL, Scotty E, Mundt P, Larson L et al (2017) Mutational and biochemical findings in adults with persistent hypophosphatasemia. Osteoporos Int 28:2343–2348
Acknowledgements
We are thankful to Alexion Pharmaceuticals, Inc for providing fund for ALP substrates and genetic analysis of the patients.
Funding
Alexion Pharmaceuticals, Inc for providing fund for ALP substrates and genetic analysis of the patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rana Bayramli, Tulay Cevlik, Tulay Guran, Zeynep Atay, Serpil Bas, Goncagul Haklar, Abdullah Bereket, and Serap Turan declared that have no conflict of interest to declare.
Human and Animal Rights and Informed Consent
This study was approved by the Marmara University Medical Faculty Research Ethic Committee (Approval number: 09.2015.330), and the consent forms were obtained from all subjects before participating in to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bayramli, R., Cevlik, T., Guran, T. et al. Clinical Significance of Hypophosphatasemia in Children. Calcif Tissue Int 106, 608–615 (2020). https://doi.org/10.1007/s00223-020-00677-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-020-00677-4